Abstract
Background
Smoking has been associated with postoperative complications and mortality in bariatric surgery. The evidence for smoking is based on self-report and medical charts, which can lead to misclassification and miscalculation of the associations. Determination of cotinine can objectively define nicotine exposure. We determined the accuracy of self-reported smoking compared to cotinine measurement in three phases of the bariatric surgery trajectory.
Methods
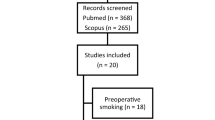
Patients in the phase of screening (screening), on the day of surgery (surgery), and more than 18 months after surgery (follow-up) were consecutively selected. Self-reported smoking was registered and serum cotinine was measured. We evaluated the accuracy of self-reported smoking compared to cotinine, and the level of agreement between self-report and cotinine for each phase.
Results
In total, 715 patients were included. In the screening, surgery, and follow-up group, 25.6%, 18.0%, and 15.5%, respectively, was smoking based on cotinine. The sensitivity of self-reported smoking was 72.5%, 31.0%, and 93.5% in the screening, surgery, and follow-up group, respectively (p < 0.001). The specificity of self-report was > 95% in all groups (p < 0.02). The level of agreement between self-report and cotinine was 0.778, 0.414, and 0.855 for the screening, surgery, and follow-up group, respectively.
Conclusions
Underreporting of smoking occurs before bariatric surgery, mainly on the day of surgery. Future studies on effects of smoking and smoking cessation in bariatric surgery should include methods taking into account the issue of underreporting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is the most effective weight loss therapy for treating morbid obesity. Besides weight loss, it contributes to improvements in comorbidity and reduces mortality [1, 2]. Smoking has been associated with postoperative complications and mortality in bariatric surgery [3,4,5]. Short-term effects of smoking cessation have shown to significantly improve pulmonary function and immune function [6, 7], and smoking cessation is thereby likely to decrease postoperative complications [8,9,10]. Therefore, patients are strictly urged to quit smoking before undergoing bariatric surgery.
However, the evidence on the associations between smoking and postoperative complications or influence on weight loss is based on self-report and medical charts [3,4,5, 11,12,13,14,15,16,17]. It may lead to misclassification if patients conceal their smoking habits. This is a common problem in studies [18, 19]. Studies on the relationship between self-reported smoking status and objectively measured nicotine exposure have shown that misclassification is greater in clinical situations where quitting expectations on part of the health care team influence self-report [18,19,20,21]. Cotinine is the biomarker of choice to objectively define nicotine exposure. It can be measured in serum, urine, and saliva [18, 19, 22].
Therefore, we evaluated the accuracy of self-reported smoking in three groups of patients based on cotinine measurement: patients screened for bariatric surgery, patients on the day of bariatric surgery, and patients more than 18 months after surgery. Additionally, we evaluated whether smoking based on cotinine measurement and self-reported were associated with the occurrence of postoperative complications. We hypothesized that self-reported smoking status may be less accurate in the phase before surgery when patients may be afraid that smoking will contribute to rejection for bariatric surgery compared to smoking status during follow-up after the operation.
Materials and Methods
Setting and Study Population
Between the 4th of January 2017 and the 24th of April 2017, all bariatric surgery patients of a high-volume bariatric center of excellence visiting the laboratory were consecutively screened. As a part of the bariatric care protocol, blood samples are taken from patients at specific time points before and after surgery. Patients in this cohort were urged to quit smoking at least 2 weeks prior to the surgery. They were counseled and were offered support by the general practitioner or smoking cessation department. Three groups were selected: patients in the phase of screening for bariatric surgery (screening), on the day of bariatric surgery (surgery), and patients more than 18 months after bariatric surgery (follow-up). We asked patients whether they were willing to answer questions on smoking behavior and allow us to extract serum from the blood already drawn for clinical management. Exclusion criteria included age under 18 years old, bariatric surgery less than 18 months ago, or missing blood sample.
The local Medical Ethics Committee at former MC Slotervaart approved the study protocol. All patients provided written informed consent before enrolment.
Data Collection
After enrolment all patients were asked to report their current and past nicotine exposure. Afterwards, blood was drawn. Variables that were extracted from medical records included sex, age at time of cotinine measurement, preoperative weight and body mass index, type of bariatric surgery, primary or revisional bariatric surgery, history of abdominal surgery, hypertension, and diabetes mellitus. In the follow-up group, we also collected information on time after surgery, percentage total weight loss, proton pump inhibitor use, and postoperative presence of hypertension and diabetes.
