Abstract
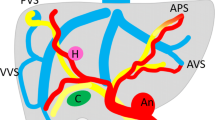
Hereditary haemorrhagic telangiectasia (HHT), also known as Rendu-Osler-Weber disease, is an autosomal-dominant vascular disease characterised by mucocutaneous or visceral angiodysplastic lesions. Its diagnosis is exclusively based on clinical criteria. The brain, lungs and liver, in growing order of prevalence, are the most frequently involved organs. Diagnostic imaging based on ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI) and digital subtraction angiography (DSA) has a fundamental role in detecting visceral involvement in HHT patients and is therefore crucial for the prognostic assessment and therapeutic approach. Arteriovenous shunts are the most common cerebrovascular malformations (CVMs). MRI and CT angiography are the methods of choice for diagnosing cerebral involvement, and it is debated whether MRI could be considered as a screening examination on account of its noninvasiveness. Pulmonary arteriovenous malformations, diffuse telangiectases or high-flow, low-pressure shunts between pulmonary arteries and veins can be studied with contrast-enhanced US, but multidetector CT seems to provide the most comprehensive evaluation of their angioarchitecture, whereas angiography has a predominant role in treatment. Liver involvement is frequent and characterised by the presence of intrahepatic shunts, disseminated intraparenchymal telangiectases and other vascular lesions. US is useful for detecting hepatic lesions but should be completed by more accurate imaging methods such as multidetector CT and MRI.
Riassunto
La telangiectasia emorragica ereditaria (HHT), o malattia di Rendu-Osler-Weber, è un disordine vascolare ereditario, caratterizzato dalla comparsa di lesioni angiodisplasiche mucocutanee e viscerali, la cui diagnosi si basa esclusivamente su criteri clinici. L’encefalo, i polmoni ed il fegato sono, in ordine crescente di prevalenza, le sedi viscerali più frequentemente coinvolte. La diagnostica per immagini, mediante gli ultrasuoni (US), la tomografia computerizzata (TC), la risonanza magnetica (RM) e la angiografia (DSA), ha un ruolo cruciale nella diagnosi del coinvolgimento viscerale nei pazienti affetti da HHT ed è, pertanto, fondamentale nella valutazione prognostica e nella impostazione terapeutica. Tra le malformazioni vascolari cerebrali gli shunt arterovenosi costituiscono l’alterazione più frequente. La RM e la angio-TC sono le metodiche di scelta nella diagnosi dell’interessamento cerebrale, ed è dibattuto se, per la scarsa invasività, la RM sia da proporre come metodica di screening. Le malformazioni arterovenose polmonari, telangiectasie diffuse o fistole tra arterie e vene polmonari, possono essere ricercate con US con MdC, ma la TC multidetettore appare l’indagine più completa per la valutazione della loro angioarchitettura mentre l’angiografia mantiene un ruolo prevalentemente terapeutico. L’interessamento epatico è frequente e caratterizzato dalla comparsa di fistole arterovenose, telangiectasie intraparenchimali ed altre alterazioni vascolari. Gli US sono utili nella ricerca delle lesioni epatiche, ma devono essere integrati da indagini più accurate quali la TC multidetettore e la RM.
