Abstract
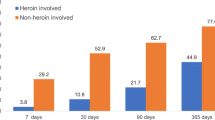
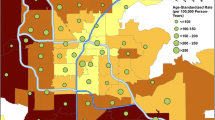
Opioid overprescribing is a major driver of the current opioid overdose epidemic. However, annual opioid prescribing in the USA dropped from 782 to 640 morphine milligram equivalents per capita between 2010 and 2015, while opioid overdose deaths increased by 63%. To better understand the role of prescription opioids and health care utilization prior to opioid-related overdose, we analyzed the death records of decedents who died of an opioid overdose in Illinois in 2016 and linked to any existing controlled substance monitoring program (CSMP) and emergency department (ED) or hospital discharge records. We found that of the 1893 opioid-related overdoses, 573 (30.2%) decedents had not filled an opioid analgesic prescription within the 6 years prior to death. Decedents without an opioid prescription were more likely to be black (33.3% vs 20.2%, p < .001), Hispanic (16.3% vs 8.8%, p < .001), and Chicago residents (46.8% vs 25.6%, p < .001) than decedents with at least one filled opioid prescription. Decedents who did not fill an opioid prescription were less likely to die of an overdose involving prescribed opioids (7.3% vs 19.5%, p < .001) and more likely to fatally overdose on heroin (63% vs 50.4%, p < .001) or fentanyl/fentanyl analogues (50.3% vs 41.8%, p = .001). Between 2012 and the time of death, decedents without an opioid prescription had fewer emergency department admissions (2.5 ± 4.2 vs 10.6 ± 15.8, p < .001), were less likely to receive an opioid use disorder diagnosis (41.3% vs 47.5%, p = .052), and were less likely to be prescribed buprenorphine for opioid use disorder treatment (3.3% vs 8.6%, p < .001). Public health interventions have often focused on opioid prescribing and the use of CSMPs as the core preventive measures to address the opioid crisis. We identified a subset of individuals in Illinois who may not be impacted by such interventions. Additional research is needed to understand what strategies may be successful among high-risk populations that have limited opioid analgesic prescription history and low health care utilization.
Similar content being viewed by others
Notes
We are using the terminology CSMP to more accurately describe these databases, which house information about receipt of controlled substance prescriptions (as opposed to all prescriptions) that are obtained in retail pharmacies.
AL, AR, AZ, CA, CO, FL, GA, IA, ID, IL, IN, KS, KY, LA, MA, MD, MI, MN, MO, MS, NC, ND, NE, NH, NV, NY, OH, OK, OR, PA, TN, TX, UT, VA, WI.
References
Kochanek KD, Murphy S, Xu J, Arias E. Mortality in the United States, 2016. NCHS Data Brief. 2017;293:1–8.
Morone NE, Weiner DK. Pain as the fifth vital sign: exposing the vital need for pain education. Clin Ther. 2013;35(11):1728–32.
Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiat. 2014;71(7):821–6.
Muhuri P, Gfroerer J, Davies M. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Review. 2013. Available at https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm. Accessed 1 March 2018.
Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154–63.
Morgan L, Weaver M, Sayeed Z, Orr R. The use of prescription monitoring programs to reduce opioid diversion and improve patient safety. J Pain Palliat Care Pharmacother. 2013;27:4–9.
Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff (Millwood). 2016;35(10):1876–83.
Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation of prescription drug monitoring programs associated with reductions in opioid-related death. Health Aff (Millwood). 2016;35(7):1324–32.
Reifler LM, Droz D, Bailey JE, Schnoll SH, Fant R, Dart RC, et al. Do prescription monitoring programs impact state trends in opioid abuse/misuse? Pain Med. 2012;13:434–42.
Patrick SW, Carrie EF, Jones TF, Buntin MB. Implementation of prescription drug monitoring programs associated with reductions in opioid-related death rates. Health Aff. 2016;35(7):1324–32.
Bryce P. Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction. 2017;112(10):1773–83.
Paulozzi LJ, Kilbourne EM, Desai HM. Prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011;12:747–54.
Li G, Brady JE, Lang BH, Giglio J, Wunsch H, DiMaggio C. Prescription drug monitoring and drug overdose mortality. Injury Epidemiol. 2014;1(9):9.
Brady JE, Wunsch H, Dimaggio C, Lang BH, Giglio J, Li G. Prescription drug monitoring and dispensing of prescription opioids. Public Health Rep. 2014;129(2):139–47.
Green TC, Bowman S, Davis C, Los C, McHugh K, Friedmann PD. Discrepancies in addressing overdose prevention through prescription monitoring programs. Drug Alcohol Depend. 2015;153:355–8.
Guy GP Jr, Zhang K, Bohm MK, et al. vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66:697–704. https://doi.org/10.15585/mmwr.mm6626a4.
Overdose Death Rates. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed 4/1/2018; 2018.
2017 State of Illinois Comprehensive Opioid Data Report. Springfield, IL: Illinois Department of Public Health; 2017. Available at http://www.dph.illinois.gov/sites/default/files/publications/publicationsdoil-opioid-data-report.pdf. Accessed 13 Feb 2018.
Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182–6.
Pain management and the opioid epidemic: balancing societal and individual benefits and risks of prescription opioid use. In: Phillips JK, Ford MA, Bonnie RJ, editors. Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse. Washington, DC: National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; 2017. Available at https://www.ncbi.nlm.nih.gov/pubmed/29023083. Accessed 23 Feb 2018.
Davoli M, Bargagli AM, Perucci CA, Schifano P, Belleudi V, Hickman M, et al. Risk of fatal overdose during and after specialist drug treatment: the VEdeTTE study, a national multi-site prospective cohort study. Addiction. 2007;102(12):1954–9.
Caudarella A, Dong H, Milloy MJ, Kerr T, Wood E, Hayashi K. Non-fatal overdose as a risk factor for subsequent fatal overdose among people who inject drugs. Drug Alcohol Depend. 2016;162:51–5.
Winkler WE. String comparator metrics and enhanced decision rules in the Fellegi Sunter model of record linkage. In: Proceedings of the Section on Survey Research Methods. Alexandria, VA: American Statistical Association; 1990.
Abbasi AB, Clark H, Agbodo N. Learning algorithm to identify drugs involved in drug overdose deaths from literal text on death certificates. West Palm Beach, FL: Council of State and Territorial Epidemiologists; 2018.
Fentanyl: a briefing guide for first responders. Washington, DC: U.S. Department of Justice, Drug enforcement administration; 2017. Archived at: https://www.nvfc.org/wp-content/uploads/2018/03/Fentanyl-Briefing-Guide-for-First-Responders.pdf. Accessed 25 Dec 2017.
Epidemiology report: increase in overdose deaths involving opioids – Chicago 2015–2016. Chicago, IL: Chicago Department of Public Health; 2017. Available athttps://www.cityofchicago.org/content/dam/city/depts/cdph/tobacco_alchohol_and_drug_abuse/2016ChicagoOpioidReport.pdf. Accessed Accessed 14 March 2018.
Health Resources & Services Administration. Defining rural population. https://www.hrsa.gov/ruralhealth/about-us/definition/index.html. Accessed 1 April 2018.
Cicero TJ, Kasper ZA, Ellis MS. Increased use of heroin as an initiating opioid of abuse: further considerations and policy implications. Addict Behav. 2018;87:267–71.
CDC. Data resources: analyzing prescription data and morphine milligram equivalents (MME). https://www.cdc.gov/drugoverdose/resources/data.html. Accessed 8/22/2017; 2017.
Surratt HL, Kurtz SP, Buttram M, Levi-Minzi MA, Pagano ME, Cicero TJ. Heroin use onset among nonmedical prescription opioid users in the club scene. Drug Alcohol Depend. 2017;179:131–8.
Quinones S. Dreamland: the true tale of America’s opiate epidemic. New York, NY: Bloomsbury Press; 2015.
Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–74.
Park TW, Saitz R, Ganoczy D, Ilgen MA, Bohnert AS. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ. 2015;350:h2698.
Jones JD, Mogali S, Comer SD. Polydrug abuse: a review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012;125(1–2):8–18.
Calcaterra SL, Yamashita TE, Min SJ, Keniston A, Frank JW, Binswanger IA. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478–85.
Hill MV, Stucke RS, Billmeier SE, Kelly JL, Barth RJ Jr. Guideline for discharge opioid prescriptions after inpatient general surgical procedures. J Am Coll Surg. 2018;226(6):996–1003.
Chen J, Vargas-Bustamante A, Mortensen K, Ortega AN. Racial and ethnic disparities in health care access and utilization under the affordable care act. Med Care. 2016;54(2):140–6.
Singhal A, Tien YY, Hsia RY. Racial-ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PLoS One. 2016;11(8):e0159224.
Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–8.
Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am J Psychiatr. 2001;158(12):2027–32.
Stein BD, Gordon AJ, Sorbero M, Dick AW, Schuster J, Farmer C. The impact of buprenorphine on treatment of opioid dependence in a Medicaid population: recent service utilization trends in the use of buprenorphine and methadone. Drug Alcohol Depend. 2012;123(1–3):72–8.
Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief. 2017;(289):1–8.
Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2017. Available at https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed 12 Feb 2018.
Cicero TJ, Ellis MS, Kasper ZA. Increases in self-reported fentanyl use among a population entering drug treatment: the need for systematic surveillance of illicitly manufactured opioids. Drug Alcohol Depend. 2017;177:101–3.
Acknowledgments
The authors were funded by the University of Chicago Institute of Politics (ABA), NIDA UG3DA044829 (MTP), and AHRQ R00HS022433 (MTP). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abbasi, A.B., Salisbury-Afshar, E., Jovanov, D. et al. Health Care Utilization of Opioid Overdose Decedents with No Opioid Analgesic Prescription History. J Urban Health 96, 38–48 (2019). https://doi.org/10.1007/s11524-018-00329-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-018-00329-x