Self-Reported Smoking and Smoking According to Cotinine
Current smoking was defined as smoking at least once during the past 2 days, because of the half-life of cotinine [19, 22,23,24,25].
Self-Report
Patients filled out a written questionnaire questioning whether they had smoked (ever), had used nicotine replacing products, or were exposed to secondhand smoking during the last 48 h. Additionally, (former) smokers answered when they had smoked the last one.
Cotinine
Serum was extracted and samples were stored at − 20 °C until analysis. Samples were obtained prospectively and analysis was performed collectively. The standard samples (calibrators and controls) were handled similarly.
Cotinine was extracted with solid-phase extraction (SPE), and quantitation was performed by reversed-phase high-performance liquid chromatography (HPLC) with UV detection [26,27,28,29,30,31]. Cotinine was detected with UV absorbance wavelength set at 259 nm and identified by retention time index (0.38). Internal standard used was 2-phenylimidazole. The quantitation limit of cotinine was 10 ng/ml. The intra-assay and inter-assay coefficients of variation were 8% and 13%, respectively. Cotinine test was defined as positive when cotinine concentration was ≥ 10 ng/ml.
The HPLC-system consisted of Varian ternair pump, Varian ProStar auto sampler, and Varian Prostar Diode Array Detector. The columns used were Bond Elut C2-solid phase extraction columns (3 ml/200 mg) and HPLC analytical column: Inertsil C8; 3.0 × 150 mm, 5 μ. Software used for controlling the HPLC-system and data processing was Galaxie chromatography software.
The technician and the blood samplers were non-smokers. Naturally, there was an interdiction to smoke in the analytical laboratory. The results of the cotinine test were never visible for the attending doctors.
Complications
Complications during the first 30 days after surgery were retrieved from the medical records. We used the Clavien Dindo classification for severity of the complications [32].
Statistical Analysis
Primary, we calculated the sensitivity and specificity of self-reported smoking, also for each group separately (screening, surgery, follow-up). Chi2 test was used to compare sensitivity between the three groups. The degree of agreement between self-report and cotinine measurement was expressed using Cohen’s kappa coefficient, also for each group.
Secondary, patients were grouped in four classification groups combining the self-report and the cotinine test (patients who reported smoking accurately, patients who concealed smoking, patients who correctly reported non-smoking, or those who reported smoking inaccurately). Then, baseline characteristics were compared using chi2 test, one-way ANOVA, or Kruskal Wallis test, in case of categorical variables, normal distributed variables, or non-normal distributed data respectively. Finally, in case of p value < 0.200, group differences were tested separately using chi2 test, unpaired T test, or Mann-Whitney U test if applicable. We calculated cotinine concentrations per classification group and described exposure to secondhand smoking and nicotine replacement products.
Finally, the associations between smoking, self-reported or defined by cotinine measurement, and complications during the first 30 days after bariatric surgery were explored using univariable logistic regression. We adjusted for possible confounding, by adding variables with p value < 0.400 after univariable logistic regression to the model.
Data analysis was performed using IBM SPSS Statistics software package for Windows version 22 (Chicago, Illinois).
Results
During the screening period, a total of 742 patients was eligible for the study. Twenty-seven patients were excluded; 13 in the screening, nine in the surgery, and five patients in the follow-up group. Patient characteristics are described in Table 1. Median time after surgery of follow-up group was 2.9 years (interquartile range 2.0–3.8). Mean total weight loss was 30.5% (standard deviation 9.0). Postoperative, 43 (21.5%) patients had hypertension, 11 (5.5%) diabetes mellitus 2, and 62 (31.0%) patients used proton pump inhibitors.
Smoking: Self-Reported and Based on Cotinine Measurement
In Table 2, self-reported smoking, positive cotinine (≥ 10 ng/ml), cotinine concentration, sensitivity, specificity and Cohen’s kappa coefficient per group are summarized. Smoking based on cotinine measurement was 25.6%, 18.4%, and 15.5% in the screening, surgery, and follow-up group, respectively. A history of smoking was reported by 41.2%, 49.4%, and 39.0% of the patients, in the screening, surgery, and follow-up group, respectively. The sensitivity of self-reported smoking was 72.5%, 31.0%, and 93.5% in the screening, surgery, and follow-up group, respectively (p < 0.001). The specificity of self-report was 99.6%, 99.3%, and 96.4% in the screening, surgery, and follow-up group, respectively (p < 0.02). The kappa between self-report and cotinine was 0.784 for the screening group, 0.414 for the surgery group, and 0.855 for the follow-up group.
