Abstract
Rationale
Temporomandibular disorder (TMD) has been the most common contraindication for mandibular advancement device (MAD) as a treatment for obstructive sleep apnea syndrome (OSAS). Exercising the mandible is a recommended form of therapy for TMD.
Objectives
To assess the efficacy of mandibular exercises in the control of pain, changes of quality of life and to assess the impact of MAD compliance in OSAS patients with previously diagnosed TMD.
Methods
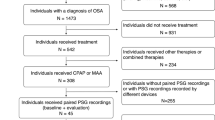
A blind, randomized, and controlled trial was used to evaluate 29 OSAS patients with TMDs were divided in two groups: the exercise support therapy (ST) and placebo therapy (PT), who were evaluated prior to and 120 days after MAD treatment. Treatment outcomes were measured using the Fletcher and Luckett sleep questionnaire, Epworth sleepiness scale, SF-36 inventory of quality of life, polysomnography, diary of MAD usage, and the research diagnostic criteria for TMD.
Measurements and main results
ST group showed significant improvement in their sleep quality and life quality when compared to the PT group (p < 0.05). Higher number of patients with persistent pain was observed in the PT group (p = 0.01). There was a reduction of pain intensity in the ST group, but not in the PT group (p < 0.05). Higher MAD compliance was observed in the ST group (p < 0.05).
Conclusions
Mandibular exercises enable patients with TMD to use MAD; exercises were found to be effective in reducing pain and increasing MAD compliance and produced a significant improvement in the quality of life and quality of sleep.







Similar content being viewed by others
References
Gotsopoulos H, Chen C, Qian J, Cistulli PA (2002) Oral appliance therapy improves symptoms in obstructive sleep apnea: a randomized, controlled trial. Am J Respir Crit Care Med 166:743–748
Chan AS, Lee RW, Cistulli PA (2007) Dental appliance treatment for obstructive sleep apnea. Chest 132:693–699
Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W (2006) Oral appliances for snoring and obstructive sleep apnea: a review. Sleep 29:244–262
Hoffstein V (2007) Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath 11:1–22
Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Owens J, Pancer JP (2006) Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: an update for 2005. Sleep 29:240–243
Bloch KE, Iseli A, Zhang JN, Xie X, Kaplan V, Stoeckli PW, Russi EW (2000) A randomized controlled crossover trial of two appliances for sleep apnea treatment. Am J Respir Crit Care Med 162:246–251
Fritsch KM, Iseli A, Russi EW, Bloch KE (2001) Side effects of mandibular advancement devices for sleep apnea treatment. Am J Respir Crit Care Med 164:813–818
Johnston CD, Gleadhill IC, Cinnamond MJ, Gabbey J, Burden DJ (2002) Mandibular advancement appliances and obstructive sleep apnoea: a randomized clinical trial. Eur J Orthod 24:251–262
Almeida FR, Bittencourt LR, de Almeida CI, Tsuiki S, Lowe AA, Tufik S (2002) Effects of mandibular posture on obstructive sleep apnea severity and the temporomandibular joint in patients fitted with an oral appliance. Sleep 25:507–513
Petit FX, Pépin JL, Bettega G, Sadek H, Raphaël B, Lévy P (2002) Mandibular advancement devices: rate of contraindications in 100 consecutive obstructive apnea patients. Am J Respir Crit Care Med 166:274–278
Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA (2001) A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med 163:1457–1461
Pitsis AJ, Darendeliler MA, Gotsopoulos H, Petocz P, Cistulli PA (2002) Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med 166:860–864
Hammond RJ, Gotsopoulos H, Shen G, Petocz P, Cistulli PA, Darendeliler MA (2007) A follow-up study of dental and skeletal changes associated with mandibular advancement splint use in obstructive sleep apnea. Am J Orthod Dentofacial Orthop 132:806–814
Marklund M, Franklin KA (2007) Long-term effects of mandibular repositioning appliances on symptoms of sleep apnoea. J Sleep Res 16:414–420
Cooper BC, Kleinberg I (2007) Examination of a large patient population for the presence of symptoms and sings of temporomandibular disorders. Cranio 25:114–126
Selaimen CM, Jeronymo JC, Brilhante DP, Grossi ML (2006) Sleep and depression as risk indicators for temporomandibular disorders in a cross-cultural perspective: a case-control study. Int J Prosthodont 19:154–161
Oliveira AS, Dias EM, Contato RG, Berzin F (2006) Prevalence study of signs and symptoms of temporomandibular disorders in Brazilian college students. Braz Oral Res 20:3–7
Conti PC, Ferreira PM, Pegoraro LF, Conti JV, Salvador MC (1996) A cross-sectional study of prevalence and etiology of signs and symptoms of temporomandibular disorders in high school and university students. J Orofac Pain 10:254–262
Okeson JP (2008) General considerations in the treatment of temporomandibular disorders. In: Okeson JP (ed) Management of temporomandibular disorders and occlusion, 6th edn. Mosby, St. Louis, pp 358–361
Reissmann DR, John MT, Schierz O, Wassell RW (2007) Functional and psychosocial impact related to specific temporomandibular disorder diagnoses. J Dent 35:643–650
John MT, Reissmann DR, Schierz O, Wassell RW (2007) Oral health-related quality of life in patients with temporomandibular disorders. J Orofac Pain 21:46–54
