Abstract
Background
Electronic consultation (eConsultation) offers a potential mechanism to increase access to specialty care, address knowledge gaps, and overcome therapeutic inertia in patients with type 2 diabetes (T2DM) being managed by primary care physicians (PCPs).
Objective
To develop and implement a system to provide unsolicited endocrinology eConsult for T2DM patients with HbA1c 8.5–10.5% managed by PCPs.
Design
Cluster-randomized matched cohort study with implementation evaluation.
Participants
PCPs affiliated with Massachusetts General Hospital (MGH).
Interventions
Unsolicited endocrinology eConsultation.
Main Measures
The primary clinical outcome was mean change in HbA1c at 6 months. Secondary process outcomes included referral completion rate, prescription rates of glucose-lowering medications, differences in rate of other management recommendations, change in all glucose-lowering medications, and number of face-to-face endocrinology visits.
Key Results
161 PCPs were randomly assigned to intervention (n=81) and control (n=80) arms. eConsultations were triggered on 130 patients from intervention arm PCPs. Intervention arm patients had a 0.89 (SD 1.45) decrease in HbA1c compared to 0.69 (SD 1.32) decrease in the control arm (p=0.28). There were significant differences in prescribing of glucose-lowering medications between arms. There was a 19.3% increase in patients prescribed GLP-1 RA or SGLT2i in the intervention arm compared to a 6.9% increase in control (p=0.003). There were also significant increases in prescription rates of metformin (3.1% vs −3.1%, p=0.03) and sulfonylureas (1.5% vs −6.9%, p=0.03). At 6-month follow-up, the intervention arm had 13 in-person endocrinology visits compared to 29 (p=0.012) in the control arm. PCPs were more likely to accept recommendations regarding adherence to or dose adjustment of current medications than initiation of new medications.
Conclusions
The implementation of an unsolicited endocrinology eConsult system for patients with poorly controlled T2DM is feasible. Unsolicited eConsultation was associated with increased prescribing of glucose-lowering medications without significant difference in HbA1c.
Trial Registration
Clinicaltrials.gov registration: NCT03542084
Similar content being viewed by others
BACKGROUND
Type 2 diabetes mellitus (T2DM) affects nearly 35 million people in the USA at an annual cost of approximately $240 billion [1]. Patients with T2DM are predominantly medically managed by a primary care physician (PCP) [2]. As the prevalence of diabetes continues to rise, PCPs are under continued pressure to achieve glycemic targets while also adopting rapidly changing standards of care [3]. Nationally, T2DM patients are not achieving recommended care goals [4]. Failure to achieve these targets has been associated with increased clinical complications and cost of care [5]. Additionally, three major classes of glucose-lowering medications and several new insulin formulations have been approved over the last 15 years, with major revisions of guidelines for management of hyperglycemia in T2DM, greatly increasing the complexity of pharmacologic management [6]. Though the newer classes of medications offer benefits such as weight loss, kidney protection, and cardiovascular risk reduction in appropriate subpopulations when compared with older agents, uptake of the new guidelines in primary care can be slow and endocrinologists are disproportionately more likely to prescribe these agents compared to PCPs [6,7,8]. Unfortunately, access to specialty care is limited, with only 7,681 board-certified adult endocrinologists currently in practice in the USA with a gap of approximately 1500 endocrinologists projected by 2025 [9].
Over the past decade, electronic consultation (eConsult) has emerged as a safe, new delivery model with potential to improve access to specialty care [10]. eConsults are asynchronous peer-to-peer consultations that require review of the electronic health record followed by clinical documentation of recommendations. eConsults are generally well received by patients and physicians, with increased uptake across health systems [11]. As such, they offer a potential mechanism to address knowledge gaps and overcome therapeutic inertia, defined as the delay of an indicated change in therapy, in many conditions managed by PCPs, including T2DM. Further evaluation is needed to understand and optimize the impact of endocrinology eConsults on key quality indicators.
One way to potentially optimize the impact of eConsults at a population level is to provide unsolicited eConsultation for patients based on pre-determined clinical criteria without requiring any action from PCPs. To that end, we developed and implemented a system to provide an endocrinology eConsult for patients with T2DM with HbA1c 8.5–10.5% being cared for by PCPs across a large primary care network affiliated with Massachusetts General Hospital (MGH). To evaluate this strategy, we randomized PCPs into treatment (HbA1c-triggered eConsult) and control (standard of care) arms and studied process, clinical, and implementation outcomes.
