Abstract
BACKGROUND AND OBJECTIVE
It is unknown whether testing HIV-infected individuals for hepatitis C virus (HCV) and informing them of their HCV status impacts subsequent alcohol use. We hypothesized that HIV-infected individuals with current or past alcohol problems who reported being told they had HCV were more likely to 1) abstain from alcohol and 2) not drink unhealthy amounts compared to individuals who had not been told.
DESIGN, PARTICIPANTS, AND MEASUREMENTS
Data from a prospective, observational cohort study (HIV-Longitudinal Interrelationships of Viruses and Ethanol) were used to assess the association between awareness of having HCV at baseline and subsequent abstinence and not drinking unhealthy amounts as reported at 6-month follow-up intervals. General estimating equations logistic regression was used to account for the correlation from using repeated observations from the same subject over time. We adjusted for age, sex, race, homelessness, injection drug use, depressive symptoms, and having abnormal liver tests.
RESULTS
Participants who reported being told they had HCV were more likely to report abstaining from alcohol (AOR = 1.60; 95% CI: 1.13 to 2.27) and not drinking unhealthy amounts (AOR = 1.46; 95% CI: 1.01 to 2.11).
CONCLUSIONS
Among patients infected with HIV who had a history of alcohol problems, reporting being told one had HCV was associated with greater abstinence from alcohol and less unhealthy amounts of drinking.
Similar content being viewed by others
BACKGROUND
Because of overlapping risk factors, approximately 30% of individuals with HIV are co-infected with hepatitis C virus (HCV).1 Alcohol and HIV infection are both associated with more rapid progression of HCV-related liver disease;2,3 therefore, it is recommended that all patients with HCV, and in particular those who are co-infected with HIV/HCV, abstain from or at least moderate their alcohol use.4 It is unknown whether patients with HIV who use alcohol change their behavior in response to being diagnosed with HCV.
We examined the effect of reporting being told one had HCV on drinking in a cohort of patients with HIV and a history of alcohol problems, hypothesizing that patients who reported being told they had HCV were more likely to have reduced alcohol consumption compared to individuals who had not been told.
METHODS
Design
Data were from a prospective, observational cohort study (HIV-Longitudinal Interrelationships of Viruses and Ethanol [HIV-LIVE]) in which assessments occurred at 6-month intervals over a maximum of 42 months.
Subjects
Recruitment occurred from a previous cohort study, an intake clinic for HIV-infected patients, HIV primary care and specialty clinics, homeless shelters, drug treatment programs, subject referrals, and flyers. Enrollment occurred between August 2001 and July 2003.
Eligibility criteria were as follows: 1) documented HIV antibody test by ELISA and confirmed by Western blot; 2) 2 or more affirmative responses to the CAGE alcohol screening questionnaire5,6 or physician investigator diagnosis of alcoholism; 3) ability to speak English or Spanish. Exclusion criteria included: 1) scoring <21 on the 30-item Folstein Mini-Mental State Examination7,8 and 2) inability to provide informed consent. The Institutional Review Boards of Boston Medical Center and Beth Israel Deaconess Medical Center approved this study.
Outcomes
The two outcomes of interest were abstinence and not drinking unhealthy amounts in the past 30 days. At each 6-month study visit past-month alcohol consumption was assessed using a validated calendar method (Alcohol timeline followback).9 Abstinence was defined as no drinks in the past 30 days. Unhealthy drinking amounts were defined as: 1) greater than 14 standard drinks per week, or greater than 4 drinks on occasion for men, or 2) greater than 7 drinks in the past week or greater than 3 drinks on occasion for women.10
Independent Variables
The primary independent variable was awareness of HCV diagnosis. This was defined as a positive response to the question “Has a doctor ever told you that you had hepatitis C?” which was queried at study entry only. A negative response could either mean that a patient had been tested and told he/she did not have hepatitis C, or that he/she was never tested.
Additional covariates were self-reported age, sex, race, recent (in the past 6 months) homelessness, recent injection drug use, depressive symptoms, and having abnormal liver enzymes. Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression scale (CES-D),11 and a threshold of ≥16 was used to define a higher level of depressive symptoms. Secondary analyses used information on chronic infection as determined by HCV RNA levels on polymerase chain reaction (PCR) testing.
