Abstract
Introduction
Marginal ulcer is one of the most common complications after Roux-en-Y gastric bypass and is defined as an ulceration of any depth at or near the gastrojejunal anastomosis. Different risk factors have been advocated to be the causative agent.
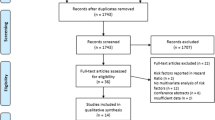
Materials and Methods
The weighted discharges from the Nationwide Inpatient Sample from 2003 to 2011 were used to assess for risk factors to develop marginal ulcer such as Helicobacter pylori infection, chronic nonsteroidal anti-inflammatory use, chronic aspirin use, alcohol dependence, smoking, hypertension, and diabetes mellitus type II.
Results
Chronic nonsteroidal anti-inflammatory drug use was the most significant risk factor for marginal ulcer, followed by Helicobacter pylori infection, obstructive sleep apnea, female sex, smoking, and alcohol dependence in decreasing order. Diabetes mellitus and hypertension were found to slightly increase the risk for marginal ulcer. The use of aspirin was found to be a minor risk factor during univariate analysis but a protective factor during multivariate analysis.
Conclusions
Multiple well-documented single factors are related to the genesis of a marginal ulcer, although it is likely that a combination of risk factors is responsible for this problem. These risk factors should be identified and removed or controlled.


Similar content being viewed by others
Change history
12 October 2020
In the original article, the author names were presented incorrectly; their family names and given names were inverted.
References
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Aminian A, Daigle CR, Romero-Talamas H, et al. Risk prediction of complications of metabolic syndrome before and 6 years after gastric bypass. Surg Obes Relat Dis. 2014;10(4):576–82.
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–14.
Hales CM, Fryar CD, Carroll MD, et al. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013-2016. JAMA. 2018;319(23):2419–29.
Bradley 3rd JF, Ross SW, Christmas AB, et al. Complications of bariatric surgery: the acute care surgeon’s experience. Am J Surg. 2015;210(3):456–61.
El Chaar M, Claros L, Ezeji GC, et al. Improving outcome of bariatric surgery: best practices in an accredited surgical center. Obes Surg. 2014;24(7):1057–63.
Ma IT, Madura 2nd JA. Gastrointestinal complications after bariatric surgery. Gastroenterol Hepatol (N Y). 2015;11(8):526–35.
American Society for Metabolic and Bariatric Surgery. Estimate of Bariatric Surgery Numbers. Available at https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers . Last accessed April 13, 2020.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Robert M, Espalieu P, Pelascini E, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet. 2019;393(10178):1299–309.
El-Hayek K, Timratana P, Shimizu H, et al. Marginal ulcer after Roux-en-Y gastric bypass: what have we really learned? Surg Endosc. 2012;26(10):2789–96.
Huang CS, Forse RA, Jacobson BC, et al. Endoscopic findings and their clinical correlations in patients with symptoms after gastric bypass surgery. Gastrointest Endosc. 2003;58(6):859–66.
Bhayani NH, Oyetunji TA, Chang DC, et al. Predictors of marginal ulcers after laparoscopic Roux-en-Y gastric bypass. J Surg Res. 2012;177(2):224–7.
Rasmussen JJ, Fuller W, Ali MR. Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc. 2007;21(7):1090–4.
Coblijn UK, Goucham AB, Lagarde SM, et al. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24(2):299–309.
Fringeli Y, Worreth M, Langer I. Gastrojejunal anastomosis complications and their management after laparoscopic Roux-en-Y gastric bypass. J Obes. 2015;2015:698425.
Schulman AR, Abougergi MS, Thompson CC. H. pylori as a predictor of marginal ulceration: A nationwide analysis. Obesity (Silver Spring). 2017;25(3):522–6.
Sverden E, Mattsson F, Sonden A, et al. Risk factors for marginal ulcer after gastric bypass surgery for obesity: a population-based cohort study. Ann Surg. 2016;263(4):733–7.
