Abstract
Purpose
Recursive partitioning analysis (RPA) is a prognostic index capable of predicting survival in patients with brain metastases. Histology of the primary tumour has only recently been introduced among the factors that could potentially affect the prognosis of these patients. The main purpose of this study was to analyse the impact of RPA in correlation with histology of the primary tumour in patients with brain metastases treated with hypofractionated radiotherapy.
Materials and methods
A total of 382 patients were treated at the Department of Radiotherapy of Brescia University, and RPA classes were retrospectively assigned to all patients. Univariate and multivariate analyses were then performed to verify the role of the single prognostic variables, for the entire group and for each prognostic class, as well as in correlation with histology of the primary tumour.
Results
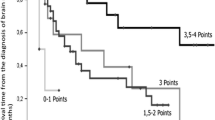
Most patients were classified as RPA prognostic class 2 (48%). The majority of patients was treated with a total dose of 30 Gy delivered in ten fractions, whereas the dose of 20 Gy in four or five fractions was primarily used in patients classified as RPA class 3. At univariate analysis, the main variable correlating with overall survival (OS) was RPA class (p=0.000). Uni- and multivariate analysis performed on RPA class 1 patients only confirmed the role of general performance status, number of metastases and total radiotherapy dose for predicting OS. In the group with the worst prognosis (RPA class 3), none of the variables had a statistically significant role in improving OS. Tumour histology and radiotherapy dose influence OS, even in RPA class 1 and 2 patients.
Conclusions
This analysis confirms that RPA prognostic class is the factor that most predicts survival. Primary tumour histology helps determine prognosis, especially in RPA prognostic classes 1 and 2. As regards RPA class 3, no factor influences survival prognosis.
Riassunto
Obiettivo
La recursive partitioning analysis (RPA) è un indice prognostico capace di predire la sopravvivenza in pazienti affetti da metastasi cerebrali. L’istologia della malattia primitiva è stata solo di recente inserita in maniera organica tra i fattori che potenzialmente potrebbero influenzare la prognosi di questi pazienti. L’obiettivo primario di questo studio è quello di analizzare l’impatto della RPA correlato con l’istologia del tumore primitivo in pazienti con metastasi cerebrali, trattati con radioterapia ipofrazionata.
Materiali e metodi
Trecentoottantadue pazienti sono stati trattati presso la Cattedra di Radioterapia di Brescia. La classe RPA è stata attribuita retrospettivamente a tutti i pazienti. È stata quindi eseguita l’analisi univariata e multivariata per verificare il ruolo delle singole variabili prognostiche, nell’intero gruppo e nelle singole classi prognostiche, anche in correlazione con l’istologia del tumore primitivo.
Risultati
La maggior parte dei pazienti è stata classificata nella classe prognostica RPA 2 (48%). La maggior parte dei pazienti è stata trattata con una dose totale di 30 Gy erogati in 10 frazioni, la dose di 20 Gy in 4 o 5 frazioni è stata utilizzata per lo più in pazienti classificati in classe RPA 3. All’analisi univariata la variabile principale correlata alla sopravvivenza globale (OS) è la classe RPA (p=0,000). L’analisi uni- e multivariata eseguita limitatamente ai pazienti in classe prognostica RPA 1 conferma il ruolo del performance status generale, del numero di metastasi e della dose totale di radioterapia nel predire la OS. Nel gruppo prognosticamente peggiore (RPA 3) nessuna variabile ha un ruolo statisticamente significativo nel migliorare la OS. L’istologia della malattia e la dose di radioterapia influiscono sulla OS, anche in pazienti con classi RPA 1 e 2.
Conclusioni
Questa analisi conferma che le classi prognostiche RPA sono il fattore che principalmente influisce sulla sopravvivenza. L’istologia della neoplasia primitiva influisce sulla prognosi specialmente nelle classi prognostiche RPA 1 e 2. Per la classe prognostica RPA 3 nessun fattore influisce sulla sopravvivenza.