Statistical Analysis
Chi-square and Student’s t tests were used to compare baseline characteristics of subjects who reported being told by a doctor they had hepatitis C compared to those who did not report being told. General estimating equations (GEE) logistic regression was used to calculate odds ratios and 95% confidence intervals, adjusting for other covariates. The GEE approach was used to account for the correlation from using repeated observations from the same subject over time. An exchangeable working correlation structure was used and empirical standard errors are reported for all analyses. Collinearity of covariates was assessed by calculating the correlation between independent variables and no pair of variables had a correlation >0.40. A two-tailed p value <0.05 was considered statistically significant for all hypothesis testing. To assess whether the effect of being told was 1) independent from having actual infection and 2) did not differ by actual infected status, we did secondary analyses adjusting for and stratifying by HCV RNA status (detectable vs undetectable). We also performed additional analyses, adjusting for site of recruitment. Analyses were performed using SAS software (version 9.1; SAS Institute, Cary, NC, USA).
RESULTS
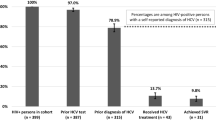
The study sample was comprised of 400 participants, of which 211 (53%) reported being told by a physician that they had hepatitis C. The latter patients were more likely to be older, female, homeless, currently using injection drugs, have more depressive symptoms, and have abnormal liver enzymes (Table 1).
At baseline, 64% of patients who were told they had hepatitis C reported abstinence from alcohol versus 52% of patients who were never told they had hepatitis C (p value = 0.02). Fewer individuals who had been told they had hepatitis C reported drinking unhealthy amounts (27% told vs 36% never told, p value = 0.09).
The median follow-up time for patients was 18 months. Reporting being told one had hepatitis C was positively associated with abstinence and not drinking unhealthy amounts in multivariable logistic regression models (Table 2). Participants who reported being told they had hepatitis C had approximately one and a half times the odds of abstaining from alcohol and not drinking unhealthy amounts compared to participants who had not been told they had hepatitis C (AOR for abstinence = 1.60; 95% CI: 1.13 to 2.27; AOR for no unhealthy alcohol use = 1.46; 95% CI: 1.01 to 2.11). Secondary analyses adjusting for recruitment site produced similar results (data not shown).
Most (396) of the 400 study subjects had HCV RNA test results available. Of the individuals who had been told they had HCV, 85% had detectable HCV RNA; of those never told they had HCV, 88% had undetectable HCV RNA. Adjusting for HCV RNA did not attenuate the impact of being told of HCV infection on abstinence (AOR = 1.59, 95% CI: 0.98 to 2.58) or not drinking unhealthy amounts (AOR = 1.56, 95% CI: 0.79 to 3.1), thus it appeared the effect of being told was independent of actual infection. Also, the effect of being told did not differ by status of HCV RNA: odds ratios were similar and confidence intervals overlapped.
DISCUSSION
Among patients infected with HIV who had current or past alcohol problems, reporting being told one had hepatitis C was associated with greater odds of abstaining from alcohol and a lower odds of drinking unhealthy amounts. The results from a secondary analysis suggest that it is being told of one’s hepatitis C diagnosis, rather than actually having infection, that is linked to the effect on drinking. This finding is clinically relevant, as it gives indirect support to the hypothesis that telling patients that they have HCV may lead to less unhealthy alcohol use, which in turn can impact long-term outcomes among patients who are co-infected with HIV and HCV.
Our findings appear to be consistent with limited prior research. A study of HIV positive veterans also found a higher rate of abstinence among patients who were co-infected with HCV (based on antibody testing) compared to patients with HIV alone.12 Studies in other populations not specifically HIV-infected have been mixed, finding either less alcohol use for those aware of their HCV status or no effect.13–16
Although the absolute difference in abstinence and unhealthy use between the 2 groups was modest, these differences could nonetheless translate into substantial gains on a population level. Approximately 4 million Americans—1.6% of the population—are believed to be infected with HCV.17 It is estimated that 5–20% of those infected will develop cirrhosis after 20 years; once diagnosed with cirrhosis, the risk of developing hepatocellular cancer may be 1–4% per year.4,18 Heavy alcohol use has a synergistic affect with HCV infection and greatly increases the odds of developing cirrhosis and liver cancer.19,20 Therefore, if screening and notifying individuals of their HCV positive status leads to even modest improvements in alcohol use, a substantial number of individuals might avert liver complications.
