Abstract
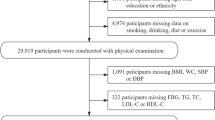
PM2.5-hypertension association were well documented in adults, while the effects of life-course exposure to PM2.5 on adulthood hypertension remained unclear. This study aimed to investigate the associations between life-course exposure to ambient PM2.5 and incident hypertension in adulthood in Asia. We included 4272 participants with 17,814 medical visits from two open cohorts in Taiwan and Hong Kong between 2000 and 2018. We used a satellite-based model to assess 2-year average PM2.5 exposure at a resolution of 1 km2. A linear mixed model was used to examine the association with blood pressure. A Cox regression model with time-dependent covariates was used to examine the overall association with the development of hypertension in adulthood. Life-course mixed models were used to examine the effects of PM2.5 exposure at different life stages on blood pressure and hypertension. For every 10 μg/m3 increase in PM2.5, the overall risk of adulthood hypertension increased by 40% (95% confidence interval [CI] 8–80%). The health effects of PM2.5 exposure at different life-stages on incident hypertension were generally independent of each other. In critical model, the risk of developing hypertension increased 23%, 27%, and 55% for each 10 μg/m3 increase in PM2.5 exposure during school age, adolescence, and adulthood, respectively. Similar associations were found between life-course PM2.5 exposure and blood pressure. Association between PM2.5 and adulthood hypertension can be traced back to childhood. Our study suggests that life-course control of air pollution exposure should be implemented to alleviate the huge burden of adulthood hypertension.


Similar content being viewed by others
Data availability
All data generated or analyzed during this study can be requested appropriately from the corresponding author.
References
Bilenko N, Brunekreef B, Beelen R, Eeftens M, de Hoogh K, Hoek G et al (2015) Associations between particulate matter composition and childhood blood pressure—the piama study. Environ Int 84:1–6
Bo Y, Guo C, Lin C, Chang L-y, Chan T-C, Huang B et al (2019) Dynamic changes in long-term exposure to ambient particulate matter and incidence of hypertension in adults: a natural experiment. Hypertension 74:669–677
Chang LY, Tsai SP, Wang ML, et al (2016) MJ Health Database (MJHD), a large health database in Taiwan, MJ Health Research Foundation Technical Report, MJHRF-TR-01, August, 2016. Available from http://www.mjhrf.org/file/en/report/MJHRF-TR01MJ%20Health%20Database.pdf. Accessed 28 July 2022
Chen X, Wang Y (2008) Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117:3171
Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV et al (2015) Ambient pm2. 5, o3, and no2 exposures and associations with mortality over 16 years of follow-up in the canadian census health and environment cohort (canchec). Environ Health Persp 123:1180–1186
Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C et al (2017) Air pollution and mortality in the medicare population. N Engl J Med 376:2513–2522
Dong GH, Wang J, Zeng XW, Chen L, Qin XD, Zhou Y et al (2015) Interactions between air pollution and obesity on blood pressure and hypertension in Chinese children. Epidemiol 26:740–747
Gehring U, Wijga AH, Koppelman GH, Vonk JM, Smit HA, Brunekreef B (2020) Air pollution and the development of asthma from birth until young adulthood. Eur Respir J 56:2000147. https://doi.org/10.1183/13993003.00147-2020
Guo C, Hoek G, Chang L-y, Bo Y, Lin C, Huang B et al (2019) Long-term exposure to ambient fine particulate matter (pm 2.5) and lung function in children, adolescents, and young adults: a longitudinal cohort study. Environ Health Perspect 127:127008
Guo C, Zeng Y, Chang L-y, Yu Z, Bo Y, Lin C et al (2020) Independent and opposing associations of habitual exercise and chronic pm2. 5 exposures on hypertension incidence. Circulation 142:645–656
Kioumourtzoglou M-A, Schwartz J, James P, Dominici F, Zanobetti A (2016) Pm2. 5 and mortality in 207 US cities: modification by temperature and city characteristics. Epidemiol 27:221
Kmietowicz Z (2018) Health of 1.8 billion children is at serious risk from air pollution, says WHO. BMJ 363:k4580
Lin C, Li Y, Yuan Z, Lau AK, Li C, Fung JC (2015) Using satellite remote sensing data to estimate the high-resolution distribution of ground-level PM2.5. Remote Sens Environ 156:117–28
Lin C, Li Y, Lau AK, Li C, Fung JC (2018) 15-year PM2.5 trends in the Pearl River Delta region and Hong Kong from satellite observation. Aerosol Air Qual Res 18(9):2355–62
Liu C, Fuertes E, Tiesler CM, Birk M, Babisch W, Bauer C-P et al (2014) The associations between traffic-related air pollution and noise with blood pressure in children: results from the giniplus and lisaplus studies. Int J Hyg Environ Health 217:499–505
Meng X, Zhang Y, Yang KQ, Yang YK, Zhou XL (2016) Potential harmful effects of pm2.5 on occurrence and progression of acute coronary syndrome: epidemiology, mechanisms, and prevention measures. Int J Environ Res Public Health 13:748
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K et al (2016) Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 134:441–450
Mishra G, Nitsch D, Black S, De Stavola B, Kuh D, Hardy R (2009) A structured approach to modelling the effects of binary exposure variables over the life course. Int J Epidemiol 38:528–537
Mitchell GF, Moyé LA, Braunwald E, Rouleau JL, Bernstein V, Geltman EM, et al (1997) Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. Circulation 96:4254–4260
