Abstract
Background
Utilization of the robotic platform has become more common in bariatric applications. We aim to show that robotic revisional bariatric surgery (RRBS) can be safely performed in a complex patient population with perioperative outcomes equivalent to laparoscopic revisional bariatric surgery (LRBS).
Methods
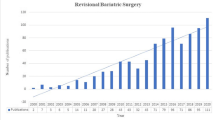
Retrospective review was conducted of adult patients undergoing laparoscopic revisional bariatric surgery (LRBS) or robotic revisional bariatric surgery (RRBS) at our institution from September 2007 to December 2016. Patients undergoing planned two-stage bariatric procedures were excluded.
Results
A total of 84 patients who underwent LRBS (n = 66) or RRBS (n = 18) were included. The index operation was adjustable gastric banding (AGB) in 39/84 (46%), sleeve gastrectomy (VSG) in 23/84 (27%), Roux-en-Y gastric bypass (RYGB) in 13/84 (16%), and vertical banded gastroplasty (VBG) in 9/84 (11%). For patients undergoing conversion from AGB (n = 39), there was no difference in operative time, length of stay, or complications by surgical approach. For patients undergoing conversion from a stapled procedure (n = 45), the robotic approach was associated with a shorter length of stay (5.8 ± 3.3 vs 3.7 ± 1.7 days, p = 0.04) with equivalent operative time and post-operative complications. There were three leaks in the LRBS group and none in the RRBS group (p = 0.36). Major complications occurred in 3/39 (8%) of patients undergoing conversion from AGB and 2/45 (4%) of patients undergoing conversion from a stapled procedure (p = 0.53) with no difference by surgical approach.
Conclusions
RRBS is associated with a shorter length of stay than LRBS in complex procedures and has at least an equivalent safety profile. Long-term follow-up data is needed.


Similar content being viewed by others
References
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52. https://doi.org/10.1056/NEJMoa066254.
Brethauer SA, Kothari S, Sudan R, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10(5):952–72. https://doi.org/10.1016/j.soard.2014.02.014.
Arapis K, Tammaro P, Parenti LR, et al. Long-term results after laparoscopic adjustable gastric banding for morbid obesity: 18-year follow-up in a single university unit. Obes Surg. 2016.
Carandina S, Tabbara M, Galiay L, et al. Long-term outcomes of the laparoscopic adjustable gastric banding: weight loss and removal rate. A single center experience on 301 patients with a minimum follow-up of 10 years. Obes Surg. 2016.
Abraham A, Ikramuddin S, Jahansouz C, et al. Trends in bariatric surgery: procedure selection, revisional surgeries, and readmissions. Obes Surg. 2016;26(7):1371–7. https://doi.org/10.1007/s11695-015-1974-2.
Inabnet WB, Belle SH, Bessler M, et al. Comparison of 30-day outcomes after non-LapBand primary and revisional bariatric surgical procedures from the longitudinal assessment of bariatric surgery study. Surg Obes Relat Dis. 2010;6(1):22–30. https://doi.org/10.1016/j.soard.2009.10.007.
Ponce J, DeMaria EJ, Nguyen NT, et al. American Society for Metabolic and Bariatric Surgery estimation of bariatric surgery procedures in 2015 and surgeon workforce in the United States. Surg Obes Relat Dis. 2016;12(9):1637–9. https://doi.org/10.1016/j.soard.2016.08.488.
Casillas RA, Um SS, Zelada Getty JL, et al. Revision of primary sleeve gastrectomy to roux-en-Y gastric bypass: indications and outcomes from a high-volume center. Surg Obes Relat Dis. 2016;12(10):1817–25. https://doi.org/10.1016/j.soard.2016.09.038.
Stefanidis D, Malireddy K, Kuwada T, et al. Revisional bariatric surgery: perioperative morbidity is determined by type of procedure. Surg Endosc. 2013;27(12):4504–10. https://doi.org/10.1007/s00464-013-3097-y.
Toro JP, Lin E, Patel AD. Review of robotics in foregut and bariatric surgery. Surg Endosc. 2015;29:1–8.
Prete FP, Pezzolla A, Prete F, et al. Robotic versus laparoscopic minimally invasive surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2017;1. https://doi.org/10.1097/SLA.0000000000002523.