METHODS
Setting
MGH is a large, urban, academic medical center with 24 affiliated primary care practices caring for approximately 190,000 adult patients. At the time of intervention, there was a robust eConsult program in place in which PCPs could elect to request eConsults across the majority of specialty services at MGH, including diabetes [12].
Participants
Eligible patients were <81 years of age, had an HbA1c 8.5–10.5% within 9 months, had a PCP visit within 14 months, and had no prior visit to an MGH endocrinologist within 2 years or any record of a solicited endocrinology eConsult as of August 2018 when the study cohort was identified. There were no other pre-specified exclusion criteria.
All attending and resident PCPs caring for eligible adult patients at MGH-affiliated practices at the time the study cohort was identified were randomized into intervention (eConsultation) and control (usual care) arms. Patients cared for by a resident PCP were attributed only to that resident PCP for the purpose of this analysis. Intervention arm PCPs were informed via electronic communication through the medical record and automatically received unsolicited endocrinology eConsults for their patients who met pre-specified inclusion criteria. PCPs in both arms could continue to actively request eConsults via the pre-existing eConsult program.
Study Design
A stepwise protocol was created to identify and screen potential patients, trigger endocrinology eConsultation, collect specialty recommendations, and track pre-specified outcomes of interest (Figure 1). The list of eligible patients was generated in August 2018 using EHR data. In the unsolicited eConsult arm, after initial review to confirm that the patient’s most recent HbA1c remained within the study inclusion criterion of 8.5–10.5%, a research coordinator sent an eConsult to one of three MGH staff endocrinologists at a rate of approximately 3–5 eConsults per endocrinologist per week. Reviewing endocrinologists could exclude a patient if the consult was deemed to be clinically inappropriate or information was insufficient to perform an unsolicited eConsult. Endocrinology consultants completed and formulated management recommendations based only on EHR chart review utilizing a standardized note template (Appendix Figure 1 in the Supplementary Information). They were paid $52 per eConsult, as per the standard eConsult reimbursement rate within the organization. Endocrinologists documented as a formal electronic consultation note in the medical record and routed this note to the PCP as a clinical message within the EHR. The PCP was ultimately responsible for accepting recommendations as they deemed appropriate and could elect to engage the eConsultant in ongoing electronic communication. Unsolicited eConsultations were performed between September 2018 and June 2019. Clinicians randomly assigned to the control arm continued to provide usual standard of care. Clinicians in both arms had the option to seek endocrinology consultation (either electronic or face-to-face) through usual care. Due to the nature of the intervention, study investigators and consulting endocrinologists were not blinded. The Mass General Brigham Institutional Review Board approved this protocol, including a waiver of patient informed consent. The trial was registered through Clinicaltrials.gov (NCT03542084).
Main Measures
We collected demographic and clinical data for all patients both at the time of eConsult and at 6-month follow-up. The primary clinical outcome was mean change in HbA1c 6 months after the date of eConsult completion (the same target dates were used for the corresponding matched control). We also evaluated A1c change at 12- and 18-month follow-up. Secondary process outcomes included referral completion rate (and reasons for non-completion or exclusion) and time to eConsultation, changes in glucose-lowering medications at 6 months, count, type, and implementation rate of management recommendations as well as the number of face-to-face endocrinology visits in each arm. We evaluated seven classes of glucose-lowering medications: metformin, sulfonylurea, DPP4 inhibitor, GLP-1 receptor agonist (GLP-1 RA), SGLT2 inhibitor (SGLT2i), insulin, and others. We also evaluated the differences in prescribing of a combined category of “newer classes” which included both GLP-1 RA and SGLT2i. Process measures were collected by chart review. PCPs in the intervention group who did not implement the eConsult recommendations received an electronic survey to better understand the reasons eConsult recommendations were not implemented.
