Summary
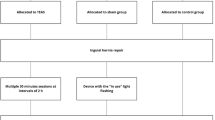
The clinical analgesic effect of electro-acupuncture (EA) stimulation (EAS) on breakthrough pain induced by remifentanil in patients undergoing radical thoracic esophagectomy, and the mechanisms were assessed. Sixty patients (ASAIII) scheduled for elective radical esophagectomy were randomized into three groups: group A (control) receiving a general anesthesia only; group B (sham) given EA needles at PC4 (Ximen) and PC6 (Neiguan) but no stimulation; and group C (EAS) electrically given EAS of the ipsilateral PC4 and PC6 throughout the surgery. The EAS consisting of a disperse-dense wave with a low frequency of 2 Hz and a high frequency of 20 Hz, was performed 30 min prior to induction of general anesthesia and continued through the surgery. At the emergence, sufentanil infusion was given for postoperative analgesia with loading dose of 7.5 μg, followed by a continuous infusion of 2.25 μg/h. The patient self-administration of sufentanil was 0.75 μg with a lockout of 15 min as needed. Additional breakthrough pain was treated with dezocine (5 mg) intravenously at the patient’s request. Blood samples were collected before (T1), 2 h (T2), 24 h (T3), and 48 h (T4) after operation to measure the plasma β-EP, PGE2, and 5-HT. The operative time, the total dose of sufentanil and the dose of self-administration, and the rescue doses of dezocine were recorded. Visual Analogue Scale (VAS) scores at 2, 12, 24 and 48 h postoperatively and the incidence of apnea and severe hypotension were recorded. The results showed that the gender, age, weight, operative time and remifentanil consumption were comparable among 3 groups. Patients in EAS group had the lowest VAS scores postoperatively among the three groups (P<0.05). The total dose of sufentanil was 115±6.0 μg in EAS group, significantly lower than that in control (134.3±5.9 μg) and sham (133.5±7.0 μg) groups. Similarly, the rescue dose of dezocine was the least in EAS group (P<0.05) among the three groups. Plasma β-EP levels in EAS group at T3 (176.90±45.73) and T4 (162.96±35.00 pg/mL) were significantly higher than those in control (132.33±36.75 and 128.79±41.24 pg/mL) and sham (136.56±45.80 and 129.85±36.14 pg/mL) groups, P<0.05 for all. EAS could decrease the release of PGE2. Plasma PGE2 levels in EAS group at T2 and T3 (41±5 and 40±5 pg/mL respectively) were significantly lower than those in control (64±5 and 62±7 pg/mL) and sham (66±6 and 62±6 pg/mL) groups. Plasma 5-HT levels in EAS group at T2 (133.66±40.85) and T3 (154.66±52.49 ng/mL) were significantly lower than those in control (168.33±56.94 and 225.28±82.03) and sham (164.54±47.53 and 217.74±76.45 ng/mL) groups. For intra-group comparison, plasma 5-HT and PGE2 levels in control and sham groups at T2 and T3, and β-EP in EAS group at T3 and T4 were significantly higher than those at T1 (P<0.05); PGE2 and 5-HT levels in EAS group showed no significant difference among the different time points (P>0.05). No apnea or severe hypotension was observed in any group. It was concluded that intraoperative ipsilateral EAS at PC4 and PC6 provides effective postoperative analgesia for patients undergoing radical esophagectomy with remifentanil anesthesia and significantly decrease requirement for parental narcotics. The underlying mechanism may be related to stimulation of the release of endogenous β-EP and inhibition of inflammatory mediators (5-HT and PGE2).