Wilson EB, Sudan R. The evolution of robotic bariatric surgery. World J Surg. 2013;37(12):2756–60. https://doi.org/10.1007/s00268-013-2125-3.
Ayloo SM, Choudhury N. Robotic revisional bariatric surgery: single-surgeon case series. Int J Med Robot. 2014.
Buchs NC, Pugin F, Azagury DE, et al. Robotic revisional bariatric surgery: a comparative study with laparoscopic and open surgery. Int J Med Robot. 2014;10(2):213–7. https://doi.org/10.1002/rcs.1549.
Maeso S, Reza M, Mayol JA, et al. Efficacy of the Da Vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis. Ann Surg. 2010;252(2):254–62. https://doi.org/10.1097/SLA.0b013e3181e6239e.
Economopoulos KP, Theocharidis V, McKenzie TJ, et al. Robotic vs. laparoscopic roux-en-Y gastric bypass: a systematic review and meta-analysis. Obes Surg. 2015;25(11):2180–9. https://doi.org/10.1007/s11695-015-1870-9.
Magouliotis DE, Tasiopoulou VS, Sioka E, et al. Robotic versus laparoscopic sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis. Obes Surg. 2017;27(1):245–53. https://doi.org/10.1007/s11695-016-2444-1.
Antanavicius G, Sucandy I. Robotically-assisted laparoscopic biliopancreatic diversion with duodenal switch: the utility of the robotic system in bariatric surgery. J Robot Surg. 2013;7(3):261–6. https://doi.org/10.1007/s11701-012-0372-1.
Edelson PK, Dumon KR, Sonnad SS, et al. Robotic vs. conventional laparoscopic gastric banding: a comparison of 407 cases. Surg Endosc. 2011;25(5):1402–8. https://doi.org/10.1007/s00464-010-1403-5.
Luciani LG, Chiodini S, Mattevi D, et al. Robotic-assisted partial nephrectomy provides better operative outcomes as compared to the laparoscopic and open approaches: results from a prospective cohort study. J Robot Surg. 2017;11(3):333–9. https://doi.org/10.1007/s11701-016-0660-2.
Thomas MN, Kufeldt J, Kisser U, et al. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition. 2016;32(2):249–54. https://doi.org/10.1016/j.nut.2015.08.021.
Abdelgawad M, De Angelis F, Iossa A, et al. Management of complications and outcomes after revisional bariatric surgery: 3-year experience at a Bariatric Center of Excellence. Obes Surg. 2016;26(9):2144–9. https://doi.org/10.1007/s11695-016-2071-x.
Miller K, Pump A, Hell E. Vertical banded gastroplasty versus adjustable gastric banding: prospective long-term follow-up study. Surg Obes Relat Dis. 2007;3(1):84–90. https://doi.org/10.1016/j.soard.2006.08.013.
Nocca D, Loureiro M, Skalli EM, et al. Five-year results of laparoscopic sleeve gastrectomy for the treatment of severe obesity. Surg Endosc. 2016.
Arman GA, Himpens J, Dhaenens J, et al. Long-term (11+years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(10):1778–86. https://doi.org/10.1016/j.soard.2016.01.013.
Obeid NR, Malick W, Concors SJ, et al. Long-term outcomes after Roux-en-Y gastric bypass: 10- to 13-year data. Surg Obes Relat Dis. 2016;12(1):11–20. https://doi.org/10.1016/j.soard.2015.04.011.
Funding
This study was internally funded.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Dr. Afaneh reports honoraria from Intuitive Surgical, outside the submitted work. Dr. Pomp reports personal fees from WL Gore & Associates and Medtronic Ethicon, outside the submitted work. Dr. Dakin reports personal fees from Medtronic, outside the submitted work. Drs. Gray, Moore, Bellorin, Elmously, and Zarnegar have nothing to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Presented as a podium presentation at the annual Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) conference in March 2017
Rights and permissions
About this article
Cite this article
Gray, K.D., Moore, M.D., Elmously, A. et al. Perioperative Outcomes of Laparoscopic and Robotic Revisional Bariatric Surgery in a Complex Patient Population. OBES SURG 28, 1852–1859 (2018). https://doi.org/10.1007/s11695-018-3119-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3119-x