Statistical Analysis
Due to the lag-time from list generation to unsolicited eConsult generation in a large proportion of the patients, the initial randomization did not provide a true contemporaneous control arm. Post-randomization exclusion from the intervention arm only also undermined the randomization. Therefore, patients who received an eConsult were matched 1:1 with patients from the control group of PCPs. Matching variables were age (within 10 years), sex, most recent PCP visit date within 90 days, and baseline HbA1c within 0.5. We compared change in HbA1c at baseline and 6 months between intervention and control arm matched patients by testing the group and time interaction in a linear regression model using the generalized estimating equations (GEE) approach to account for repeated measures. When limited to those with data available for both subjects in a pair, we used a paired t-test to compare changes. We compared rates of change in medication use at 6 months, focusing on newer glucose-lowering medications that were less familiar to PCPs, using the same GEE approach with logistic regression models. We estimated that with at least 97 patients in each arm, the study would have 90% power to detect a 0.5 between-group difference in HbA1c from a paired t-test, assuming a standard deviation of 1.5.
RESULTS
In total, 161 primary care providers were randomly assigned to intervention (n=81) and control (n=80) arms. The age range of patients enrolled was 26–80 years old. Intervention providers had 275 eligible patients based on the pre-specified inclusion criteria. Of those 275 patients, 145 (53%) were excluded from the study after eligibility review or initial endocrinologist chart review (Figure 2). The median time to eConsult was 94 days (IQR 59–147) from EHR list generation and 6 (IQR 1–8) days from the eConsult order. The most common reasons for exclusion included improvement in HbA1c following randomization (n=60, 22%), recent medication change by the PCP as part of usual care (n=43, 30%), current endocrinology consultation at another institution (n=15, 10%), and concerns regarding patient appropriateness based on engagement, adherence, or comorbidities (n=6; 4%).
eConsultations were completed by endocrinologists on the remaining 130 (47%) patients. All unsolicited eConsultations were reviewed by the PCP of record. After these 130 intervention patients were matched 1:1 with patients from control arm PCPs, there were only minimal differences in baseline characteristics between the two groups (Table 1).
There was no difference in the primary outcome of glycemic control between the intervention and matched control arm patients. Among all patients with 6-month follow-up HbA1c data, patients in the intervention group (n=113) had a mean HbA1c decrease of 0.83 (SD 1.41). Patients in the control group (n=112) had a mean HbA1c decrease of 0.72 (SD 1.41) (p=0.52) (Table 2). Similarly, there was no difference at 12 (−0.75 vs −0.68, p=0.74) and 18 (−0.85 vs −0.88, p=0.91) months of follow-up. There were 98 matched pairs of intervention and control patients with 6-month follow-up data available. Among matched pairs, patients in the intervention group had a 0.89 (SD 1.45) decrease in HbA1c and patients in the control group had a 0.69 (SD 1.32) decrease in HbA1c (p=0.28). At 12 (n=78 pairs) and 18 (n=39 pairs) months, there was also no difference in mean HbA1c change (−0.83 vs −0.62, p=0.36; −0.89 vs −0.78, p=0.76).
Secondary outcomes revealed significant differences in prescribing patterns between the two arms. The most commonly prescribed medications at baseline and at 6 months were metformin and insulin in both study arms (Table 3). Compared to baseline, at 6-month follow-up, 2.3% of intervention group patients had a reduction in the number of glucose-lowering agents prescribed, 71.5% had the same, and 26.2% had an increase. This is compared to the control group in which 14.6% of patients had a reduction in the number of glucose-lowering agents prescribed, 72.3% had the same, and 13.1% had an increase (p<0.001). Patients in the intervention arm had a statistically significant increase in prescription rates of both metformin (3.1% vs −3.1%, p=0.03) and a sulfonylurea (1.5% vs −6.9%, p=0.03) compared to controls.
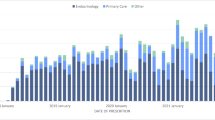
In our analysis examining frequency of prescribing “newer classes” of medications, there was a 19.3% increase in the use of newer classes of GLP-1 RA and SGLT2i medications that reduce cardiac and renal risk in patients with diabetes in the intervention group compared to a 6.9% increase in the control group (p=0.003) (Figure 3). This was driven mostly by a significant increase in prescription rates for SGLT2i in the intervention group compared to control (12% vs 2%, p=0.005).