Muntner P, He J, Cutler JA, Wildman RP, Whelton PK (2004) Trends in blood pressure among children and adolescents. JAMA 291:2107–2113
Nanchahal K, Ashton WD, Wood DA (2000) Alcohol consumption, metabolic cardiovascular risk factors and hypertension in women. Int J Epidemiol 29:57–64
Ntarladima AM, Vaartjes I, Grobbee DE, Dijst M, Schmitz O, Uiterwaal C et al (2019) Relations between air pollution and vascular development in 5-year old children: a cross-sectional study in the netherlands. Environ Health 18:50
World Health Organization (2013) Draft comprehensive global monitoring framework and targets for the prevention and control of noncommunicable diseases: formal meeting of the Member States to conclude the work on the comprehensive global monitoring framework, including indicators, and a set of voluntary global targets for the prevention and control of noncommunicable diseases: report by the Director-General. 2013. Available from https://apps.who.int/iris/handle/10665/105633. Accessed 28 July 2022
Pieters N, Koppen G, Van Poppel M, De Prins S, Cox B, Dons E et al (2015) Blood pressure and same-day exposure to air pollution at school: associations with nano-sized to coarse pm in children. Environ Health Perspect 123:737–742
Qin P, Luo X, Zeng Y, Zhang Y, Li Y, Wu Y et al (2021) Long-term association of ambient air pollution and hypertension in adults and in children: a systematic review and meta-analysis. Sci Total Environ 796:148620
Rajagopalan S, Al-Kindi SG, Brook RD (2018) Air pollution and cardiovascular disease: Jacc state-of-the-art review. J Am Coll Cardiol 72:2054–2070
Sanders AP, Saland JM, Wright RO, Satlin L (2018) Perinatal and childhood exposure to environmental chemicals and blood pressure in children: a review of literature 2007–2017. Pediatr Res 84:165–180
Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC (2018) The age of adolescence. Lancet Child Adolesc 2:223–228
Schultz ES, Hallberg J, Bellander T, Bergstrom A, Bottai M, Chiesa F et al (2016) Early-life exposure to traffic-related air pollution and lung function in adolescence. Am J Respir Crit Care Med 193:171–177
Sharma AK, Metzger DL, Rodd CJ (2018) Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr 172:557–565
Sly PD, Flack F (2008) Susceptibility of children to environmental pollutants. Ann NY Acad Sci 1140(1):163–183
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D et al (2020) 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypert 75:1334–1357
van Rossem L, Rifas-Shiman SL, Melly SJ, Kloog I, Luttmann-Gibson H, Zanobetti A et al (2015) Prenatal air pollution exposure and newborn blood pressure. Environ Health Perspect 123:353–359
Warembourg C, Maitre L, Tamayo-Uria I, Fossati S, Roumeliotaki T, Aasvang GM et al (2019) Early-life environmental exposures and blood pressure in children. J Am Coll Cardiol 74:1317–1328
Whelton PK, Carey RM, Aronow WS et al (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 71(19):e127–e248
Xiao X, Yang BY, Hu LW, Markevych I, Bloom MS, Dharmage SC et al (2020) Greenness around schools associated with lower risk of hypertension among children: findings from the seven northeastern cities study in china. Environ Pollut 256:113422
Yu P, Xu R, Coelho MS, Saldiva PH, Li S, Zhao Q et al (2021) The impacts of long-term exposure to pm2.5 on cancer hospitalizations in Brazil. Environ Int 154:106671
Zhang Z, Ly C, Lau AK, Chan TC, Chieh Chuang Y, Chan J et al (2017) Satellite-based estimates of long-term exposure to fine particulate matter are associated with c-reactive protein in 30 034 taiwanese adults. Int J Epidemiol 46:1126–1136
Zhang Z, Guo C, Lau AK, Chan TC, Chuang YC, Lin C et al (2018) Long-term exposure to fine particulate matter, blood pressure, and incident hypertension in taiwanese adults. Environ Health Perspect 126:017008
Zhang Z, Dong B, Li S, Chen G, Yang Z, Dong Y et al (2019) Exposure to ambient particulate matter air pollution, blood pressure and hypertension in children and adolescents: a national cross-sectional study in China. Environ Int 128:103–108
Zhou B, Bentham J, Di Cesare M, Bixby H, Danaei G, Cowan MJ et al (2017) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet 389:37–55
Funding
This work was in part supported by Direct Grant for Research of the Chinese University of Hong Kong (2020.023), Guangdong Basic and Applied Basic Research Foundation (2019A1515011697), and Health and Medical Research Fund (19202201). Cui Guo is in part supported by the RGC Postdoctoral Fellowship Scheme of Hong Kong.
Author information
Authors and Affiliations
Contributions
CG and XQL conceived of and designed the study. LC, AKHL, TT, and XQL acquired the data. CG analyzed data and drafted the manuscript. CG and XQL interpreted the results. All authors critically revised the manuscript. CG and XQL acquired the funding. LC, AKHL, TT, and XQL supervised this study.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee (2018.388 and 2021.233).
Consent to participate
Each participant signed written informed consent prior to each medical examination.
Consent for publication
All the authors agreed with the content and agreed to submit.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, C., Chang, Ly., Bo, Y. et al. Life-course exposure to ambient fine particulate matter and hypertension in adulthood: a longitudinal cohort study. Environ Sci Pollut Res 30, 788–797 (2023). https://doi.org/10.1007/s11356-022-22272-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-022-22272-w