This study has several important limitations. We did not assess whether patients received advice about their drinking so we cannot determine whether patients changed their behavior in response to physician counseling. Drinking was based on participants’ self-report; despite using a validated tool and assuring confidentiality, patients who were told they had hepatitis C and were aware that they should not be drinking may have been more likely to misrepresent their alcohol use (social desirability bias). Finally, although we adjusted for confounders, there may have been residual confounding.
Among a cohort of HIV-infected individuals with current or past alcohol problems, reporting being told that one had hepatitis C was associated with greater abstinence and less unhealthy amounts of drinking. Testing HIV-infected patients for HCV and informing them of their status may lead them to drink less, and thus reduce their likelihood of developing HCV-associated liver disease.
References
Alter MJ. Epidemiology of viral hepatitis and HIV co-infection. J Hepatol. 2006;44:S6–9.
Peters MG, Terrault NA. Alcohol use and hepatitis C. Hepatology. 2002;36:S220–5.
Sulkowski MS, Thomas DL. Hepatitis C in the HIV-infected person. Ann Intern Med. 2003;138:197–207.
Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. Centers for Disease Control and Prevention. Morb Mort Wkly Rep Recomm Rep. 1998;47:1–39.
Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–3.
Samet JH, Phillips SJ, Horton NJ, Traphagen ET, Freedberg KA. Detecting alcohol problems in HIV-infected patients: use of the CAGE questionnaire. AIDS Res Hum Retroviruses. 2004;20:151–5.
Folstein M, Folstein S, McHugh P. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Smith KL, Horton NJ, Saitz R, Samet JH. The use of the mini-mental state examination in recruitment for substance abuse research studies. Drug Alcohol Depend. 2006;82:231–7.
Sobell L, Sobell M. Alcohol Timeline Followback. In: Association AP, ed. Handbook of Psychiatric Measures. Washington, DC; 1996:477–9.
Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med. 2005;352:596–607.
Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Conigliaro J, Madenwald T, Bryant K, et al. The Veterans Aging Cohort Study: observational studies of alcohol use, abuse, and outcomes among human immunodeficiency virus-infected veterans. Alcohol Clin Exp Res. 2004;28:313–21.
Kwiatkowski CF, Fortuin Corsi K, Booth RE. The association between knowledge of hepatitis C virus status and risk behaviors in injection drug users. Addiction. 2002;97:1289–94.
McCusker M.Influence of hepatitis C status on alcohol consumption in opiate users in treatment. Addiction. 2001;96:1007–14.
Ompad DC, Fuller CM, Vlahov D, Thomas D, Strathdee SA. Lack of behavior change after disclosure of hepatitis C virus infection among young injection drug users in Baltimore, Maryland. Clin Infect Dis. 2002;35:783–8.
Nalpas B, Martin S, Fontaine H, Fabbro-Peray P, Brechot C, Pol S. Impact of medical recommendations on alcohol consumption in HCV positive patients. J Hepatol. 2001;35:312–3.
Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705–14.
Seeff LB. Natural history of chronic hepatitis C. Hepatology. 2002;36:S35–46.
Corrao G, Arico S. Independent and combined action of hepatitis C virus infection and alcohol consumption on the risk of symptomatic liver cirrhosis. Hepatology. 1998;27:914–9.
Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol. 2002;155:323–31.
Acknowledgments
The authors appreciate the contribution of Vincent Faber for data management assistance. Support for this study came from the following grants from the National Institute of Alcohol Abuse and Alcoholism (NIAAA) of the NIH: R01-AA13766, R01-AA11785, R01-AA10870, and K24 AA015674. This research was conducted in part in the General Clinical Research Center at Boston University School of Medicine, USPHS Grant M01 RR00533 and the Clinical Research Center at Beth Israel Deaconess Medical Center, USPHS Grant M01 RR01032. Support for Dr. Tsui comes from Grant Number KL2 RR024130 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. This paper was presented at the 29th Society of General Internal Medicine Annual Meeting in April 2006.
Conflict of interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsui, J.I., Saitz, R., Cheng, D.M. et al. Awareness of Hepatitis C Diagnosis is Associated with Less Alcohol Use Among Persons Co-Infected with HIV. J GEN INTERN MED 22, 822–825 (2007). https://doi.org/10.1007/s11606-007-0147-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0147-y