ABSTRACT
Background
Hypertension is a major risk factor for peripheral artery disease (PAD). Little is known about relative efficacy of antihypertensive treatments for preventing PAD.
Objectives
To compare, by randomized treatment groups, hospitalized or revascularized PAD rates and subsequent morbidity and mortality among participants in the Antihypertensive and Lipid-Lower Treatment to Prevent Heart Attack Trial (ALLHAT).
Design
Randomized, double-blind, active-control trial in high-risk hypertensive participants.
Participants
Eight hundred thirty participants with specified secondary outcome of lower extremity PAD events during the randomized phase of ALLHAT.
Interventions/events
In-trial PAD events were reported during ALLHAT (1994–2002). Post-trial mortality data through 2006 were obtained from administrative databases. Mean follow-up was 8.8 years.
Main Measures
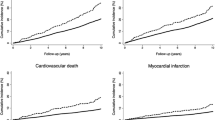
Baseline characteristics and intermediate outcomes in three treatment groups, using the Kaplan-Meier method to calculate cumulative event rates and post-PAD mortality rates, Cox proportional hazards regression model for hazard ratios and 95 % confidence intervals, and multivariate Cox regression models to examine risk differences among treatment groups.
Key Results
Following adjustment for baseline characteristics, neither participants assigned to the calcium-channel antagonist amlodipine nor to the ACE-inhibitor lisinopril showed a difference in risk of clinically advanced PAD compared with those in the chlorthalidone arm (HR, 0.86; 95 % CI, 0.72–1.03 and HR, 0.98; 95 % CI, 0.83–1.17, respectively). Of the 830 participants with in-trial PAD events, 63 % died compared to 34 % of those without PAD; there were no significant treatment group differences for subsequent nonfatal myocardial infarction, coronary revascularizations, strokes, heart failure, or mortality.
Conclusions
Neither amlodipine nor lisinopril showed superiority over chlorthalidone in reducing clinically advanced PAD risk. These findings reinforce the compelling need for comparative outcome trials examining treatment of PAD in high-risk hypertensive patients. Once PAD develops, cardiovascular event and mortality risk is high, regardless of type of antihypertensive treatment.




Similar content being viewed by others
REFERENCES
Murabito JM, D’Agostino RB, Silbershatz H, Wilson WF. Intermittent claudication. A risk profile from the Framingham Heart Study. Circulation. 1997;96:44–49.
Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2004;110:738–743.
Bozkurt AK, Tasci I, Tabak O, Gumus M, Kaplan Y. Peripheral artery disease assessed by ankle-brachial index in patients with established cardiovascular disease or at least one risk factor for atherothrombosis–CAREFUL study: a national, multi-center, cross-sectional observational study. BMC Cardiovasc Disord. 2011;11:4.
Meijer WT, Grobbee DE, Hunink MGM, Hofman A, Hoes AW. Determinants of peripheral arterial disease in the elderly: the Rotterdam study. Arch Intern Med. 2000;160:2934–2938.
Criqui MH, Denenberg JO. The generalized nature of atherosclerosis: how peripheral arterial disease may predict adverse events from coronary artery disease. Vasc Med. 1998;3:241–245.
Hirsch AT, Hartman L, Town RJ, Virnig BA. National health care costs of peripheral arterial disease in the Medicare population. Vasc Med. 2008;13:209–215.
Antonopoulos S, Kokkoris S, Stasini F, et al. High prevalence of subclinical peripheral artery disease in Greek hospitalized patients. Eur J Intern Med. 2005;16:187–191.
Cacoub PP, Abola MT, Baumgartner I, et al. REACH Registry Investigators. Cardiovascular risk factor control and outcomes in peripheral artery disease patients in the REduction of Atherothrombosis for Continued Health (REACH) registry. Atherosclerosis. 2009;204:e86–e92.
Clement DL, De Buyzere ML, Duprez DA. Hypertension in peripheral arterial disease. Curr Pharm Des. 2004;10:3615–3620.
De Buyzere ML, Clement DL. Management of hypertension in peripheral arterial disease. Prog Cardiovasc Dis. 2008;50:238–263.
Singer DR, Kite A. Management of hypertension in peripheral arterial disease: does the choice of drugs matter? Eur J Vasc Endovasc Surg. 2008;35:701–708.
Lauer MS. Comparative effectiveness research: the view from the NHLBI. J Am Coll Cardiol. 2009;53:1084–1086.
Matchar DB, McCrory DC, Orlando LA, et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Ann Intern Med. 2008;148:16–29.
Sciarretta S, Palano F, Tocci G, Baldini R, Volpe M. Antihypertensive treatment and development of heart failure in hypertension: a Bayesian network meta-analysis of studies in patients with hypertension and high cardiovascular risk. Arch Intern Med. 2011;171:384–394.
Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive And Lipid-Lowering Treatment To Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–2997.
Cushman WC, Davis BR, Pressel SL, ALLHAT Collaborative Research Group, et al. Mortality and morbidity during and after the Antihypertensive And Lipid-Lowering Treatment To Prevent Heart Attack Trial. J Clin Hypertens (Greenwich). 2012;14:20–31.
The fifth report of the Joint National Committee On Detection. Evaluation, and treatment of high blood pressure (JNC V). Arch Int Med. 1993;153:154–183.