Schreiber H, Ben-Meir A, Sonpal I, et al. Cigarette smoking, but not the presence of H. pylori, is associated with anastomotic ulcers in Roux-en-Y gastric bypass patients. Surg Obes Relat Dis. 2005;1(3):257.
Bhutta HY, Ashley SW. Hypertension and marginal ulceration after gastric bypass. J Surg Res. 2013;185(2):509–10.
Mason EE, Munns JR, Kealey GP, et al. Effect of gastric bypass on gastric secretion. 1977. Surg Obes Relat Dis. 2005;1(2):155–60. discussion 161-2
Sidani S, Akkary E, Bell R. Catastrophic bleeding from a marginal ulcer after gastric bypass. JSLS. 2013;17(1):148–51.
Sapala JA, Wood MH, Sapala MA, et al. Marginal ulcer after gastric bypass: a prospective 3-year study of 173 patients. Obes Surg. 1998;8(5):505–16.
Dallal RM, Bailey LA. Ulcer disease after gastric bypass surgery. Surg Obes Relat Dis. 2006;2(4):455–9.
Hedberg J, Hedenstrom H, Nilsson S, et al. Role of gastric acid in stomal ulcer after gastric bypass. Obes Surg. 2005;15(10):1375–8.
Gribsholt SB, Pedersen AM, Svensson E, et al. Prevalence of self-reported symptoms after gastric bypass surgery for obesity. JAMA Surg. 2016;151(6):504–11.
Subhani M, Rizvon K, Mustacchia P. Endoscopic evaluation of symptomatic patients following bariatric surgery: a literature review. Diagn Ther Endosc. 2012;2012:753472.
Csendes A, Torres J, Burgos AM. Late marginal ulcers after gastric bypass for morbid obesity. Clinical and endoscopic findings and response to treatment. Obes Surg. 2011;21(9):1319–22.
Csendes A, Smok G, Burgos AM, et al. Prospective sequential endoscopic and histologic studies of the gastric pouch in 130 morbidly obese patients submitted to Roux-en-Y gastric bypass. Arq Bras Cir Dig. 2012;25(4):245–9.
Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017;390(10094):613–24.
Wallace JL. Prostaglandins, NSAIDs, and gastric mucosal protection: why doesn't the stomach digest itself? Physiol Rev. 2008;88(4):1547–65.
Chaves LC, Borges IK, Souza MD, et al. Inflammatory disorders associated with Helicobacter pylori in the Roux-en-Y bypass gastric pouch. Arq Bras Cir Dig. 2016;29Suppl 1(Suppl 1):31–4.
Hartin Jr CW, ReMine DS, Lucktong TA. Preoperative bariatric screening and treatment of Helicobacter pylori. Surg Endosc. 2009;23(11):2531–4.
Schirmer B, Erenoglu C, Miller A. Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Obes Surg. 2002;12(5):634–8.
Rawlins L, Rawlins MP, Brown CC, et al. Effect of helicobacter pylori on marginal ulcer and stomal stenosis after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2013;9(5):760–4.
Ashrafian H, Toma T, Rowland SP, et al. Bariatric surgery or non-surgical weight loss for obstructive sleep apnoea? A systematic review and comparison of meta-analyses. Obes Surg. 2015;25(7):1239–50.
Kurata JH, Honda GD, Frankl H. The incidence of duodenal and gastric ulcers in a large health maintenance organization. Am J Public Health. 1985;75(6):625–9.
Kanotra R, Ahmed M, Patel N, et al. Seasonal variations and trends in hospitalization for peptic ulcer disease in the United States: a 12-year analysis of the nationwide inpatient sample. Cureus. 2016;8(10):e854.
Dong WG, Cheng CS, Liu SP, et al. Epidemiology of peptic ulcer disease in Wuhan area of China from 1997 to 2002. World J Gastroenterol. 2004;10(22):3377–9.
