Abstract
Purpose
The objective of this study was to evaluate the prevalence, the clinical characteristics, and the possible predictors of Chinese patients with positional obstructive sleep apnea (POSA) according to the Amsterdam Positional Obstructive Sleep Apnea Classification (APOC).
Methods
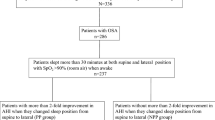
A retrospective study in the sleep unit of Peking Union Medical College Hospital was conducted to analyze the clinical and polysomnography data of Chinese patients with obstructive sleep apnea (OSA).
Results
Of 372 patients with OSA, 54% met the APOC criteria for POSA. The prevalence of POSA was significantly higher in women with OSA than in men. Chinese patients with POSA had a lower apnea–hypopnea index, oxygen desaturation index, and the percentage of time spent at oxygen saturation below 90% in total sleep time; and a higher mean oxygen saturation (SaO2) and minimum SaO2 during sleep, which were remarkable in the APOC I group. By multivariate logistic regression analyses, the higher mean SaO2 (≥95%) during sleep and mild and moderate OSA were positive predictors of POSA. Mild and moderate OSA was the independent predictor of POSA in women. Higher mean SaO2 (≥95%) during sleep was the independent predictor of POSA in men.
Conclusion
According to the APOC, the prevalence of POSA is high in Chinese patients with OSA, especially in women. Chinese patients with POSA had less severe OSA and a lower degree of nocturnal hypoxia, which was remarkable in the APOC I group.
Similar content being viewed by others
Abbreviations
- OSA:
-
Obstructive sleep apnea
- POSA:
-
Positional obstructive sleep apnea
- BMI:
-
Body mass index
- NPOSA:
-
Nonpositional obstructive sleep apnea
- AHI:
-
Apnea-hypopnea index
- APOC:
-
Amsterdam Positional Obstructive Sleep Apnea Classification
- TST:
-
Total sleep time
- BSP:
-
Best sleeping position
- WSP:
-
Worst sleeping position
- PT:
-
Positional therapy
- CPAP:
-
Continuous positive airway pressure
- PSG:
-
Polysomnography
- AASM:
-
American Academy of Sleep Medicine criteria
- ODI:
-
Oxygen desaturation index
- SIT90% :
-
The percentage of time spent at oxygen saturation below 90% in total sleep time
- SaO2 :
-
Oxygen saturation
- REM:
-
Rapid eye movement sleep
- NREM:
-
Non-rapid eye movement sleep
References
Veasey SC, Rosen IM (2019) Obstructive sleep apnea in adults. N Eng J Med 380(15):1442–1449. https://doi.org/10.1056/NEJMcp1816152
Oksenberg A, Gadoth N (2014) Are we missing a simple treatment for most adult sleep apnea patients? The avoidance of the supine sleep position. J Sleep Res 23(2):204–210. https://doi.org/10.1111/jsr.12097
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8):687–698. https://doi.org/10.1016/s2213-2600(19)30198-5
Mo JH, Lee CH, Rhee CS, Yoon IY, Kim JW (2011) Positional dependency in Asian patients with obstructive sleep apnea and its implication for hypertension. Arch Otolaryngol-Head Neck Surg 137(8):786–790. https://doi.org/10.1001/archoto.2011.122
Mador MJ, Kufel TJ, Magalang UJ, Rajesh SK, Watwe V, Grant BJ (2005) Prevalence of positional sleep apnea in patients undergoing polysomnography. Chest 128(4):2130–2137. https://doi.org/10.1378/chest.128.4.2130
O'Driscoll DM, Landry SA, Pham J, Young A, Sands SA, Hamilton GS, Edwards BA (2019) The physiological phenotype of obstructive sleep apnea differs between Caucasian and Chinese patients. Sleep 42(11). https://doi.org/10.1093/sleep/zsz186
Joosten SA, O'Driscoll DM, Berger PJ, Hamilton GS (2014) Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev 18(1):7–17. https://doi.org/10.1016/j.smrv.2013.01.005
Lee S-A, Paek J-H, Chung Y-S, Kim WS (2017) Clinical features in patients with positional obstructive sleep apnea according to its subtypes. Sleep Breathing 21(1):109–117. https://doi.org/10.1007/s11325-016-1379-z
Huang YC, Lin CY, Lan CC, Wu YK, Lim CS, Huang CY, Huang HL, Yeh KH, Liu YC, Yang MC (2014) Comparison of cardiovascular co-morbidities and CPAP use in patients with positional and non-positional mild obstructive sleep apnea. BMC Pulm Med 14:153. https://doi.org/10.1186/1471-2466-14-153
Drager LF, Bortolotto LA, Lorenzi MC, Figueiredo AC, Krieger EM, Lorenzi-Filho G (2005) Early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med 172(5):613–618. https://doi.org/10.1164/rccm.200503-340OC
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Eng J Med 342(19):1378–1384. https://doi.org/10.1056/nejm200005113421901
Alvarez D, Arroyo CA, de Frutos JF, Crespo A, Cerezo-Hernandez A, Gutierrez-Tobal GC, Vaquerizo-Villar F, Barroso-Garcia V, Moreno F, Ruiz T, Hornero R, del Campo F (2020) Assessment of nocturnal autonomic cardiac imbalance in positional obstructive sleep apnea. A multiscale nonlinear approach. Entropy 22(12). https://doi.org/10.3390/e22121404
Cartwright RD (1984) Effect of sleep position on sleep apnea severity. Sleep 7(2):110–114. https://doi.org/10.1093/sleep/7.2.110
Bignold JJ, Mercer JD, Antic NA, McEvoy RD, Catcheside PG (2011) Accurate position monitoring and improved supine-dependent obstructive sleep apnea with a new position recording and supine avoidance device. J Clin Sleep Med: JCSM: Official Publ Am Acad Sleep Med 7(4):376–383. https://doi.org/10.5664/jcsm.1194