Fifty-three of 199 patients in the screening group were not operated for several reasons. In 22 (41.5%) of them, cotinine was detected, and 16 (30.2%) reported smoking. Once, an unsuccessful cessation of smoking was mentioned as reason for postponement of the operation.
Accuracy of Self-Report and Exposure to Other Types of Nicotine
We found no clinically relevant differences in baseline characteristics between patients who reported smoking accurately, patients who concealed smoking, patients who reported correctly to be non- smoking, or those who inaccurately reported to be smoking (data not shown).
In Table 3, cotinine values and characteristics of secondhand smoking exposure are shown, in all patients and grouped on accuracy of self-report. Overall, seven patients (< 1%) had used e-cigarettes, and no other type of nicotine replacement product was reported. Two of the seven patients reported also to be a current smoker (one in screening and one in follow-up group). Five patients (all in the surgery group) reported to have already stopped with cigarette smoking; the shortest cessation period was 2.3 months, the longest 4 years. All cotinine levels were above 180 ng/ml (mean 284.8 ng/ml (SD 67.4)).
30-Day Complications
For the relationship between self-reported smoking, cotinine, and complications within 30 days after surgery, we analyzed the screening group and the surgery group (Total n = 461). Overall, 73 (15.8%) of these patients had a surgical complication (bleedings (n = 22), nausea or dysphagia (n = 11), abdominal pain (n = 7), infection (n = 7), leakage of anastomosis (n = 6), stenosis (n = 5), allergic reaction (n = 3), other complications (n = 11), and one patient died. Forty-seven complications (10.2%) were classified as Clavien Dindo I, 15 (3.3%) as Clavien Dindo II; 10 complications (2.2%) were categorized as Clavien Dindo III, and one complication (0.2%) as Clavien Dindo V.
In the screening group, cotinine was detected in eight (33%) of the patients with a complication and in 21 (17%) without complication. Smoking was reported by seven patients (29%) with a complication and by 14 (12%) without a complication. The adjusted odds ratios for having a postoperative complication were 3.8 (1.3–11.3) for positive cotinine and 5.1 (1.6–16.4) for self-reported smoking. We adjusted for presence of type 2 diabetes, preoperative BMI, time before surgery, and primary bariatric surgery (Table 4).
In the surgery group, cotinine was detected in eight patients (15%) with a complication and in 49 (19%) without a complication. Smoking was reported by three patients (6%) with a complication and by 16 (6%) without a complication. In this group, the adjusted odds ratios for having a postoperative complication were 0.9 (0.4–2.2) for positive cotinine and 1.1 (0.3–3.9) for self-reported smoking. We adjusted for gender, preoperative BMI, age, and presence of hypertension (Table 5).
Discussion
This is the first study in bariatric surgery examining the accuracy of self-reported smoking status. When smoking was based on cotinine concentration, 15.5–25.6% of all patients was currently smoking on the different time points before and after surgery. As hypothesized, underreporting of smoking is present during the screening period before surgery (sensitivity 72.5%) and especially on the day of surgery (sensitivity 31.0%). This indicates that preoperative self-reported smoking is a poor indicator of actual smoking status compared to cotinine values. The self-reported smoking status is most reliable when patients are already operated (sensitivity 93.5%).
In most bariatric surgery studies, smoking is based on self-report and medical chart review [3, 11,12,13,14,15,16,17, 33,34,35,36,37,38,39,40]. Our study shows that it really matters at which moment smoking status is reported and that is likely that underreporting may influence results and conclusions of studies. We evaluated how and at which moment smoking status was evaluated in all studies since 2010 in which smoking status was an outcome or was associated with bariatric surgery outcome (Table 6) [3, 11,12,13,14,15,16,17, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. This evaluation showed that all studies were based on self-report or medical chart, and in only a few studies, a specific questionnaire was used. It also indicated that in many studies, the definitions of smoking or former smoking were not well described, and the percentages of lost to follow-up were high. This underlines that results of these studies are based on an imprecise method to evaluate smoking status and patient groups with many missing data which will definitely influence results.