There were 211 discrete management recommendations made in the 130 eConsultations; however, only 80 (38%) of those recommendations were implemented by primary care providers during the 6-month intervention follow-up period. The most common recommendations were addition of a new medication (n=131) and dose adjustment of an existing medication (n=45), with implementation rates of only 28% and 53%, respectively. In the control arm, there were 113 discrete management changes made by PCPs (Appendix Table 1 in the Supplementary Information). When we evaluated the sub-group of patients whose recommendations were implemented, there was still no difference in HbA1c change at 6-, 12-, or 18-month follow-up (Appendix Table 2 in the Supplementary Information).
We queried PCPs to determine why recommendations were not accepted. The most common barrier noted was that the patient had not returned to the office since the eConsult was performed. Other barriers included disagreement with the recommendation, lack of familiarity with the medications recommended, desire to recheck HbA1c or try lifestyle change before adopting, or patient refusal. PCPs additionally requested help with prior authorizations and education regarding new classes of medications.
At 6-month follow-up, the intervention arm had 13 subsequent in-person endocrinology visits compared to 29 in the control arm (p=0.012). Both the intervention arm and control arm had 4 solicited eConsults (p=0.99).
CONCLUSION
The implementation of an unsolicited endocrinology eConsult system for patients with poorly controlled type 2 diabetes is feasible. In our health system, an unsolicited eConsultation program did not result in a clinically significant change in mean HbA1c at 6, 12, or 18 months. One potential reason for this null result is that only 38% of recommendations made by endocrinologists were ultimately adopted by PCPs. Adoption was even lower (28%) when endocrinologists recommended the addition of a new medication. Many of the barriers to acceptance of recommendations provided in the unsolicited eConsults could be addressed by adapting the intervention design to increase provider engagement and knowledge.
Unsolicited eConsultation did lead to improvements in a number of secondary process outcomes. First, patients of PCPs randomly assigned to the eConsultation arm had significant increase in overall glucose-lowering medication use compared to the control arm suggesting that eConsultation may be one strategy to combat therapeutic inertia. Given that this was a population of patients with suboptimal glycemic control, an increase in medication prescription was likely to be clinically appropriate. Additionally, patients in the intervention arm experienced an increase in the prescription rates for newer diabetes medications, including SGLT2i and GLP1-RA, concordant with more recent guidelines [6, 13]. While we did not see a corresponding change in HbA1c, both these classes of medications have increasingly been shown to have important renovascular benefits independent of the glycemic effect [14].
Second, as hypothesized, we observed fewer in-person endocrinology visits in the intervention arm (13) compared to the control arm (29). One important way that eConsultation has the potential to increase access to specialty care is by allowing ongoing management of patients in the primary care setting who would otherwise have been referred to a specialist, thereby decreasing inappropriate referrals [15]. Prior studies have indicated that interventions such as academic detailing or clinical decision support are not effective at promoting changes in chronic disease patient management. Therefore, we chose to study whether an unsolicited, individualized peer-to-peer eConsult would be an effective way to impact care.
Our study had several limitations. First, we had a relatively small sample size which was in part driven by a high percentage (53%) of patients who, despite meeting pre-specified inclusion criteria, were excluded from the analysis most commonly due to outdated HbA1c values or recent therapeutic changes made by the PCP. This occurred in part due to a flaw in our study design in which patient eligibility for unsolicited eConsultation was determined at a single timepoint. Unsolicited eConsultations took our consulting endocrinologists longer than anticipated to complete, and as a result the lag from list generation to completion of the eConsultation was 94 days. In future iterations, we will aim to identify and randomize patients on a rolling basis and immediately trigger eConsults in real time (i.e., within 2 weeks of an HbA1c measurement) to allow consultants to provide more salient guidance and ensure recommendations are delivered at a moment when the PCP is already considering management changes. Second, this is a study of patients at a single, urban academic medical center and as such, the results may not be broadly generalizable.
The implementation of an unsolicited eConsult program requires certain structural and administrative capabilities. There must be an existing robust EHR with traditional eConsultation capabilities and a diabetes clinical registry that can be used for real-time case finding. A centralized team of specialty and primary care providers as well as population health leadership is needed to develop clinical algorithms and workflows. Information technology and support staff are essential to develop a smooth operational experience for providers and to offer support for recommendation implementation. Finally, mechanisms should be in place to collect and analyze process and outcome measures to allow for real-time, iterative quality improvement efforts.
