Abstract
Background
Bariatric surgery candidates exhibit cognitive impairment on neuropsychological testing and these deficits are associated with reduced post-operative weight loss. However, less is known about the prevalence of cognitive function in older adults that pursue surgery, despite being at higher risk for cognitive dysfunction.
Objective
To examine the prevalence and profile of cognitive impairment using the Montreal Cognitive Assessment (MoCA) in elderly bariatric patients. We hypothesized that increased body mass index (BMI) and higher number of medications would be linked to lower MoCA score, and that men would evidence poorer MoCA scores than women given past work showing that men presenting for bariatric surgery have more medical comorbidities.
Methods
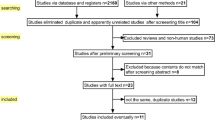
Data was retrospectively extracted from electronic medical records. Patients 65 and older who completed pre-surgical MoCA assessment and bariatric surgery were included in the study (n = 55).
Results
Twenty-two percent of patients scored below cutoff for impairment on the MoCA. MoCA total score was negatively correlated with BMI and number of medications pre-surgery. There was a significant effect for gender, with men outperforming women.
Conclusions
The current findings suggest that cognitive impairment is common in older adults presenting for bariatric surgery. Future studies are needed to determine the most appropriate methods for detecting cognitive dysfunction in this high-risk population.
Similar content being viewed by others
References
Rochette AD, Spitznagel MB, Strain G, et al. Mild cognitive impairment is prevalent in persons with severe obesity. Obesity (Silver Spring). 2016;24:1427–9.
Spitznagel MB, Galioto R, Limbach K, et al. Cognitive function is linked to adherence to bariatric postoperative guidelines. Surg Obes Relat Disord. 2013c;9:580–5.
Spitznagel MB, Garcia S, Miller LA, et al. Cognitive function predicts weight loss after bariatric surgery. Surg Obes Relat Disord. 2013a;9:453–9.
Spitznagel MB, Alosco M, Strain G, et al. Cognitive function predicts 24-month weight loss success following bariatric surgery. Surg Obes Relat Disord. 2013b;9:765–70.
Spitznagel MB, Alosco M, Galioto R, et al. The role of cognitive function in postoperative weight loss outcomes: 36 moth follow-up. Obes Surg. 24:1078–84.
Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. J Am Med Assoc. 2012;307(5):491–7.
Alosco ML, Spitznagel MB, Gunstad J. Obesity as a risk factor for poor neurocognitive outcomes in older adults with heart failure. Heart Fail Rev. 2014;19:403–11.
Alosco ML, Cohen R, Spitznagel MB, et al. Older age does not limit post-bariatric surgery cognitive benefits: a preliminary investigation. Surg Obes Relat Dis. 2014;10(6):1196–201.
Stanek KM, Strain G, Devlin M, et al. Body mass index and neurocognitive functioning across the adult lifespan. Neuropsychology. 2013;27:141–51.
Chodosh, J., Petitti, D. B., Elliot, M., Hays, R. D., Crooks, V. C., Reuben, D. B.,. .. Wenger, N. (2004). Physician recognition of cognitive impairment: evaluating the need for improvement. J Am Geriatr Soc, 52, 1051–1059.
Valcour VG, Masaki KH, Curb JD, et al. The detection of dementia in the primary care setting. Arch Intern Med. 2000;160:2964–8.
Petersen RC, Morris JC. Mild cognitive impairment as a clinical entity and treatment target. Arch Neurol. 2005;62:1160–3.
Galioto R, Garcia S, Sptiznagel MB, et al. The Mini-Mental State Exam (MMSE) is not sensitive to cognitive impairment in bariatric surgery candidates. Surg Obes Relat Dis. 2014;10:553–9.
Spitznagel MB, Hawkins M, Alosco M, et al. Neurocognitive effects of obesity and bariatric surgery. Gunstad, J., Eur Eat Disord Rev. 23:488–95.
Julayanont, P., & Nasreddine, Z. (2017). Montreal Cognitive Assessment (MoCA): concept and clinical review in A. J. Larner (Ed), Cognitive Screening Instruments. Cham, Switzerland: Springer International Publishing.
Luis CA, Keegan AP, Mullan M. Cross validation of the Montreal Cognitive Assessment in community dwelling older adults residing in the Southeastern US. Int J Geriatr Psychiatry. 2009;24:197–201.
Agmon M, Armon G. A cross-sectional study of the association between mobility test performance and personality among older adults. BioMed Central Geriatr. 2016;16:105.
Farinholt GN, Carr AD, Chang EJ, et al. A call to arms: obese men with more severe comorbid disease and underutilization of bariatric operations. Surg Endosc. 2013;27(12):4556–63.
Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9.
Manderino L, Spitznagel MB, Strain G, et al. Cognitive dysfunction predicts poorer emotion recognition in bariatric surgery candidates. Obes Sci Pract. 2015;1:97–103.
Gunstad J, Strain G, Devlin MJ, et al. Improved memory function 12 weeks after bariatric surgery. Surg Obes Relat Dis. 2011;7:465–72.
Libeton M, Dixon JB, Laurie C, et al. Patient motivation for bariatric surgery: characteristics and impact on outcomes. Obes Surg. 2004;14:392–8.
Mahony D. Psychological gender differences in bariatric surgery candidates. Obesity Surgery. 2007;18(5):607–10.
Cheke LG, Simons JS, Clayton NS. Higher BMI is associated with episodic memory deficits in young adults. Q J Exp Psychol. 2015;
Kivipelto M, Ngandu T, Fratiglioni L, et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol. 2005;62:1556–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
The Institutional Review Board approved the preceding as an exempt study as it involved retrospective chart review.
Rights and permissions
About this article
Cite this article
Mohun, S.H., Spitznagel, M.B., Gunstad, J. et al. Performance on the Montreal Cognitive Assessment (MoCA) in Older Adults Presenting for Bariatric Surgery. OBES SURG 28, 2700–2704 (2018). https://doi.org/10.1007/s11695-018-3206-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3206-z