Possible explanations for inaccurate self-report are high quitting expectations from the health care team, embarrassment for failing to quit, fear for gaining weight as a result of smoking cessation (which interferes with the preoperative weight goal), the stigma associated with smoking, and fear for rejection [18,19,20, 60]. However, fear for rejection could have been an extra motivation to stop (at least temporarily) and accept the offered support, which would abate the necessity of concealing. And, misclassification is a common problem in settings where there is no surgery involved [18,19,20, 61,62,63,64]. Our patients were informed that the self-report would be solely related to cotinine and would never be visible for their attending doctor. Hence, the problem of misclassification could be larger in normal practice, when patients report smoking to their attending doctor, without verification. Consequently, patients who disclose their smoking are not encouraged to attempt cessation, are poorly informed about possible positive effects of quitting, and receive no individual support.
Smoking is known to contribute to short-term and long-term postoperative complications [3,4,5, 12, 13, 15, 16, 34, 36, 46, 65]. In our study, current smoking based on cotinine and self-report at the phase of screening was associated with complications after surgery, but smoking at the day of surgery not. Studies on the timing of preoperative smoking cessation to effect short-term postoperative complications in the field of bariatric surgery are scarce. Mean time until surgery was approximately 5 months. Exact timing of the smoking cessation and the success rate in the screening group is unclear but was ineffective to improve complication rates. We suggest further research on this topic should use cotinine to assess preoperative smoking.
Cotinine detected at the day of surgery was not a predictor for complications, possibly due to occasional smoking out of fear for the operation and due to a short period of smoking cessation on the other hand. Clearly, the level of cotinine on the day of surgery does not represent the impairment of organs by rarely occasional smoking or the improvement after short-term smoking cessation. The exact duration of cessation is unknown, because cotinine is generally only detectable during the first 48–96 h after inhalation of a cigarette [19, 22,23,24,25, 66, 67].
Noteworthy is the preoperative group that is not (yet) operated; 41.5% had positive cotinine test at screening. Reasons for forgoing, postponement, or rejections are diverse; only once an unsuccessful cessation of smoking was mentioned. Other studies have shown that a history of smoking is associated with longer wait times [68,69,70].
In spite of the preoperative urgent advice to quit smoking for a lifetime, 15% of all the patients after surgery appeared to be a current smoker. This emphasizes the ongoing need for routinely monitoring the smoking status, better counseling, and the necessity for more effective long-term smoking cessation strategies, also after surgery.
We used solid-phase extraction in combination with high-performance liquid chromatography (HPLC) to measure cotinine levels [19, 26,27,28,29,30,31]. The intra- and inter-assay variabilities indicate safe and valid use of HPLC in this study. To rule out possible interference in the determination of cotinine, we checked for peak purity for each positive cotinine test. We did not focus on the correlation between cotinine concentration and reported number of cigarettes, which may be relevant when investigating a dose response reaction.
It still may be difficult to correctly identify a smoker using cotinine taking into account the short half-life, the time between smoking and sample collection, variation in metabolism of nicotine (race, ethnicity, gender, medications, diet, age, genetic variation in CYP2A6 enzyme, pregnancy, liver or kidney disease), intermittent smokers, patients heavily exposed to secondhand smoking (SHS), and interference by species of the nightshades family. [19, 22, 25, 67, 71,72,73,74,75,76,77,78,79,80]
Nevertheless, our cut-off value was relatively high; patients (heavily) exposed to secondhand smoking often do not reach serum levels above 3 ng/ml, and in non-smoking subjects, cotinine concentrations are below 1 ng/ml [22, 67, 78, 81,82,83,84]. In active smokers, much higher concentrations have been found (often above 100 ng/ml) [73, 81, 83, 85]. In agreement with this, no positive cotinines were detected in the “correctly non-smoking and incorrectly smoking” group. Thus, the high levels of cotinine (in total and SHS subgroup) in the patients that concealed smoking and the fact that the SHS part of this group had not lower but higher values supports active smoking as explanation of increased cotinine instead of very heavy secondhand smoking. Due to variation in metabolism of cotinine and divergent steady-state levels before cessation, we cannot exclude that patients truly had stopped more than 48 h before, although this is unlikely the case in all patients [19, 22, 25, 67, 71,72,73,74,75,76,77,78,79,80].
Only five (< 1%) patients reported to have solely used electronic cigarettes during the last 48 h. We collected no further information about brand, generation, composition of vapor, level of nicotine, or experience of vaping. All these factors can influence actual nicotine delivery. Although, by vaporizing, patients often do not reach the blood levels that can be achieved by cigarette smoking [86,87,88]. Therefore, it is unlikely that cotinine levels of above 180 ng/ml can be explained by the use of e-cigarettes. No use of other types of nicotine replacement products was reported.
