Abstract
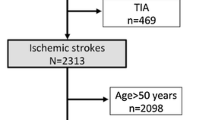
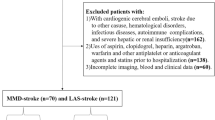
Based on the recently proposed Chinese ischemic stroke subclassification (CISS) system, intracranial branch atheromatous disease (BAD) is divided into large artery atherosclerosis (LAA) and penetrating artery disease (PAD). In the current retrospective analysis, we compared the general characteristics of BAD-LAA with BAD-PAD, BAD-LAA with non-BAD-LAA and BAD-PAD with non-BAD-PAD. The study included a total of 80 cases, including 45 cases of BAD and 35 cases of non-BAD. Subjects were classified using CISS system: BAD-LAA, BAD-PAD, non-BAD-LAA and non-BAD-PAD. In addition to analysis of general characteristics, the correlation between the factors and the two subtypes of BAD was evaluated. The number of cases included in the analysis was: 32 cases of BAD-LAA, 13 cases of BAD-PAD, 21 cases of non-BAD-LAA, and 14 cases of non-BAD-PAD. Diabetes mellitus affected more non-BAD-LAA patients than BAD-LAA patients (P=0.035). In comparison with non-BAD-PAD, patients with BAD-PAD were younger (P=0.040), had higher initial NIHSS score (P<0.001) and morbidity of ischemic heart disease (P=0.033). Within patients with BAD, the PAD subtype was associated with smoking (OR=0.043; P=0.011), higher low-density lipoprotein (OR=5.339; P=0.029), ischemic heart disease (OR=9.383; P=0.047) and diabetes mellitus (OR=12.59; P=0.020). It was concluded that large artery atherosclerosis was the primary mechanism of BAD. The general characteristics showed no significant differences between the CISS subtypes of LAA and PAD within BAD, as well as between the BAD and non-BAD within LAA subtype. Several differences between PAD subtypes of BAD and non-BAD were revealed.
Similar content being viewed by others
References
Yamamoto Y, Ohara T, Hamanaka M, et al. Characteristics of intracranial branch atheromatous disease and its association with progressive motor deficits. J Neurol Sci, 2011,304(1-2):78–82
Kunz S, Griese H, Busse O. Etiology and long-term prognosis of unilateral paramedian pontine infarction with progressive symptoms. Eur Neurol, 2003,50(3): 136–140
Donnan GA, O’ Malley HM, Quang L, et al. The capsular warning syndrome: pathogenesis and clinical features. Neurology, 1993,43(5):957–962
Moon HS, Kim YB, Suh BC, et al. Association of initial infarct extent and progressive motor deficits in striatocapsular infarction. J Clin Neurol, 2008,4(3):111–115
Caplan LR. Intracranial branch atheromatous disease: a neglected, understudied, and underused concept. 1989, 39(9):1246–1250
Klein IF, Lavallee PC, Mazighi M, et al. Basilar artery atherosclerotic plaques in paramedian and lacunar pontine infarctions: a high-resolution MRI study. Stroke, 2010, 41(7):1405–1409
Tatsumi S, Yamamoto T. An autopsied case of an apparent pontine branch atheromatous disease. Eur Neurol, 2010,63(3):184–185
Fisher CM. Capsular infarcts: the underlying vascular lesions. Arch Neurol, 1979,36(2):65–73
Fisher CM, Caplan LR. Basilar artery branch occlusion: a cause of pontine infarction. Neurology, 1971,21(9):900–905
Kwan MW, Mak W, Cheung RT, et al. Ischemic stroke related to intracranial branch atheromatous disease and comparison with large and small artery diseases. J Neurol Sci, 2011,303(1-2):80–84
Adams HJ, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke, 1993,24(1):35–41
Gao S, Wang YJ, Xu AD, et al. Chinese ischemic stroke subclassification. Front Neurol, 2011,2:6
Men X, Wu A, Zhang B, et al. Leukoaraiosis and NIHSS score help to differentiate subtypes of intracranial branch atheromatous disease in Southern Han Chinese patients with stroke. Neurol Sci, 2013,34(10):1727–1733
Nakase T, Yoshioka S, Sasaki M, et al. Clinical evaluation of lacunar infarction and branch atheromatous disease. J Stroke Cerebrovasc Dis, 2013,22(4):406–412
Gallego CJ, Erro AM. Basilar branch occlusion. Curr Treat Options Cardiovasc Med, 2011,13(3):247–260
Ghika JA, Bogousslavsky J, Regli F. Deep perforators from the carotid system. Template of the vascular territories. Arch Neurol, 1990,47(10):1097–1100
Damasio H. A computed tomographic guide to the identification of cerebral vascular territories. Arch Neurol, 1983,40(3):138–142
Miyaji Y, Kawabata Y, Joki H, et al. High-resolution magnetic resonance imaging findings of basilar artery plaque in a patient with branch atheromatous disease: a case report. J Med Case Rep, 2014,8:395
Niizuma K, Shimizu H, Takada S, et al. Middle cerebral artery plaque imaging using 3-Tesla high-resolution MRI. J Clin Neurosci, 2008,15(10):1137–1141
Xu W-H, Li ML, Niu JW, et al. Intracranial artery atherosclerosis and lumen dilation in cerebral small-vessel diseases: a high-resolution MRI study. CNS Neurosci Ther, 2014,20(4):364–367
Chung JW, Kim BJ, Sohn CH, et al. Branch atheromatous plaque: a major cause of lacunar infarction (high-resolution MRI study). Cerebrovasc Dis Extra, 2012,2(1):36–44
Chung JW, Kim BJ, Choi BS, et al. High-resolution magnetic resonance imaging reveals hidden etiologies of symptomatic vertebral arterial lesions. J Stroke Cerebrovasc Dis, 2014,23(2):293–302
Zhao DL, Deng G, Xie B, et al. High-resolution MRI of the vessel wall in patients with symptomatic atherosclerotic stenosis of the middle cerebral artery. J Clin Neurosci, 2015,22(4):700–704
Kim JM, Jung KH, Sohn CH, et al. Middle cerebral artery plaque and prediction of the infarction pattern. Arch Neurol, 2012,69(11):1470–1475
Hoshino H, Takagi M, Yamamoto Y, et al. Neurological progression and clinical outcome of branch atheromatous disease (results from the J-BAD registry. Rinsho Shinkeigaku, 2010,50(11):919–920
Yamamoto Y. Concept, pathophysiology and treatment for branch atheromatous disease. Rinsho Shinkeigaku, 2014,54(4):289–297
Men X, Li J, Zhang B, et al. Homocysteine and C-reactive protein associated with progression and prognosis of intracranial branch atheromatous disease. PLoS One, 2013,8(9):e73030
Yoshida K, Fukumitsu R, Kurosaki Y, et al. The association between expansive arterial remodeling detected by high-resolution MRI in carotid artery stenosis and clinical presentation. J Neurosurg, 2015,123(2):434–440
Wang Q, Zeng Y, Wang Y, et al. Comparison of carotid arterial morphology and plaque composition between patients with acute coronary syndrome and stable coronary artery disease: a high-resolution magnetic resonance imaging study. Int J Cardiovasc Imaging, 2011,27(5):715–726
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Mei, B., Liu, Gz., Yang, Y. et al. Comparative analysis of general characteristics of ischemic stroke of BAD and non-BAD CISS subtypes. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 35, 885–890 (2015). https://doi.org/10.1007/s11596-015-1523-1
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-015-1523-1