Abstract
Objective
Obstructive sleep apnea syndrome (OSAS) may affect voice performance due to alterations that occur in the upper respiratory tract. The aim of the study was to assess the effect of OSAS and continuous positive airway pressure (CPAP) treatment on voice performance.
Materials and methods
Twenty-seven patients with moderate to severe OSAS (apnea-hypopnea index ≥15/h) who underwent polysomnographic examination and 28 age- and gender-matched normal control subjects were enrolled in the study. The patients and the control subjects completed Voice Handicap Index (VHI) questionnaires, and their acoustic voice analyses were performed. Fundamental frequency (F0), jitter %, and shimmer % parameters were statistically compared. Acoustic analyses were performed again 1 month after regular CPAP use in OSAS patients, and the parameters before and after the treatment were compared.
Results
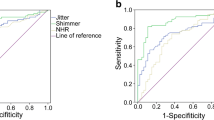
F0 was 160.82 Hz, jitter was 0.70 %, shimmer was 1.05 %, and VHI was 1.18 in the control group. In OSAS patients before CPAP treatment, F0 was 157.04 Hz, jitter was 0.82 %, shimmer was 1.33 %, and VHI was 13.11. These results showed that shimmer and VHI parameters were significantly worse in OSAS patients. After CPAP treatment, F0 was 169.19 Hz, jitter was 0.62 %, shimmer was 0.93 % and VHI was 5.00. The differences were statistically significant in all parameters.
Conclusion
The acoustic parameters of OSAS patients differed from those of the normal control subjects. The patients’ voice performance improved after a regular use of CPAP treatment for 1 month.
Similar content being viewed by others
References
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619
Köktürk O, Tatlicioglu T, Kemaloğlu Y, Fırat H, Çetin N (1997) Habituel horlaması olan olgularda obstrüktif sleep apne sendromu prevelansı. Tüberkülöz ve Toraks Dergisi 45:7–11
Han D, Xu W, Hu R, Zhang L (2012) Voice function following Han’s uvulopalatopharyngoplasty. J Laryngol Otol 126:47–51
Behrman A, Shikowitz MJ, Dailey S (2002) The effect of upper airway surgery on voice. Otolaryngol Head Neck Surg 127:36–42
Grote L, Hedner J, Peter JH (2000) Sleep-related breathing disorder is an independent risk factor for uncontrolled hypertension. J Hypertens 18:679–685
Ryan CF, Lowe AA, Li D, Fleetham JA (1991) Magnetic resonance imaging of the upper airway in obstructive sleep apnea before and after chronic nasal continuous positive airway pressure therapy. Am Rev Respir Dis 144:939–944
Shrivastava D (2014) Impact of sleep-disordered breathing treatment on upper airway anatomy and physiology. Sleep Med 15:733–741
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, Vaughn BV, for the American Academy of Sleep Medicine (2014) The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.0.3. www.aasmnet.org. Darien, Illinois, American Academy of Sleep Medicine
Baken RJ (1987) Clinical measurement of speech and voice. Allyn and Bacon, Needham Heights
Hirano M (1981) Clinical examination of voice. Springer, Vienna
Kılıç MA (2010) Evaluation of the patient with voice problem by objective and subjective methods. Curr Pract ORL 6:257–265
Morton LL, Diubaldo D (1993) Circadian differences in the dichotic processing of voicing. Int J Neurosci 68:43–52
Subramaniam V, Kumar P (2009) Impact of tonsillectomy with or without adenoidectomy on the acoustic parameters of the voice: a comparative study. Arch Otolaryngol Head Neck Surg 135:966–969
Kim YH, Lee SH, Park CW, Cho JH (2013) Nasalance change after sinonasal surgery: analysis of voice after septoturbinoplasty and endoscopic sinus surgery. Am J Rhinol Allergy 27:67–70
Dejonckere PH, Bradley P, Clemente P, Cornut G, Crevier-Buchman L, Friedrich G et al (2001) A basic protocol for functional assessment of voice pathology, especially for investigating the efficacy of (phonosurgical) treatments and evaluating new assessment techniques. Guideline elaborated by the Committee on Phoniatrics of the European Laryngological Society (ELS). Eur Arch Otorhinolaryngol 258:77–82
Hogikyan ND, Sethuraman G (1999) Validation of an instrument to measure voice-related quality of life (V-RQOL). J Voice 13:557–569
Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS (1997) The voice handicap index (VHI): development and validation. Am J Speech Lang Pathol 6:66–70
Hsiung MW, Pai L, Wang HW (2002) Correlation between voice handicap index and voice laboratory measurements in dysphonic patients. Eur Arch Otorhinolaryngol 259:97–99
Wheeler KM, Collins SP, Sapienza CM (2006) The relationship between VHI scores and specific acoustic measures of mildly disordered voice production. J Voice 20:308–317
Birkent H, Soken H, Akcam T, Karahatay S, Gerek M (2008) The effect of radiofrequency volumetric tissue reduction of soft palate on voice. Eur Arch Otorhinolaryngol 265:195–198
Van Lierde KM, Van Borsel J, Moerman M, Van Cauwenberge P (2002) Nasalance, nasality, voice, and articulation after uvulopalatopharyngoplasty. Laryngoscope 112:873–878
Greene JS, Zipfel TE, Harlor M (2004) The effect of uvulopalatopharyngoplasty on the nasality of voice. J Voice 18:423–430
Bertino G, Matti E, Migliazzi S, Pagella F, Tinelli C, Benazzo M (2006) Acoustic changes in voice after surgery for snoring: preliminary results. Acta Otorhinolaryngol Ital 26:110–114
Abu El-ella MY, Eldin HE, Malki KH, Samir MM, Abd Al-Naser NH, Mohamed AA (2010) Effect of classic uvulopalatopharyngoplasty and laser-assisted uvulopalatopharyngoplasty on voice acoustics and speech nasalance. Ann Saudi Med 230:459–463
Mora R, Jankowska B, Crippa B, Dellepiane M, Bavazzano M, Guastini L et al (2009) Effects of uvulopalatopharyngoplasty with Harmonic Scalpel on speech and voice. Eur Arch Otorhinolaryngol 266:1989–1994
Corda L, Redolfi S, Montemurro LT, La Piana GE, Bertella E, Tantucci C (2009) Short- and long-term effects of CPAP on upper airway anatomy and collapsibility in OSAH. Sleep Breath 13:187–193
Hamdan AL, Sabra O, Rifai H, Tabri D, Hussari A (2008) Vocal changes in patients using nasal continuous positive airway pressure. J Voice 22:603–606
Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H et al (2007) Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 30:711–719
Engleman HM, Martin SE, Deary IJ, Douglas NJ (1994) Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet 343:572–575
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Atan, D., Özcan, K.M., İkincioğulları, A. et al. The effect of obstructive sleep apnea syndrome and continuous positive airway pressure treatment on voice performance. Sleep Breath 19, 777–782 (2015). https://doi.org/10.1007/s11325-014-1092-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-014-1092-8