The effect of selection bias seems limited. In this large sample, we included all patients consecutively and only 27 (3.6%) patients were excluded. This high inclusion rate was established by the inclusion setting at the laboratory where the patients had to draw blood anyway. Potentially, all 27 exclusions could have been smoking; nonetheless, the percentage is low (3.6%) and suggests that reliable conclusions can be made.
In conclusion, smoking is underreported especially in patients at the day of bariatric surgery, but also in the trajectory months before surgery. Self-reported smoking is most reliable when patients are already operated. Cotinine-based and self-reported smoking was associated with the occurrence of postoperative complications at the phase of screening, but smoking at the day of screening was not. In most previous studies on smoking and bariatric surgery, outcome smoking was assessed by different types of self-report and often without precise definition and timing of smoking status. Future studies on risks of smoking should include cotinine measurement or other methods to address the issue of underreporting. In addition, reporting and evaluation of current policies on smoking cessation and intervention studies on the effects of smoking cessation before and after bariatric surgery are warranted.
References
Arterburn DE, Courcoulas AP. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014;349(aug 27):g349–g3961.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–73.
Haskins IN, Amdur R, Vaziri K. The effect of smoking on bariatric surgical outcomes. Surg Endosc. 2014;28(11):3074–80.
Livingston EH, Arterburn D, Schifftner TL, et al. National surgical quality improvement program analysis of bariatric operations: modifiable risk factors contribute to bariatric surgical adverse outcomes. J Am Coll Surg. 2006;203(5):625–33.
Theadom A, Cropley M. Effects of preoperative smoking cessation on the incidence and risk of intraoperative and postoperative complications in adult smokers: a systematic review. Tob Control. 2006;15(5):352–8.
Tønnesen H, Nielsen PR, Lauritzen JB, et al. Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth. 2009;102(3):297–306.
Akrawi WBJL. A pathophysiological basis for informed preoperative smoking cessation counseling. J Cardiothorac Vasc Anesth. 1997;11(5):629–40.
Mills E, Eyawo O, Lockhart I, et al. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med. 2011;124(2):144–54.
Moller A, Villebro N, Pedersen T. Interventions for preoperative smoking cessation (review). Cochrane Database Syst Rev. 2014 Mar 27;(3):CD002294. https://doi.org/10.1002/14651858.CD002294.pub4
Gourgiotis S, Aloizos S, Aravosita P, et al. The effects of tobacco smoking on the incidence and risk of intraoperative and postoperative complications in adults. Surgeon. 2011;9(4):225–32.
Conason A, Teixeira J, Hsu CH, et al. Substance use following bariatric weight loss surgery. JAMA Surg. 2013;148(2):145–50.
Haskins IN, Nowacki AS, Khorgami Z, et al. Should recent smoking be a contraindication for sleeve gastrectomy? Surg Obes Relat Dis. 2017;13(7):1130–5.
Inadomi M, Iyengar R, Fischer I, et al. Effect of patient-reported smoking status on short-term bariatric surgery outcomes. Surg Endosc. 2018;32(2):720–6.
Kowalewski PK, Olszewski R, Waledziak MS, et al. Cigarette smoking and its impact on weight loss after bariatric surgery: a single center, retrospective study. Surg Obes Relat Dis. 2018;14(8):1163–6.
Lent MR, Hu Y, Benotti PN, et al. Demographic, clinical, and behavioral determinants of 7-year weight change trajectories in roux-en-Y gastric bypass patients. Surg Obes Relat Dis. 2018;14(11):1680–5.
Mitchell JE, Christian NJ, Flum DR, et al. Postoperative behavioral variables and weight change 3 years after bariatric surgery. JAMA Surg. 2016;151(8):752–7.
Moser F, Signorini FJ, Maldonado PS, et al. Relationship between tobacco use and weight loss after bariatric surgery. Obes Surg. 2016;26(8):1777–81.
Gorber SC, Schofield-Hurwitz S, Hardt J, et al. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res. 2009;11(1):12–24.
Florescu A. Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: focus on developmental toxicology. Drug Monitor. 2009;31(1):14–30.
Patrick DL, Cheadle A, Thompson DC, et al. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086–93.
Ambwani S, Boeka AG, Brown JD, et al. Socially desirable responding by bariatric surgery candidates during psychological assessment. Surg Obes Relat Dis. 2013;9(2):300–5.
Benowitz NL. Cotinine as a biomarker of environmental tobacco smoke exposure. Epidemiol Rev. 1996;18(2):188–204.