Similar content being viewed by others
References/Bibliografia
Dakeishi M, Shioya T, Wada Y et al (2002) Genetic epidemiology of hereditary hemorrhagic telangiectasia in a local community in the northern part of Japan. Hum Mutat 19:140–148
Kjeldsen AD, Vase P, Green A (2000) Hereditary hemorrhagic telangiectasia. A population-based study on prevalence and mortality among Danish HHT patients. Ugeskr Laeger 162:3597–3601
Guttmacher AE, Marchuk DA, White RI Jr (1995) Hereditary hemorrhagic telangiectasia. N Engl J Med 333:918–924
Ianora AA, Memeo M, Sabba C et al (2004) Hereditary hemorrhagic telangiectasia: multi-detector row helical CT assessment of hepatic involvement. Radiology 230:250–259
Plauchu H, de Chadarevian JP, Bideau A, Robert JM (1989) Age-related clinical profile of hereditary hemorrhagic telangiectasia in an epidemiologically recruited population. Am J Med Genet 32:291–297
Shovlin CL, Guttmacher AE, Buscarini E et al (2000) Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet 91:66–67
Marchuk DA, Guttmacher AE, Penner JA, Ganguly P (1998) Report on the workshop on Hereditary Hemorrhagic Telangiectasia, July 10–11, 1997. Am J Med Genet 76:269–273
Ference BA, Shannon TM, White RI Jr et al (1994) Life-threatening pulmonary hemorrhage with pulmonary arteriovenous malformations and hereditary hemorrhagic telangiectasia. Chest 106:1387–1390
Matsubara S, Mandzia JL, ter Brugge K et al (2000) Angiographic and clinical characteristics of patients with cerebral arteriovenous malformations associated with hereditary hemorrhagic telangiectasia. AJNR Am J Neuroradiol 21:1016–1020
Fulbright RK, Chaloupka JC, Putman CM et al (1998) MR of hereditary hemorrhagic telangiectasia: prevalence and spectrum of cerebrovascular malformations. AJNR Am J Neuroradiol 19:477–484
Putman CM, Chaloupka JC, Fulbright RK et al (1996) Exceptional multiplicity of cerebral arteriovenous malformations associated with hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome). AJNR Am J Neuroradiol 17:1733–1742
Kawaguchi T, Fujita S, Yamada H et al (1990) Multiple cerebral and pulmonary arteriovenous malformations in association with brain and subcutaneous abscesses: a possible variant of hereditary hemorrhagic telangiectasia-case report. Neurol Med Chir (Tokyo) 30:272–276
Berenstein A, Lasjaunias P, ter Brugge KG (2004) Cerebral vascular malformations: incidence, classification, angioarchitecture, and symptomatology of brain arteriovenous and venous malformations. In: Surgical Neuroangiography, Vol.2: Clinical and Endovascular Treatment Aspects in Adults. 2nd edn. Springer, Berlin, pp 609–694
Maher CO, Piepgras DG, Brown RD Jr et al (2001) Cerebrovascular manifestations in 321 cases of hereditary hemorrhagic telangiectasia. Stroke 32:877–882
Yasargil M (1997) Microneurosurgery. Thieme Publishers, Stuttgart
Willinsky R, Lasjaunias P, Comoy J, Pruvost P (1988) Cerebral micro arteriovenous malformations (mAVM): review of 13 cases. Acta Neurochir (Wien) 91:29–36
Al-Shahi R, Warlow C (2001). A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain 124:1900–1926
Lasjaunias, P Burrows, C Placet (1986) Developmental venous anomalies (DVA): the so-called venous angioma. Neurosurg Rev 9:233–242
Cirillo S, Simonetti L, Sirabella G et al (1999) Cranio-encefalo: patologia vascolare. In: Dal Pozzo G (ed) Compendio di tomografia computerizzata e TC spirale. UTET, Torino, pp 159–183
Willemse RB, Mager JJ, Westermann CJ et al (2000) Bleeding risk of cerebrovascular malformations in hereditary hemorrhagic telangiectasia. J Neurosurg 92:779–784
Brown R, Weibers D, Forbes G et al (1988) The natural history of unruptured intracranical arteriovenous malformations. J Neurosurg 68:353–357
Teragaki M, Akioka K, Yasuda M et al (1988) Hereditary hemorrhagic telangiectasia with growing pulmonary arteriovenous fistulas followed for 24 years. Am J Med Sci 295:545–547