Kim KT, Cho YW, Kim DE, Hwang SH, Song ML, Motamedi GK (2016) Two subtypes of positional obstructive sleep apnea: supine-predominant and supine-isolated. Clin Neurophysiol: Official J Int Federation Clin Neurophysiol 127(1):565–570. https://doi.org/10.1016/j.clinph.2015.06.009
Lee SA, Paek JH, Chung YS, Kim WS (2017) Clinical features in patients with positional obstructive sleep apnea according to its subtypes. Sleep Breathing = Schlaf Atmung 21(1):109–117. https://doi.org/10.1007/s11325-016-1379-z
Frank MH, Ravesloot MJ, van Maanen JP, Verhagen E, de Lange J, de Vries N (2015) Positional OSA part 1: Towards a clinical classification system for position-dependent obstructive sleep apnoea. Sleep Breathing = Schlaf Atmung 19(2):473–480. https://doi.org/10.1007/s11325-014-1022-9
Ravesloot MJ, Frank MH, van Maanen JP, Verhagen EA, de Lange J, de Vries N (2016) Positional OSA part 2: retrospective cohort analysis with a new classification system (APOC). Sleep Breathing = Schlaf Atmung 20(2):881–888. https://doi.org/10.1007/s11325-015-1206-y
Permut I, Diaz-Abad M, Chatila W, Crocetti J, Gaughan JP, D'Alonzo GE, Krachman SL (2010) Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. J Clin Sleep Med: JCSM : Official Publ Am Acad Sleep Med 6(3):238–243
Kulkas A, Duce B, Töyräs J, Seppä J, Leppänen T (2020) Comparison of the effect of weight change, simulated computational continuous positive airway pressure treatment and positional therapy on severity of sleep apnea. J Sleep Res:e13070. https://doi.org/10.1111/jsr.13070
Dieltjens M, Vroegop AV, Verbruggen AE, Wouters K, Willemen M, De Backer WA, Verbraecken JA, Van de Heyning PH, Braem MJ, de Vries N, Vanderveken OM (2015) A promising concept of combination therapy for positional obstructive sleep apnea. Sleep Breathing 19(2):637–644. https://doi.org/10.1007/s11325-014-1068-8
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med: JCSM: Official Publ Am Acad Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Teerapraipruk B, Chirakalwasan N, Simon R, Hirunwiwatkul P, Jaimchariyatam N, Desudchit T, Charakorn N, Wanlapakorn C (2012) Clinical and polysomnographic data of positional sleep apnea and its predictors. Sleep Breathing = Schlaf Atmung 16(4):1167–1172. https://doi.org/10.1007/s11325-011-0627-5
Duce B, Kulkas A, Langton C, Toyras J, Hukins C (2017) Amsterdam positional OSA classification: the AASM 2012 recommended hypopnoea criteria increases the number of positional therapy candidates. Sleep Breathing = Schlaf Atmung 21(2):411–417. https://doi.org/10.1007/s11325-016-1432-y
Mohsenin V (2001) Gender differences in the expression of sleep-disordered breathing: role of upper airway dimensions. Chest 120(5):1442–1447. https://doi.org/10.1378/chest.120.5.1442
Oksenberg A, Gadoth N, Töyräs J, Leppänen T (2020) Prevalence and characteristics of positional obstructive sleep apnea (POSA) in patients with severe OSA. Sleep Breathing = Schlaf Atmung 24(2):551–559. https://doi.org/10.1007/s11325-019-01897-1
Chang ET, Shiao GM (2008) Craniofacial abnormalities in Chinese patients with obstructive and positional sleep apnea. Sleep Med 9(4):403–410. https://doi.org/10.1016/j.sleep.2007.04.024
McNicholas WT, Bonsignore MR, Lévy P, Ryan S (2016) Mild obstructive sleep apnoea: clinical relevance and approaches to management. Lancet Respir Med 4(10):826–834. https://doi.org/10.1016/s2213-2600(16)30146-1
Walsh JH, Maddison KJ, Platt PR, Hillman DR, Eastwood PR (2008) Influence of head extension, flexion, and rotation on collapsibility of the passive upper airway. Sleep 31(10):1440–1447
van Kesteren ER, van Maanen JP, Hilgevoord AA, Laman DM, de Vries N (2011) Quantitative effects of trunk and head position on the apnea hypopnea index in obstructive sleep apnea. Sleep 34(8):1075–1081. https://doi.org/10.5665/sleep.1164
Acknowledgments
The authors would like to thank Hairong Zhang and Shuning Li for their help in collecting data.
Availability of data and material
The data used or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Funding
The National Key Research and Development Project (No. SQ2018YFC200148) and the National Natural Science Foundation of China (No. 81570085) funded this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Xiaona Wang, Rong Huang, and Jinmei Luo. The first draft of the manuscript was written by Xiaona Wang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Research Ethics Committee of Peking Union Medical College Hospital approved this study with a waiver of patient consent (protocol number S-K1190).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 46.7 kb)
Rights and permissions
About this article
Cite this article
Wang, X., Luo, J., Huang, R. et al. Preliminary study on clinical characteristics of Chinese patients with positional obstructive sleep apnea. Sleep Breath 26, 67–74 (2022). https://doi.org/10.1007/s11325-021-02346-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02346-8