Similar content being viewed by others
References/Bibliografia
Posner JB (1992) Management of brain metastases. Rev Neurol (Paris) 148:477–487
Sawaya R, Bindal RK (1995) Metastatic brain tumors. In: Kaye AH, Laws ER (eds) Brain tumors: an encyclopaedic approach. Churchill Livingstone, Edinburgh, pp 923–946
Zimm S, Wampler GL, Stablein D et al (1981) Intracerebral metastases in solid-tumor patients: natural history and results of treatment. Cancer 48:384–394
Sundstrom JT, Minn H, Lertola KK et al (1998) Prognosis of patients treated for intracranial metastases with wholebrain irradiation. Ann Med 30:296–299
Gaspar L, Scott C, Rotman M et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in the three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiation Oncol 37:745–751
Gaspar L, Scott C, Murray K, Curran W (2000) Validation of the RTOG recursive partitioning analysis (RPA) classification for brain metastases. Int J Radiation Oncol 47:1001–1006
Sperduto PW, Berkey B, Gaspar LE et al (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiation Oncology Biol Phys 70:510–514
Sperduto PW, Chao ST, Sneed PK et al (2010) Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4259 patients. Int J Radiation Oncology Biol Phys 77:655–661
Sperduto PW (2010) What is your patient’s GPA and why does it matter? Managing brain metastases and the cost of hope. Int J Radiation Oncology Biol Phys 77:643–644
Karnofsky DA, Burchenal JH (1949) The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM (ed) Evaluation of chemotherapeutic agents. Columbia University Press, New York, p 196
MRC Brain Tumour Working Party (1990) Prognostic factors for high-grade malignant gliomas: development of a prognostic index. J Neurooncol 9:47–55
Chatani M, Matayoshi Y, Masaki N et al (1994) Radiation therapy for brain metastases from lung carcinoma. Prospective randomized trial according to level of lactate dehydrogenase. Strahlenther Onkol 170:155–161
Harwood AR, Simpson WJ (1977) Radiation therapy of cerebral metastases: a randomized prospective clinical trial. Int J Radiat Oncol Biol Phys 2:1091–1094
Priestman TJ, Dunn J, Brada M et al (1996) Final results of the Royal College of Radiologists trial comparing two different radiotherapy schedules in the treatment of cerebral metastases. J Clin Oncol 8:308–315
Borgelt G, Gelber R, Kramer S et al (1980) The palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 6:1–9
Borgelt B, Gelber R, Larson M et al (1981) Ultra-rapid high dose irradiation schedules for the palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 7:1633–1638
Chatani M, Teshima T, Hata K et al (1985) Whole brain irradiation for metastases from lung carcinoma. A clinical investigation. Acta Radiol Oncol 24:311–314
Kurtz JM, Gelber R, Brady LW et al (1981) The palliation of brain metastases in a favourable patient population: a randomized clinical trial by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 7:891–895
Murray KJ, Scott C, Greenberg H et al (1997) A randomized phase III study of accelerated hyperfractionation versus standard in patients with unresected brain metastases: a report of the Radiation Therapy Oncology Group (RTOG) 9104. Int J Radiat Oncol Biol Phys 39:571–574
Mintz AH, Kestle J, Rathbone MP et al (1996) A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with single brain metastasis. Cancer 78:1470–1476
Noordijk EM, Vecht CJ, Haaxma-Reiche H et al (1994) The choice of treatment of single brain metastasis should be based on extracranial tumour activity and age. Int J Radiat Oncol Biol Phys 29:711–717
Patchell RA, Tibbs PA, Walsh JW et al (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322:494–500
Patchell RA, Tibbs PA, Regine WF et al (1998) Postoperative radiotherapy in the treatment of single metastases to the brain. JAMA 280:1485–1489
Saito EY, Viani GA, Ferrigno R et al (2006) Whole brain radiation therapy in management of brain metastasis: results and prognostic factors. Radiat Oncol 29:20
Videtic GM, Adelstein DJ, Mekhail TM et al (2007) Validation of the RTOG recursive partitioning analysis (RPA) classification for small-cell lung canceronly brain metastases. Int J Radiat Oncol Biol Phys 67:240–243
Cannady SB, Cavanaugh KA, Lee SY et al (2004) Results of whole brain radiotherapy and recursive partitioning analysis in patients with brain metastases from renal cell carcinoma: a retrospective study. Int J Radiat Oncol Biol Phys 58:253–258
Kepka L, Cieslak E, Bujko K et al (2005) Results of the whole-brain radiotherapy for patients with brain metastases from lung cancer: the RTOG RPA intra-classes analysis. Acta Oncol 44:389–398
Agboola O, Benoit B, Cross P et al (1998) Prognostic factors derived from recursive partition analysis (RPA) of Radiation Therapy Oncology Group (RTOG) brain metastases trials applied to surgically resected and irradiated brain metastatic cases. Int J Radiat Oncol Biol Phys 42:155–159
Tendulkar RD, Liu SW, Barnett GH et al (2006) RPA classification has prognostic significance for surgically resected single brain metastasis. Int J Radiat Oncol Biol Phys 66:810–817
Lutterbach J, Bartelt S, Stancu E, Guttenberger R (2002) Patients with brain metastases: hope for recursive partitioning analysis (RPA) class 3. Radiother Oncol 63:339–345
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buglione, M., Bandera, L., Grisanti, S. et al. The impact of tumour histology and recursive partitioning analysis classification on the prognosis of patients treated with whole-brain hypofractionated radiotherapy for brain metastases: analysis of 382 patients. Radiol med 117, 133–147 (2012). https://doi.org/10.1007/s11547-011-0738-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-011-0738-x