Davis BR, Cutler JA, Gordon DJ, et al. Rationale and design for the Antihypertensive And Lipid-Lowering Treatment To Prevent Heart Attack Trial (ALLHAT). Am J Hypertens. 1996;9:342–360.
Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial Collaborative Research Group. Diuretic versus alpha-blocker as first-step antihypertensive therapy: final results from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension. 2003;42:239–246.
Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial Protocol. Available at: https://allhat.sph.uth.tmc.edu/Forms/protocol.pdf. Accessed April 28, 2014
Klein JP, Moeschberger ML. Survival Analysis: Techniques for Censored and Truncated Regression. 2nd ed. New York, NY: Springer; 2003.
Stafylas PC, Sarafidis PA. Carvedilol in hypertension treatment. Vasc Health Risk Manag. 2008;4:23–30.
Espinola-Klein C, Weisser G, Jagodzinski A, et al. ß-Blockers in patients with intermittent claudication and arterial hypertension: results from the nebivolol or metoprolol in arterial occlusive disease trial. Hypertension. 2011;58:148–154.
Bavry AA, Anderson RD, Gong Y, et al. Outcomes among hypertensive patients with concomitant peripheral and coronary artery disease: findings from the INternational VErapamil-SR/Trandolapril STudy. Hypertension. 2010;55:48–53.
Hirsch AT, Duprez D. The potential role of angiotensin-converting enzyme inhibition in peripheral arterial disease. Vasc Med. 2003;8:273–278.
Coppola G, Romano G, Corrado E, Grisanti RM, Novo S. Peripheral artery disease: potential role of ACE-inhibitor therapy. Vasc Health Risk Manag. 2008;4:1179–1187.
Ostergren J, Sleight P, Dagenais G, et al. HOPE study investigators. Impact of ramipril in patients with evidence of clinical or subclinical peripheral arterial disease. Eur Heart J. 2004;25:17–24.
Ahimastos AA, Lawler A, Reid CM, Blombery PA, Kingwell BA. Brief communication: ramipril markedly improves walking ability in patients with peripheral arterial disease: a randomized trial. Ann Intern Med. 2006;144:660–664.
Gey DC, Lesho EP, Manngold J. Management of peripheral arterial disease. Am Fam Physician. 2004;69:525–532.
Hirsch AT, Haskal ZJ, Hertzer NR, American Association for Vascular Surgery, Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, ACC/AHA Task Force on Practice Guidelines, American Association of Cardiovascular and Pulmonary Rehabilitation, National Heart, Lung, and Blood Institute, Society for Vascular Nursing, TransAtlantic Inter-Society Consensus, Vascular Disease Foundation, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary. J Am Coll Cardiol. 2006;47:1239–1312.
Gregg EW, Sorlie P, Paulose-Ram R, Gu Q, Eberhardt MS, Wolz M, Burt V, Curtin L, Engelgau M, Geiss L. 1999–2000 National Health And Nutrition Examination Survey. Prevalence of lower-extremity disease in the US adult population >=40 years of age with and without diabetes: 1999–2000 National Health And Nutrition Examination Survey. Diabetes Care. 2004;27:1591–1597.
Extension Protocol: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Available at: https://allhat.sph.uth.tmc.edu/Forms/ExtensionProtocol.pdf. Accessed April 28, 2014
Cimminiello C, Borghi C, Kownator S, PANDORA Study Investigators, et al. Prevalence of peripheral arterial disease in patients at non-high cardiovascular risk Rationale and design of the PANDORA study. BMC Cardiovasc Disord. 2010;10:35.
Dawson DL, Hiatt WR, Creager MA, Hirsch AT. Peripheral arterial disease: medical care and prevention of complications. Prev Cardiol. 2002;5:119–130.
ACKNOWLEDGMENTS
The authors thank Dr. Ellen Breckenridge, The University of Texas School of Public Health, for editorial assistance in the preparation of this manuscript.
Funding
This research was supported by contracts NO1-HC-35130 and HHSN268201100036C from the National Heart, Lung, and Blood Institute. The ALLHAT investigators acknowledge contributions of study medications supplied by Pfizer, Inc. (amlodipine and doxazosin), AstraZeneca (atenolol and lisinopril), and Bristol-Myers Squibb (pravastatin) and financial support provided by Pfizer, Inc.
Prior Presentations
None
Conflict of Interest
Dr. Basil has received honoraria from Daiichi Sankyo and Takeda.
Dr. Probstfield has received research support from GlaxcoSmithKline and Sanofi Aventis.
Dr. Rahman has received honoraria from Boehringer Ingelheim.
Drs. Baraniuk, Dart, Davis, Ellsworth, Fendley, Habib, Piller, Simpson, and Whelton have no financial interests to disclose.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Clinical Trial Registration
www.clinicaltrials.gov NCT00000542
For a complete list of members of the ALLHAT Collaborative Research Group, see JAMA 2002;288:2981–2997.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 533 kb)
Rights and permissions
About this article
Cite this article
Piller, L.B., Simpson, L.M., Baraniuk, S. et al. Characteristics and Long-Term Follow-Up of Participants with Peripheral Arterial Disease During ALLHAT. J GEN INTERN MED 29, 1475–1483 (2014). https://doi.org/10.1007/s11606-014-2947-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2947-1