Haley NJ, Sepkovic DW, Hoffmann D. Elimination of cotinine from body fluids: disposition in smokers and nonsmokers. Am J Public Health. 1989;79(8):1046–8.
Zevin S, Jacob 3rd P, Benowitz N. Cotinine effects on nicotine metabolism. Clin Pharmacol Ther. 1997;61(6):649–54.
Verification SfRoNaTSoB. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4(2):149–59.
Zuccaro P, Altieri I, Rosa M, et al. Determination of nicotine and 4 metabolites in the serum of smokers by high-performance liquid-chromatography with ultraviolet detection. J Chromatogr-Biomed. 1993;621(2):257–61.
Pacifici R, Pichini S, Altieri I, et al. Determination of nicotine and 2 major metabolites in serum by solid-phase extraction and high-performance liquid-chromatography, and high-performance liquid-chromatography particle beam mass-spectrometry. J Chromatogr-Biomed. 1993;612(2):209–13.
Zuccaro P, Altieri I, Rosa M, et al. Solid-phase extraction of nicotine and its metabolites for high-performance liquid-chromatographic determination in urine. J Chromatogr B. 1995;668(1):187–8.
Teeuwen HWA, Aalders RJW, Vanrossum JM. Simultaneous estimation of nicotine and cotinine levels in biological-fluids using high-resolution capillary-column gas-chromatography combined with solid-phase extraction work-up. Mol Biol Rep. 1989;13(3):165–75.
Pichini S, Altieri I, Pacifici R, et al. Simultaneous determination of cotinine and trans-3'-hydroxycotinine in human serum by high-performance liquid-chromatography. J Chromatogr-Biomed. 1992;577(2):358–61.
Pichini S, Altieri I, Passa AR, et al. Cotinine content in control sera. J Anal Toxicol. 1995;19(4):267–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Coblijn UK, Karres J, de Raaff CAL, et al. Predicting postoperative complications after bariatric surgery: the bariatric surgery index for complications. BASIC Surg Endosc. 2017;31(11):4438–45.
Coblijn UK, Lagarde SM, de Castro SM, et al. Symptomatic marginal ulcer disease after roux-en-Y gastric bypass: incidence, risk factors and management. Obes Surg. 2015;25(5):805–11.
Pierik AS, Coblijn UK, de Raaff CAL, et al. Unexplained abdominal pain in morbidly obese patients after bariatric surgery. Surg Obes Relat Dis. 2017;13(10):1743–51.
Adams CE, Gabriele JM, Baillie LE, et al. Tobacco use and substance use disorders as predictors of postoperative weight loss 2 years after bariatric surgery. J Behav Health Serv Res. 2012;39(4):462–71.
Wood GC, Benotti PN, Lee CJ, et al. Evaluation of the association between preoperative clinical factors and long-term weight loss after roux-en-Y gastric bypass. JAMA Surg. 2016;151(11):1056–62.
Wood GC, Chu X, Manney C, et al. An electronic health record-enabled obesity database. BMC Med Inform Decis Mak. 2012;28:12.
Cayci HM, Oner S, Erdogdu UE, et al. The factors affecting lower urinary tract functions in patients undergoing laparoscopic sleeve gastrectomy. Obes Surg. 2018;28(4):1025–30.
Lent MR, Hayes SM, Wood GC, et al. Smoking and alcohol use in gastric bypass patients. Eat Behav. 2013;14(4):460–3.
Still CD, Wood GC, Chu X, et al. Clinical factors associated with weight loss outcomes after Roux-en-Y gastric bypass surgery. Obesity (Silver Spring, Md). 2014;22(3):888–94.
Maniscalco M, Carratu P, Faraone S, et al. Smoking habit in severe obese after bariatric procedures. Tob Induc Dis. 2015;13(1):20.
Finks JF, Kole KL, Yenumula PR, et al. Predicting risk for serious complications with bariatric surgery: results from the Michigan bariatric surgery collaborative. Ann Surg. 2011;254(4):633–40.
Turner PL, Saager L, Dalton J, et al. A nomogram for predicting surgical complications in bariatric surgery patients. Obes Surg. 2011;21(5):655–62.
Gupta PK, Franck C, Miller WJ, et al. Development and validation of a bariatric surgery morbidity risk calculator using the prospective, multicenter NSQIP dataset. J Am Coll Surg. 2011;212(3):301–9.
King WC, Chen JY, Mitchell JE, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307(23):2516–25.