Similar content being viewed by others
References
Kaplan JA, Miller ED, Gallagther EG. Postoperative analgesia for thoracotomy patients. Anesth Analg, 1975,54(6):773–777
Joly V, Richebe P, Guignard B, et al. Remifentanil-induced postoperative hyperalgesia and its prevention with small dose ketamine. Anesthesiology, 2005,103(1):147–155
Sanjay OP, Kadam VR, Menezes J, et al. Thoracic epidural infusions for post thoracotomy pain relief: a clinical study to compare the efficacy of fetanyl-bupivacaine mixtures versus fentanyl alone. Ind J Thorac Cardiovasc Surg, 2003,19:113–118
Komatsu R, Turan AM, Orhan-Sungur M, et al. Remifentanil for general anaesthesia: a systematic review. Anaesthesia, 2007,62(12):1266–1280
Chu LF, Clark DJ, Angst MS. Opioid tolerance and hyperalgesia in chronic pain patients after one month of oral morphine therapy: a preliminary prospective study. J Pain, 2006,7(1):43–48
Angst MS, Clark JD. Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology, 2006,104(3):570–587
Scott NB, Turfrey DJ, Ray DA, et al. A prospective randomized study of the potential benefits of thoracic epidural anesthesia and analgesia in patients undergoing coronary artery bypass grafting. Anesth Analg, 2001,93(3):528–535
Jideus L, Joachimsson PO, Stridsberg M, et al. Thoracic epidural anesthesia does not influence the occurrence of postoperative sustained atrial fibrillation. Am Thorac Surg, 2001,72(1):65–71
Tenling A, Joachimsson PO, Tyden H, et al. Thoracic epidural analgesia as an adjunct to general anaesthesia for cardiac surgery. Acta Anaesthesiol Scand, 2000,44(9):1071–1076
Troster A, Sittl R, Singler B, et al. Modulation of remifentanil-induced analgesia and postinfusion hyperalgesia by parecoxib in humans. Anesthesiology, 2006, 105(5):1016–1023
Lee C, Kim YD, Kim JN. Antihyperalgesic effects of dexmedetomidine on high-dose remifentanil-induced hyperalgesia. Korean J Anesthesiol, 2013,64(4):301–307
Zhang YQ, Ji GC, Wu GC, et al. Excitatory amino acid receptor antagonists and electroacupuncture synergetically inhibit carrageenan-induced behavioral hyperalgesia and spinal for expression in rats. Pain, 2002,99(3):525–535
Zhang Y, Meng XZ, Li AH, et al. Acupuncture alleviates the affective dimension of pain in a rat model of inflammatory hyperalgesia. Neurochem Res, 2011,36(11):2104–2110
Goldman N, Chen M, Fujita T, et al. Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neuroscience, 2010,13(7):883–888
Wang SM, Kain ZN, White P. Acupuncture analgesia:I. The scientific basis. Anesth Analg, 2008,106(2):602–610
Han JS, Chen XH, Sun SL, et al. Effect of different low and high frequency TENS Met-ekephalin-Arg-Phe and dynorphin A immunoreactivity in human lumbar CSF. Pain, 1991,47(3):295–298
Compilation group from Shandong medical school and traditional Chinese medicine school. Altas of Acupuncture Anatomy (Chinese). Jinan: Shandong Science and Technology Press, 1979:29
Vickers AJ, Rusch VW, Malhotra VT, et al. Acupuncture is a feasible treatment for post-thoracotomy pain: results of a prospective pilot trial. BMC Anesthesiol, 2006,6:5
Ma W, Zhu YM, Zhou H, et al. Protecting action of acupuncture-drug compound anesthesia with different frequency electroacupuncture on stress reaction in patients of pneumonectomy. World J Acupuncture Moxibustion (Chinese), 2012,22(3):24–30
Linde K, Vickers A, Hondras M, et al. Systematic reviews of complementary therapies-anannotated bibliography. Part 1: Acupuncture. BMC Complement Altern Med, 2001,1:3
Tenenbein PK, Debrouwere R, Maguire D, et al. Thoracic epidural analgesia improves pulmonary function in patients undergoing cardiac surgery. Can J Anesth, 2008, 55(6):344–350