Shovlin CL, Letarte M (1999) Hereditary haemorrhagic telangiectasia and pulmonary arteriovenous malformations: issues in clinical management and review of pathogenic mechanisms. Thorax 54:714–729
Bosher L, Blake A, Byrd B (1959) An analysis of pathologic anatomy of pulmonary arteriovenous aneurysms with particular reference to the applicability of local excision. Surgery 45:91–104
Saluja S, Henderson K, White RI Jr (2000) Embolotherapy in the bronchial and pulmonary circulations. Radiol Clin North Am 38:425–448
White RI Jr, Lynch-Nyhan A, Terry P et al (1988) Pulmonary arteriovenous malformations: techniques and longterm outcome of embolotherapy. Radiology 169:663–669
Faughnan ME, Lui Y, Wirth JA et al (2000) Diffuse pulmonary arteriovenous malformations. Characteristics and prognosis. Chest 117:31–38
White RI Jr, Mitchell S, Barth KH et al (1983) Angioarchitecture of pulmonary arteriovenous malformations: an important consideration before embolotherapy. AJR Am J Roentgenol 140:681–686
White RI Jr, Pollak JS, Wirth JA (1996) Pulmonary arteriovenous malformations: diagnosis and transcatheter embolotherapy. J Vasc Interv Radiol 7:787–804
Remy J, Remy-Jardin M, Wattinne L, Deffontaines C (1992) Pulmonary arteriovenous malformations: evaluation with CT of the chest before and after treatment. Radiology 182:809–816
Kjeldsen AD, Oxhoj H, Andersen PE et al (1999) Pulmonary arteriovenous malformations: screening procedures and pulmonary angiography in patients with hereditary hemorrhagic telangiectasia. Chest 116:432–439
Haitjema T, Disch F, Overtoom TT et al (1995) Screening family members of patients with hereditary hemorrhagic telangiectasia. Am J Med 99:519–524
Nanthakumar K, Graham AT, Robinson TI et al (2001) Contrast echocardiography for detection of pulmonary arteriovenous malformations. Am Heart J 141:243–246
Lee WL, Graham AF, Pugash RA et al (2003) Contrast echocardiography remains positive after treatment of pulmonary arteriovenous malformations. Chest 123:351–358
Gramiak R, Shah P (1968) Echocardography of the aortic root. Invest Radiol 3:356–366
Ernst A, Cikes I, Custovic F (1984) Polygenin colloid solution as an echocardiographic contrast agent. J Cardiovasc Ultrasonography 3:143–145
Berwing K, Schlepper M (1988) Echocardiographic imaging of the left ventricle by peripheral intravenous injection of echo contrast agent. Am Heart J 115:399–408
Gossage J, Kanj G (1988) Pulmonary arteriovenous malformations. A state of the art review. Am J Respir Crit Care Med 158:643–661
Rydberg G, Buckwalter K, Caldemeyer K (2000) Multisection CT: scanning techniques and clinical application. Radiographics 20:1787–1806
Remy J, Remy-Jardin M, Giraud F, Wattinne L (1994) Angioarchitecture of pulmonary arteriovenous malformations: clinical utility of three-dimensional helical CT. Radiology 191:657–664
Rankin S, Faling LJ, Pugatch RD (1992) CT diagnosis of pulmonary arteriovenous malformations. J Comput Assist Tomogr 6:746–749
Webb W, Gamsu G, Golden J, Crooks L (1984) Nuclear magnetic resonance of pulmonary arteriovenous fistula: effects of flow. J Comput Assist Tomogr 8:155–157
Khalil A, Farres M, Mangiapan G et al (2000) Pulmonary arteriovenous malformations. Diagnosis by contrast-enhanced Magnetic Resonance Angiography. Chest 117:1399–1403
Feinstein JA, Moore P, Rosenthal DN et al (2002) Comparison of contrast echocardiography versus cardiac catheterization for detection of pulmonary arteriovenous malformations. Am J Cardiol 89:281–285
Oxhoj H, Kjeldsen AD, Nielsen G (2000) Screening for pulmonary arteriovenous malformations: contrast echocardiography versus pulse oximetry. Scand Cardiovasc J 34:281–285
Gossage J (2003) The role of echocardiography in screening for pulmonary arteriovenous malformations. Chest 123:320–322