Yang X, Guo Y, He J, et al. Estrogen and estrogen receptors in the modulation of gastrointestinal epithelial secretion. Oncotarget. 2017;8(57):97683–92.
Mehaffey JH, LaPar DJ, Clement KC, et al. 10-year outcomes after Roux-en-Y gastric bypass. Ann Surg. 2016;264(1):121–6.
Lent MR, Hayes SM, Wood GC, et al. Smoking and alcohol use in gastric bypass patients. Eat Behav. 2013;14(4):460–3.
Palermo M, Acquafresca PA, Rogula T, et al. Late surgical complications after gastric by-pass: a literature review. Arq Bras Cir Dig. 2015;28(2):139–43.
Azagury DE, Abu Dayyeh BK, Greenwalt IT, et al. Marginal ulceration after Roux-en-Y gastric bypass surgery: characteristics, risk factors, treatment, and outcomes. Endoscopy. 2011;43(11):950–4.
Kular KS, Manchanda N, Rutledge R. Analysis of the five-year outcomes of sleeve gastrectomy and mini gastric bypass: a report from the Indian sub-continent. Obes Surg. 2014;24(10):1724–8.
Scheffel O, Daskalakis M, Weiner RA. Two important criteria for reducing the risk of postoperative ulcers at the gastrojejunostomy site after gastric bypass: patient compliance and type of gastric bypass. Obes Facts. 2011;4(Suppl 1):39–41.
Dittrich L, Schwenninger MV, Dittrich K, et al. Marginal ulcers after laparoscopic Roux-en-Y gastric bypass: analysis of the amount of daily and lifetime smoking on postoperative risk. Surg Obes Relat Dis. 2020;16(3):389–96.
Franke A, Teyssen S, Singer MV. Alcohol-related diseases of the esophagus and stomach. Dig Dis. 2005;23(3–4):204–13.
Kaufman DW, Kelly JP, Wiholm BE, et al. The risk of acute major upper gastrointestinal bleeding among users of aspirin and ibuprofen at various levels of alcohol consumption. Am J Gastroenterol. 1999;94(11):3189–96.
Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12.
Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321(7258):412–9.
Weisman SM, Graham DY. Evaluation of the benefits and risks of low-dose aspirin in the secondary prevention of cardiovascular and cerebrovascular events. Arch Intern Med. 2002;162(19):2197–202.
Uemura N, Sugano K, Hiraishi H, et al. Risk factor profiles, drug usage, and prevalence of aspirin-associated gastroduodenal injuries among high-risk cardiovascular Japanese patients: the results from the MAGIC study. J Gastroenterol. 2014;49(5):814–24.
Pantea M, Negovan A, Voidazan S, et al. Statins and gastroduodenal endoscopic lesions: a case-control study. Medicine (Baltimore). 2018;97(50):e13579.
Badillo R, Schmidt R, Mortensen EM, et al. Statin therapy and gastrointestinal hemorrhage: a retrospective cohort study with propensity score-matching. Pharmacoepidemiol Drug Saf. 2015;24(8):849–57.
Pyke O, Yang J, Cohn T, et al. Marginal ulcer continues to be a major source of morbidity over time following gastric bypass. Surg Endosc. 2018;
Stulberg JJ, Haut ER. Practical guide to surgical data sets: healthcare cost and utilization project National Inpatient Sample (NIS). JAMA Surg. 2018;153(6):586–7.
Acknowledgments
We would like to thank Nicole L. Duarte for providing language help and proofreading the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
For this type of study, formal consent is not required. An IRB official waiver of ethical approval was granted.
Consent to Participate
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodrigo, DC., Jill, S., Daniel, M. et al. Which Factors Correlate with Marginal Ulcer After Surgery for Obesity?. OBES SURG 30, 4821–4827 (2020). https://doi.org/10.1007/s11695-020-04960-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04960-z