In summary, unsolicited electronic consultation represents a novel care delivery tool. While implementation of such a program is feasible, it did not result in a clinically significant decrease in HbA1c compared to matched controls. Improvements in secondary process outcomes suggest the potential of this tool to improve care for patients with T2DM with improvements in program design and implementation. Additional research and process improvement efforts focused on unsolicited endocrinology eConsult programs are required to better understand and address this gap in diabetes care.
References
American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-928.
Davidson JA. The increasing role of primary care physicians in caring for patients with type 2 diabetes mellitus. Mayo Clin Proc. 2010;85(Suppl. 12):S3–S4
O’Connor PJ, Bodkin NL, Fradkin J, et al. Diabetes Performance Measures: Current Status and Future Directions. Diabetes Care. 2011; 34(7): 1651-1659.
Kazemian P, Shebl FM, McCann N, Walensky RP, Wexler DJ. Evaluation of the Cascade of Diabetes Care in the United States, 2005-2016. JAMA Intern Med. 2019;179(10):1376–1385. doi:https://doi.org/10.1001/jamainternmed.2019.2396
Giugliano D, Maiorino MI, Bellastella G et al. Glycemic Control, Preexisting Cardiovascular Disease, and Risk of Major Cardiovascular Events in Patients with Type 2 Diabetes Mellitus: Systematic Review With Meta-Analysis of Cardiovascular Outcome Trials and Intensive Glucose Control Trials. J Am Heart Assoc. 2019 8;e012356
American Diabetes Association. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S111-S124.
McCoy RG, Dykhoff HJ, Sangaralingham L, et al. Adoption of New Glucose-Lowering Medications in the U.S.-The Case of SGLT2 Inhibitors: Nationwide Cohort Study. Diabetes Technol Ther. 2019;21(12):702-712.
Dave CV, Schneeweiss S, Wexler DJ, Brill G, Patorno E. Trends in Clinical Characteristics and Prescribing Preferences for SGLT2 Inhibitors and GLP-1 Receptor Agonists, 2013-2018. Diabetes Care. 2020;43(4):921-924.
The Lewin Group. Endocrine clinical workforce: supply and demand projections. The Endocrine Society. June 2014. https://www.endocrine.org/-/media/endosociety/files/advocacy-and-outreach/other-documents/2014-06-white-paper%2D%2Dendocrinology-workforce.
Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (eConsults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323-30.
Larson A, Wheeler J. E-Consult Innovation: A Middle-Ground Model To Enhance Adoption and Improve Care. NEJM Catalyst. 1(6). https://doi.org/10.1056/CAT.20.0032
Wasfy JH, Rao SK, Essien UR, Richardson CA, Jeune T, Goldstein SA, Laikhter E, Chittle MD, Weil M, Wein M, Ferris TG. Initial experience with endocrinology e-consults. Endocrine. 2017; 55(2):640-642.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669-2701.
Das SR, Everett BM, Birtcher KK, Brown JM, Januzzi JL Jr, Kalyani RR, Kosiborod M, Magwire M, Morris PB, Neumiller JJ, Sperling LS. 2020 Expert Consensus Decision Pathway on Novel Therapies for Cardiovascular Risk Reduction in Patients With Type 2 Diabetes: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2020;76(9):1117-1145. doi: https://doi.org/10.1016/j.jacc.2020.05.037. Epub 2020 Aug 5. PMID: 32771263; PMCID: PMC7545583.
Vimalananda VG, Gupte G, Seraj SM, Orlander J, Berlowitz D, Fincke BG, Simon SR. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323-30. doi: https://doi.org/10.1177/1357633X15582108. Epub 2015 May 20.
Funding
This work was supported by funding from the division of General Internal Medicine at Massachusetts General Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
DJW reports serving on Data Monitoring Committees for Novo Nordisk.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Andrew S. Oseran and Karthik Rao contributed equally to this work. Deborah J. Wexler and Daniel M. Horn contributed equally to this work.
Supplementary Information
ESM 1
(DOCX 36 kb)
Rights and permissions
About this article
Cite this article
Oseran, A.S., Rao, K., Chang, Y. et al. HbA1c-Triggered Endocrinology Electronic Consultation for Type 2 Diabetes Management. J GEN INTERN MED 37, 1081–1087 (2022). https://doi.org/10.1007/s11606-021-07157-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07157-x