Belle SH, Berk PD, Chapman WH, et al. Baseline characteristics of participants in the longitudinal assessment of bariatric surgery-2 (LABS-2) study. Surg Obes Relat Dis. 2013;9(6):926–35.
Gordon PC, Sallet JA, Sallet PC. The impact of temperament and character inventory personality traits on long-term outcome of roux-en-Y gastric bypass. Obes Surg. 2014;24(10):1647–55.
Ramanan B, Gupta PK, Gupta H, et al. Development and validation of a bariatric surgery mortality risk calculator. J Am Coll Surg. 2012;214(6):892–900.
Arterburn D, Livingston EH, Olsen MK, et al. Predictors of initial weight loss after gastric bypass surgery in twelve veterans affairs medical centers. Obes Res Clin Pract. 2013;7(5):e367–76.
Benotti P, Wood GC, Winegar DA, et al. Risk factors associated with mortality after roux-en-Y gastric bypass surgery. Ann Surg. 2014;259(1):123–30.
Spaniolas K, Yang J, Crowley S, et al. Association of long-term anastomotic ulceration after roux-en-Y gastric bypass with tobacco smoking. JAMA Surg. 2018;153(9):862–4.
Signorini FJ, Polero V, Viscido G, et al. Long-term relationship between tobacco use and weight loss after sleeve gastrectomy. Obes Surg. 2018;28(9):2644–9.
Birkmeyer NJ, Dimick JB, Share D, et al. Hospital complication rates with bariatric surgery in Michigan. JAMA. 2010;304(4):435–42.
Odom J, Zalesin KC, Washington TL, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg. 2010;20(3):349–56.
Mitchell JE, Steffen K, Engel S, et al. Addictive disorders after roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015 Jul-Aug;11(4):897–905. https://doi.org/10.1016/j.soard.2014.10.026. Epub 2014 Nov 13.
King WC, Chen J-Y, Belle SH, et al. Surgery for use of prescribed opioids before and after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis. 2017;13:1337–46.
Altieri MS, Aurora Pryor B, Jie Yang B, et al. The natural history of perforated marginal ulcers after gastric bypass surgery. Surg Endosc. 2018;32(3):1215-1222. https://doi.org/10.1007/s00464-017-5794-4. Epub 2017 Aug 25.
Kedrin D, Gandhi SC, Wolf M, et al. Bariatric surgery prior to index screening colonoscopy is associated with a decreased rate of colorectal adenomas in obese individuals. Clin Transl Gastroenterol. 2017;8(2):e73.
Aubin HJ, Farley A, Lycett D, et al. Weight gain in smokers after quitting cigarettes: meta-analysis. BMJ (Online). 2012;345(7868):1–21.
Boyd NR, Windsor RA, Perkins LL, et al. Quality of measurement of smoking status by self-report and saliva cotinine among pregnant women. Matern Child Health J. 1998;2(2):77–83.
Coultas DB, Howard CA, Peake GT, et al. Discrepancies between self-reported and validated cigarette smoking in a community survey of New Mexico Hispanics. Am Rev Respir Dis. 1988;137(4):810–4.
Hald J, Overgaard J, Grau C. Evaluation of objective measures of smoking status--a prospective clinical study in a group of head and neck cancer patients treated with radiotherapy. Acta Oncol. 2003;42(2):154–9.
Lewis SJ, Cherry NM, Mc LNR, et al. Cotinine levels and self-reported smoking status in patients attending a bronchoscopy clinic. Biomarkers. 2003;8(3–4):218–28.
Wilson JA, Romagnuolo J, Karl Byrne T, et al. Predictors of endoscopic findings after roux-en-Y gastric bypass. Am J Gastroenterol. 2006;101(10):2194–9.
Benowitz NL, Jacob 3rd. P. Daily intake of nicotine during cigarette smoking. Clin Pharmacol Ther. 1984;35(4):499–504.
Benowitz NL, Dains KM, Dempsey D, et al. Urine nicotine metabolite concentrations in relation to plasma cotinine during low-level nicotine exposure. Nicotine Tob Res. 2009;11(8):954–60.
Alvarez R, Bonham AJ, Buda CM, Carlin AM, Ghaferi AA, Varban OA. Factors associated with long wait times for bariatric surgery. Ann Surg. 2018.https://doi.org/10.1097/SLA.0000000000002826. [Epub ahead of print].
Heinberg LJ, Ashton K, Windover A. Moving beyond dichotomous psychological evaluation: the Cleveland clinic behavioral rating system for weight loss surgery. Surg Obes Relat Dis. 2010;6(2):185–90.
