Abstract
Purpose
The presence of periodic limb movements during sleep (PLMS) varies among patients with obstructive sleep apnea (OSA) undergoing treatment with continuous positive airway pressure (CPAP). The factors associated with this variation are unknown.
Methods
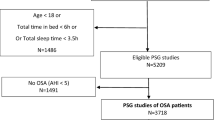
PLMS were defined as a periodic leg movements index of > 15/h. Patients with OSA and PLMS were categorized into four groups depending on diagnostic and CPAP titration polysomnography (PSG). A multinomial logistic regression analysis was performed using a non-PLMS group as the reference category.
Results
This study included 861 patients with OSA who underwent a full-night CPAP titration PSG. The proportions of the subjects with PLMS on both PSGs (persistent PLMS), those with CPAP-emergent PLMS, and those with CPAP-resolved PLMS were 12.9%, 9.2%, and 3.9%, respectively. Compared with the non-PLMS group, the persistent group was more likely to be of older age and male sex and has a higher body mass index and restless legs syndrome (RLS). Patients in the CPAP-emergent group were also older and more likely to have RLS as well as more severe apnea. Patients in the CPAP-resolved group were more likely to be women, of older age, have a higher body mass index, but less severe apnea.
Conclusions
PLMS elicited by CPAP are more likely to occur in older patients with more severe sleep apnea and comorbid RLS, whereas OSA patients in which PLMS resolve after CPAP are more likely to be women and have milder sleep apnea. Persistent PLMS share clinical characteristics with PLMS in general population.


Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien, IL
Huang TC, Tseng PT, Wu MN, Stubbs B, Carvalho AF, Lin PY, Chen YW, Chen TY, Hsu CY (2019) Periodic limb movements during sleep are associated with cardiovascular diseases: a systematic review and meta-analysis. J Sleep Res 28:e12720. https://doi.org/10.1111/jsr.12720
Giannaki CD, Zigoulis P, Karatzaferi C, Hadjigeorgiou GM, George KP, Gourgoulianis K, Koutedakis Y, Stefanidis I, Sakkas GK (2013) Periodic limb movements in sleep contribute to further cardiac structure abnormalities in hemodialysis patients with restless legs syndrome. J Clin Sleep Med 9:147–153
Scofield H, Roth T, Drake C (2008) Periodic limb movements during sleep: population prevalence, clinical correlates, and racial differences. Sleep 31:1221–1227
Karatas M (2007) Restless legs syndrome and periodic limb movements during sleep: diagnosis and treatment. Neurologist 13:294–301. https://doi.org/10.1097/NRL.0b013e3181422589
Fry JM, DiPhillipo MA, Pressman MR (1989) Periodic leg movements in sleep following treatment of obstructive sleep apnea with nasal continuous positive airway pressure. Chest 96:89–91. https://doi.org/10.1378/chest.96.1.89
Baran AS, Richert AC, Douglass AB, May W, Ansarin K (2003) Change in periodic limb movement index during treatment of obstructive sleep apnea with continuous positive airway pressure. Sleep 26:717–720. https://doi.org/10.1093/sleep/26.6.717
Hedli LC, Christos P, Krieger AC (2012) Unmasking of periodic limb movements with the resolution of obstructive sleep apnea during continuous positive airway pressure application. J Clin Neurophysiol 29:339–344. https://doi.org/10.1097/WNP.0b013e3182624567
Chervin RD, Chung S, O’Brien LM, Hoban TF, Garetz SL, Ruzicka DL, Guire KE, Hodges EK, Felt BT, Giordani BJ, Dillon JE (2014) Periodic leg movements during sleep in children scheduled for adenotonsillectomy: frequency, persistence, and impact. Sleep Med 15:1362–1369. https://doi.org/10.1016/j.sleep.2014.05.004
Yamashiro Y, Kryger MH (1994) Acute effect of nasal CPAP on periodic limb movements associated with breathing disorders during sleep. Sleep 17:172–175. https://doi.org/10.1093/sleep/17.2.172
Budhiraja R, Javaheri S, Pavlova MK, Epstein LJ, Omobomi O, Quan SF (2020) Prevalence and correlates of periodic limb movements in OSA and the effect of CPAP therapy. Neurology 94:e1820–e1827. https://doi.org/10.1212/WNL.0000000000008844
Aritake-Okada S, Namba K, Hidano N, Asaoka S, Komada Y, Usui A, Matsuura M, Inoue Y (2012) Change in frequency of periodic limb movements during sleep with usage of continuous positive airway pressure in obstructive sleep apnea syndrome. J Neurol Sci 317:13–16. https://doi.org/10.1016/j.jns.2012.03.013
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, Zucconi M, Ferri R, Trenkwalder C, Lee HB (2014) Restless legs syndrome/Willis–Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria–history, rationale, description, and significance. Sleep Med 15:860–873
Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MWJS (2011) The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath 15:377–384
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA, Task PAPT, F, American Academy of Sleep M, (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4:157–171
Iber C, Ancoli-Israel S, Chesson A, Quan S (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, vol 1. American Academy of Sleep Medicine, Westchester
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus C, Vaughn BV (2012) The AASM manual for the scoring of sleep and associated events. Rules, Terminology and Technical Specifications, Darien, Illinois, American Academy of Sleep Medicine 176:2012
Manconi M, Zavalko I, Bassetti CL, Colamartino E, Pons M, Ferri RJS (2014) Respiratory-related leg movements and their relationship with periodic leg movements during sleep. Sleep 37:497–504
Seo WH, Guilleminault CJC (2012) Periodic leg movement, nasal CPAP, and expiratory muscles. Chest 142:111–118
Manconi M, Zavalko I, Fanfulla F, Winkelman JW, Fulda SJS (2015) An evidence-based recommendation for a new definition of respiratory-related leg movements. Sleep 38:295–304
Schipper MH, Alvarez-Estevez D, Jellema K, Verbraecken J, Fulda S, Rijsman RMJSM (2020) Sleep-related leg movements in obstructive sleep apnea: definitions, determinants, and clinical consequences. Sleep Med 75:131–140
Fulda S, Heinzer R, Haba-Rubio JJS (2018) Characteristics and determinants of respiratory event–associated leg movements. Sleep 41:zsx206
Haba-Rubio J, Marti-Soler H, Tobback N, Andries D, Marques-Vidal P, Vollenweider P, Preisig M, Heinzer R (2018) Clinical significance of periodic limb movements during sleep: the HypnoLaus study. Sleep Med 41:45–50. https://doi.org/10.1016/j.sleep.2017.09.014
Al-Alawi A, Mulgrew A, Tench E, Ryan CF (2006) Prevalence, risk factors and impact on daytime sleepiness and hypertension of periodic leg movements with arousals in patients with obstructive sleep apnea. J Clin Sleep Med 2:281–287
Leary EB, Moore HEt, Schneider LD, Finn LA, Peppard PE, Mignot E (2018) Periodic limb movements in sleep: prevalence and associated sleepiness in the Wisconsin Sleep Cohort. Clin Neurophysiol 129:2306-2314. https://doi.org/10.1016/j.clinph.2018.08.022
Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lesperance P (1997) Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord 12:61–65. https://doi.org/10.1002/mds.870120111
Morgenthaler TI, Kagramanov V, Hanak V, Decker PA (2006) Complex sleep apnea syndrome: is it a unique clinical syndrome? Sleep 29:1203–1209. https://doi.org/10.1093/sleep/29.9.1203
Narkiewicz K, Somers VK (1997) The sympathetic nervous system and obstructive sleep apnea: implications for hypertension. J Hypertens 15:1613–1619. https://doi.org/10.1097/00004872-199715120-00062
Guggisberg AG, Hess CW, Mathis J (2007) The significance of the sympathetic nervous system in the pathophysiology of periodic leg movements in sleep. Sleep 30:755–766. https://doi.org/10.1093/sleep/30.6.755
Trotti LM, Bliwise DL, Greer SA, Sigurdsson AP, Gudmundsdottir GB, Wessel T, Organisak LM, Sigthorsson T, Kristjansson K, Sigmundsson T, Rye DB (2009) Correlates of PLMs variability over multiple nights and impact upon RLS diagnosis. Sleep Med 10:668–671. https://doi.org/10.1016/j.sleep.2008.06.009
Lee S-A, Paek J-H, Han S-H (2016) REM-related sleep-disordered breathing is associated with depressive symptoms in men but not in women. Sleep Breath 20:995–1002
Yang C, White DP, Winkelman JW (2005) Antidepressants and periodic leg movements of sleep. Biol Psychiatry 58:510–514. https://doi.org/10.1016/j.biopsych.2005.04.022
Author information
Authors and Affiliations
Contributions
Conceptualization: Sang-Ahm Lee; Methodology: Sang-Ahm Lee; Writing—Original draft preparation: Sang-Ahm Lee; Reviewing, Editing, and Supervision: Sang-Ahm Lee; Data curation: Hyo Jae Kim, Soo Jeong Kim, and So Young Lee; Formal analysis: Hyo Jae Kim.
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Asan Medical Center approved this study.
Consent to participate
This was a retrospective study based on records, and formal consent was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, SA., Kim, S.J., Lee, S.Y. et al. Clinical characteristics of periodic limb movements during sleep categorized by continuous positive airway pressure titration polysomnography in patients with obstructive sleep apnea. Sleep Breath 26, 251–257 (2022). https://doi.org/10.1007/s11325-021-02387-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02387-z