Abstract
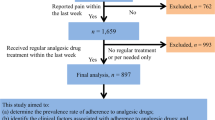
This study aimed to determine the relationship between the different factors of analgesic therapy and the compliance of chronic pain inpatients. We prospectively investigated 100 consecutive inpatients with noncancer chronic pain who were hospitalized to receive oral analgesic treatment in the Pain Department of West China Hospital from May 2013 to October 2013. Patients who completed the treatment plan were recorded as good compliance, whereas patients who partly completed or even refused the treatment were recorded as moderate or non-compliance, respectively. A total of 73 (73.7%), 17 (17.1%), and 9 (9.2%) patients showed good, moderate, and non-compliance, respectively. Univariate analyses showed significantly better compliance among farmers, patients educated in college or above, with family income of < 3000 CNY, and with severe or moderate pain than those employed and unemployed (P = 0.02), patients educated below college (P = 0.013), with family income of ≥ 3000 CNY (P = 0.025), and with mild pain (P < 0.001), respectively. Logistic regression analysis showed that the family income of ≥ 3000 CNY (OR: 2.50, 95%CI: 1.65–4.51, P = 0.021) and mild pain (OR: 1.27, 95%CI: 1.03–3.31, P = 0.016) were associated with moderate or non-compliance with oral analgesic treatment. In conclusion, the low compliance with oral treatment of analgesics was found in Chinese inpatients with chronic pain and compliance was negatively associated with family income and degree of pain of patients.
Similar content being viewed by others
References
Main CJ, Spanswick CC. Pain Management: an Interdisciplinary Approach. London: Churchill Livingstone (Parent company: Elsevier), 2001: 93
Institute of Medicine. Committees on Advancing Pain Research, Care, and Education. Relieving Pain in America: a Blueprint for Transforming Prevention, Care, Education, and Research Washington, DC: The National Academies Press, 2011
Yaksh TL, Wallace MS. Opioids, analgesia and pain management. In: Brunton LL, Chabner BA, Knollmann BC. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. New York, NY: McGraw-Hill, 2011: 481–525
Broekmans S, Dobbels F, Milisen K, Morlion B, Vanderschueren S. Medication adherence in patients with chronic non-malignant pain: is there a problem? Eur J Pain 2009; 13(2): 115–123
Passik SD, Kirsh KL, McDonald MV, Ahn S, Russak SM, Martin L, Rosenfeld B, Breitbart WS, Portenoy RK. A pilot survey of aberrant drug-taking attitudes and behaviors in samples of cancer and AIDS patients J Pain Symptom Manage 2000; 19(4): 274–286
Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, Weisner CM, Silverberg MJ, Campbell CI, Psaty BM, Von Korff M. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med 2010; 152(2): 85–92
Manchikanti L, Helm S, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV. Opioid epidemic in the United States Pain Physician 2012; 15(3 Suppl): ES9–ES38
Manchikanti L, Manchukonda R, Damron KS, Brandon D, McManus CD, Cash K. Does adherence monitoring reduce controlled substance abuse in chronic pain patients? Pain Physician 2006; 9(1): 57–60
tIves TJ, Chelminski PR, Hammett-Stabler CA, Malone RM, Perhac JS, Potisek NM, Shilliday BB, DeWalt DA, Pignone MP. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Serv Res 2006; 6(1): 46
Gilbert JW, Wheeler GR, Mick GE, Storey BB, Herder SL, Richardson GB, Watts E, Gyarteng-Dakwa K, Marino BS, Kenney CM, Siddiqi M, Broughton PG. Importance of urine drug testing in the treatment of chronic noncancer pain: implications of recent medicare policy changes in Kentucky. Pain Physician 2010; 13(2): 167–186
Zung WW. A rating instrument for anxiety disorders. Psychosomatics 1971; 12(6): 371–379
Berndt S, Maier C, Schütz HW. Polymedication and medication compliance in patients with chronic non-malignant pain. Pain 1993; 52(3): 331–339
Polatin PB, Kinney RK, Gatchel RJ, Lillo E, Mayer TG. Psychiatric illness and chronic low-back pain. The mind and the spine—which goes first? Spine 1993; 18(1): 66–71
Sagheer MA, Khan MF, Sharif S. Association between chronic low back pain, anxiety and depression in patients at a tertiary care centre. J Pak Med Assoc 2013; 63(6): 688–690
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, H., Zheng, Y., Gao, H. et al. Factors related to compliance with oral analgesic treatment of inpatients with chronic pain. Front. Med. 9, 374–379 (2015). https://doi.org/10.1007/s11684-015-0411-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11684-015-0411-1