Hood DD, Curry R, Eisenach JC. Intravenous remifentanil produces withdrawal hyperalgesia in volunteers with capsaicin-induced hyperalgesia. Anesth Analg, 2003, 97(3):810–815
Zhao M, Joo DT. Enhancement of spinal N-methyl-D-aspartate receptor function by remifentanil action at delta-opioid receptors as a mechanism for acute opioid-induced hyperalgesia or tolerance. Anesthesiology, 2008,109(2):308–317
Park JH, Han JB, Kim SK, et al. Spinal GABA receptors mediate the suppressive effect of electroacupuncture on cold allodynia in rats. Brain Res, 2010,1322:24–29
Aloe L, Manni L. Low-frequency electro-acupuncture reduces the nociceptive response and the pain mediator enhancement induced by nerve growth factor. Neurosci Lett, 2009,449(3):73–77
Park JH, Kim SK, Kim HN, et al. Spinal cholinergic mechanism of the relieving effects of electroacupuncture on cold and warm allodynia in a rat model of neuropathic pain. J Physiol Sci, 2009 (59):291–298
Choi BT, Kang J, Jo UB. Effects of electroacupuncture with different frequencies on spinal ionotropic glutamate receptor expression in complete Freund’s adjuvant-injected rat. Acta Histochem, 2005,107(1):67–76
Wang L, Zhang Y, Dai J, et al. Electroacupuncture (EA) modulates the expression of NMDA receptors in primary sensory neurons in relation to hyperalgesia in rats. Brain Res, 2006,1120(1):46–53
Wang ZY, Liang LS, Song WG, et al. Clinical observation of preemptive analgesia effect of HANS and its effect on serum IL-6 level. J Shandong Univ Traditional Chin Med (Chinese), 2000,38(3):300–301
Yang ZJ, Bao GB, Deng HP. Interaction of δ-opioid receptor with membrane transporters: Possible mechanisms in pain suppression by acupuncture. J Acupunct Tuina Sci (Chinese), 2008,6(5):298–300
Redington KI, Disenhouse T, Li J, et al. Electroacupuncture reduces myocardial size and improves post-ischemic recovery by invoking release of humoral, dialyzable, cardioprotective factors. J Physicl Sci, 2013,63(3):219–223
Han JS. Study on the machnisms of acupuncture analgesia. CJIM, 1995,1(1):63–67
Sprouse-Blum AS, Smith G, Suqai D, et al. Unstanding endorphins and their importance in pain management. Hawaii Med J, 2010,69(3):70–71
Max MB. Mechanisms of pain and analgesia. Anesth Prog, 1987,33(4):113
Parikh D, Hamid A, Friedman TC, et al. Stress-induced analgesia and endogenous opioid peptide: the importance of stress duration. Eur J Pharmacol, 2011,650(2–3):563–567
Zhang RX, Lao L, Wang L, et al. Involvement of opioid receptors in electroacupuncture-produced anti-hyperalgesia in rats with peripheral inflammation. Brain Res, 2004,1020(1–2):12–17
Zhang RX, Wang L, Liu B, et al. Mu opioid receptor-containing neurons mediate electroacupuncture-produced anti-hyperalgesia in rats with hind paw inflammation. Brain Res, 2005,1048(1–2):235–240
Lenz H, Raeder J, Draegni T, et al. Effects of COX inhibition on experimental pain and hyperalgesia during and after remifentanil infusion in humans. Pain, 2011,152(6):1289–1297
Marshall TM, Herman DS, Largent-Milnes TM, et al. Activation of descending pain-facilitatory pathways from the rostral ventromedial medulla by cholecystokinin elicits release of prostaglandin-E2 in the spinal cord. Pain, 2012,153(1):86–94
Taiwo YO, Levine JD. Serotonin is a directly-acting hyperalgesic agent in the rat. Neuroscience, 1992,48(2):485–490
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xie, Yh., Chai, Xq., Wang, Yl. et al. Effect of electro-acupuncture stimulation of Ximen (PC4) and Neiguan (PC6) on remifentanil-induced breakthrough pain following thoracal esophagectomy. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 34, 569–574 (2014). https://doi.org/10.1007/s11596-014-1317-x
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-014-1317-x