Heinberg L, Marek R, Haskins IN, et al. 30-day readmission following weight loss surgery: can psychological factors predict nonspecific indications for readmission? Surg Obes Relat Dis. 2017;13(8):1376–81.
Benowitz NL, Jacob 3rd. P. Nicotine and cotinine elimination pharmacokinetics in smokers and nonsmokers. Clin Pharmacol Ther. 1993;53(3):316–23.
Benowitz NL, Pomerleau OF, Pomerleau CS, et al. Nicotine metabolite ratio as a predictor of cigarette consumption. Nicotine Tob Res. 2003;5(5):621–4.
Benowitz NL, Bernert JT, Caraballo RS, et al. Optimal serum cotinine levels for distinguishing cigarette smokers and nonsmokers within different racial/ethnic groups in the United States between 1999 and 2004. Am J Epidemiol. 2009;169(2):236–48.
Benowitz NL, Schultz KE, Haller CA, et al. Prevalence of smoking assessed biochemically in an urban public hospital: a rationale for routine cotinine screening. Am J Epidemiol. 2009;170(7):885–91.
Benowitz NL, Hukkanen J, Jacob 3rd. P. Nicotine chemistry, metabolism, kinetics and biomarkers. Handb Exp Pharmacol. 2009;192:29–60.
Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362(24):2295–303.
Bernert JT, Jacob 3rd P, Holiday DB, et al. Interlaboratory comparability of serum cotinine measurements at smoker and nonsmoker concentration levels: a round-robin study. Nicotine Tob Res. 2009;11(12):1458–66.
Kim S. Overview of cotinine cutoff values for smoking status classification. Int J Environ Res Public Health. 2016;13(12)
Kyerematen GA, Damiano MD, Dvorchik BH, et al. Smoking-induced changes in nicotine disposition: application of a new HPLC assay for nicotine and its metabolites. Clin Pharmacol Ther. 1982;32(6):769–80.
Siegmund B, Leyden DE, Zikulnig E, et al. The contribution of dietary nicotine and dietary cotinine to salivary cotinine levels as a nicotine biomarker. Food Chem. 2001;74(3):259–65.
Jarvis M, Tunstall-Pedoe H, Feyerabend C, et al. Biochemical markers of smoke absorption and self reported exposure to passive smoking. J Epidemiol Community Health. 1984;38(4):335–9.
Ballbe M, Martinez-Sanchez JM, Sureda X, et al. Cigarettes vs. e-cigarettes: passive exposure at home measured by means of airborne marker and biomarkers. Environ Res. 2014;135:76–80.
Flouris AD, Chorti MS, Poulianiti KP, et al. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhal Toxicol. 2013;25(2):91–101.
Metsios GS, Flouris AD, Jamurtas AZ, et al. A brief exposure to moderate passive smoke increases metabolism and thyroid hormone secretion. J Clin Endocrinol Metab. 2007;92(1):208–11.
Schnoll RA, Patterson F, Wileyto EP, et al. Nicotine metabolic rate predicts successful smoking cessation with transdermal nicotine: a validation study. Pharmacol Biochem Behav. 2009;92(1):6–11.
Hartmann-Boyce J, McRobbie H, Bullen C, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:CD010216.
Vansickel AR, Cobb CO, Weaver MF, et al. A clinical laboratory model for evaluating the acute effects of electronic “cigarettes”: nicotine delivery profile and cardiovascular and subjective effects. Cancer Epidemiol Biomark Prev. 2010;19(8):1945–53.
Eissenberg T. Electronic nicotine delivery devices: ineffective nicotine delivery and craving suppression after acute administration. Tob Control. 2010;19(1):87–8.
Acknowledgments
We thank all colleagues of the former MC Slotervaart who have contributed to the care for the patients in this study, especially the colleagues at the laboratory and the medium care department. We thank Fidessa Straat for helping with the recruitment of patients. The bariatric surgery team of the MC Slotervaart will continue at the Spaarne Gasthuis after the bankruptcy of the hospital in 2018.
Funding
This study was funded by the SKWOSZ (Foundation for Clinical Scientific Research at Medical Center Slotervaart).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. This study was approved by the Institutional review board.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wolvers, P.J.D., Bruin, S.C., Mairuhu, W.M. et al. Self-Reported Smoking Compared to Serum Cotinine in Bariatric Surgery Patients: Smoking Is Underreported Before the Operation. OBES SURG 30, 23–37 (2020). https://doi.org/10.1007/s11695-019-04128-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04128-4