Reilly PJ, Nostrant TT (1984) Clinical manifestations of hereditary hemorrhagic telangiectasia. Am J Gastroenterol 79:363–367
Bernard G, Mion F, Henry L et al (1993) Hepatic involvement in hereditary hemorrhagic telangiectasia: clinical, radiological, and hemodynamic studies of 11 cases. Gastroenterology 105:482–487
Cloogman HM, Di Capo RD (1984) Hereditary hemorrhagic telangiectasia: sonographic findings in the liver. Radiology 150:521–522
Naganuma H, Ishida H, Niizawa M et al (1995) Hepatic involvement in Osler-Weber-Rendu disease: findings on pulsed and color Doppler sonography. AJR Am J Roentgenol 165:1421–1425
Lane MJ, Jeffrey RB Jr, Katz DS (2000) Spontaneous intrahepatic vascular shunts. AJR Am J Roentgenol 174:125–131
Memeo M, Stabile Ianora AA, Scardapane A et al (2004) Hepatic involvement in hereditary hemorrhagic telangiectasia. Abdom Imaging 29:211–220
Buscarini E, Buscarini L, Danesino C et al (1997) Hepatic vascular malformations in hereditary hemorrhagic telangiectasia: Doppler sonographic screening in a large family. J Hepatol 26:111–118
Caselitz M, Bahr MJ, Bleck JS et al (2003) Sonographic criteria for the diagnosis of hepatic involvement in hereditary hemorrhagic telangiectasia (HHT). Hepatology 37:1139–1146
Hashimoto M, Tate E, Nishii T et al (2003) Angiography of hepatic vascular malformations associated with hereditary hemorrhagic telangiectasia. Cardiovasc Intervent Radiol 26:177–180
Ralls PW, Johnson MB, Radin DR et al (1992) Hereditary hemorrhagic telangiectasia: findings in the liver with color Doppler sonography. AJR Am J Roentgenol 159:59–61
Buscarini E, Buscarini L, Civardi G et al (1994) Hepatic vascular malformations in hereditary hemorrhagic telangiectasia: imaging findings. AJR Am J Roentgenol 163:1105–1110
Bodner G, Peer S, Karner M et al (2002) Nontumorous vascular malformations in the liver: color Doppler ultrasonographic findings. J Ultrasound Med 21:187–197
Chou YH, Tiu CM, Hsu CC et al (2000) Hereditary haemorrhagic telangiectasia: hepatic lesions demonstrated with colour Doppler and power Doppler sonography. Eur J Radiol 34:52–56
Goes E, Van Tussenbroeck F, Cottenie F et al (1987) Osler’s disease diagnosed by ultrasound. J Clin Ultrasound 15:129–131
Lin JH, Yang PM, Tsang YM, Hsieh FJ (1999) Sequential Doppler sonographic studies of embolization in a patient with hepatic involvement in hereditary hemorrhagic telangiectasia: correlation with angiographic findings. J Formos Med Assoc 98:633–638
Matsuo M, Kanematsu M, Kato H et al (2001) Osler-Weber-Rendu disease: visualizing portovenous shunting with three-dimensional sonography. AJR Am J Roentgenol 176:919–920
Vilgrain V, Menu Y, Nahum H (1991) Doppler sonography in Osler-Weber-Rendu disease. AJR Am J Roentgenol 157:413–414
Pompili M, Rapaccini GL, Marzano MA et al (1994) Doppler ultrasound findings in Osler-Weber-Rendu disease with hepatic involvement: a case report. Ital J Gastroenterol 26:83–85
Milot L; Gautier G; Beuf O; Pilleul F (2006) Hereditary hemorrhagic telangiectases: magnetic resonance imaging features in liver involvement. J Comput Assist Tomogr 30:405–411
Itai Y, Kurosaki Y, Saida Y et al (1994) CT and MRI in detection of intrahepatic portosystemic shunts in patients with liver cirrhosis. J Comput Assist Tomogr 18:768–773
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Memeo, M., Scardapane, A., De Blasi, R. et al. Diagnostic imaging in the study of visceral involvement of hereditary haemorrhagic telangiectasia. radiol med 113, 547–566 (2008). https://doi.org/10.1007/s11547-008-0276-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-008-0276-3
Keywords
- Hereditary hemorrhagic telangiectasia
- Rendu-Osler-Weber disease
- Cerebral arteriovenous malformations
- Pulmonary arteriovenous malformations
- Intrahepatic shunts