Michelotti A, Steenks MH, Farella M, Parisini F, Cimino R, Martina R (2004) The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: short-term results of a randomized clinical trial. J Orofac Pain 18:114–125
Michelotti A, de Wijer A, Steenks M, Farella M (2005) Home-exercise regimes for the management of non-specific temporomandibular disorders. J Oral Rehabil 32:779–885
Nicolakis P, Erdogmus B, Kopf A, Djaber-Ansari A, Piehslinger E, Fialka-Moser V (2000) Exercise therapy for craniomandibular disorders. Arch Phys Med Rehabil 81:1137–1142
Nicolakis P, Erdogmus B, Kopf A, Ebenbichler G, Kollmitzer J, Piehslinger E, Fialka-Moser V (2001) Effectiveness of exercise therapy in patients with internal derangement of the temporomandibular joint. J Oral Rehabil 28:1158–1164
Nicolakis P, Erdogmus B, Kopf A, Nicolakis M, Piehslinger E, Fialka-Moser V (2002) Effectiveness of exercise therapy in patients with myofascial pain dysfunction syndrome. J Oral Rehabil 29:362–368
Yoda T, Sakamoto I, Imai H, Honma Y, Shinjo Y, Takano A, Tsukahara H, Morita S, Miyamura J, Yoda Y, Sasaki Y, Tomizuka K, Takato T (2003) A randomized controlled trial of therapeutic exercise for clicking due to disk anterior displacement with reduction in the temporomandibular joint. Cranio 21:10–16
Yoda T, Sakamoto I, Imai H, Ohashi K, Hoshi K, Kusama M, Kano A, Mogi K, Tsukahara H, Morita S, Miyamura J, Yoda Y, Ida Y, Abe M, Takano A (2006) Response of temporomandibular joint intermittent closed lock to different treatment modalities: a multicenter survey. Cranio 24:130–136
American Academy of Sleep Medicine (2005) The international classification of sleep disorders, 2nd ed. Diagnostic and coding manual. American Academy of Sleep Medicine, Westchester, IL
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6:301–355
Pereira FJ Jr, Favilla EE, Dworkin SF, Huggins K (2004) Research diagnostic criteria for temporomandibular disorders (RDC/TMD): formal translation to Portuguese. J Bras Clin Odontol Integr 8:384–395
Kosminsky M, Lucena LBS, Siqueira JTT, Pereira FJ Jr, Góes PSA (2004) Cultural adaptation of the “Researche diagnostic criteria for tempodomandibular disorders: axis II” questionnaire. J Bras Clin Odontol Integr 8:51–61
Fletcher EC, Luckett RA (1991) The effect of positive reinforcement on hourly compliance in nasal continuous positive airway pressure users with obstructive sleep apnea. Am Rev Respir Dis 143:936–941
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
McHorney CA, Ware JE Jr, Raczek AE (1993) The MOS 36-item short form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31:247–263
Rechtschaffen A, Kales A (1968) A manual of standardized technology, techniques and scoring system for sleep stages of human subjects. Brain Information Service/Brain Research Institute/UCLA, Los Angeles, CA
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine task force. Sleep 22:667–689
American Sleep Disorders Association (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:173–184
Travel JG, Simons DG (1983) Myofascial pain and dysfunction: the trigger point manual. Williams and Wilkins, Baltimore
Shadaba A, Battagel JM, Owa A, Croft CB, Kotecha BT (2000) Evaluation of the Herbst mandibular advancement splint in the management of patients with sleep-related breathing disorders. Clin Otolaryngol Allied Sci 25:404–412
Bates CJ, McDonald JP (2006) Patients’ and sleeping partners’ experience of treatment for sleep-related breathing disorders with a mandibular repositioning splint. Br Dent J 200:95–101
Barnes M, McEvoy RD, Banks S, Tarquinio N, Murray CG, Vowles N, Pierce RJ (2004) Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med 170:656–664
Engleman HM, McDonald JP, Graham D, Lello GE, Kingshott RN, Coleman EL, Mackay TW, Douglas NJ (2002) Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 166:855–859
Chervin RD, Aldrich MS (1999) The Epworth sleepiness scale may not reflect objective measures of sleepiness or sleep apnea. Neurology 52:125–131
Clark GT (1998) Mandibular advancement devices and sleep disordered breathing. Sleep Med Rev 2:163–174
Cunali PA, Almeida FR, Santos CD, Valdrighi NY, Nascimento LS, Dal-Fabbro C, Tufik S, Bittencourt LRA (2009) Prevalence of temporomandibular disorders in obstructive sleep apnea patients referred for oral appliance therapy. J Orofac Pain 23:339–344
McGown AD, Makker HK, Battagel JM, L’Estrange PR, Grant HR, Spiro SG (2001) Long-term use of mandibular advancement splints for snoring and obstructive sleep apnoea: a questionnaire survey. Eur Respir J 17:462–466
Ueda H, Almeida FR, Chen H, Lowe AA (2009) Effect of 2 jaw exercises on occlusal function in patients with obstructive sleep apnea during oral appliance therapy: a randomized controlled trial. Am J Orthod Dentofacial Orthop 135:430e1–430e7
Landry ML, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ (2006) Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Int J Prosthodont 19(6):549–556
Acknowledgements
The authors would like to thank the Fundacao de Amparo a Pesquisa do Estado de Sao Paulo (FAPESP, number 2006/04488-4), the FAPESP-Centros de Pesquisa, Inovação e Difusão (CEPID), and the Associacao Fundo de Incentivo a Psicofarmacologia (AFIP) for their support and funding. Sergio Tufik and Lia Rita Azeredo Bittencourt are principal investigators of FAPESP and researchers of Conselho Nacional de Desenvolvimento Científico e Tecnológico.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cunali, P.A., Almeida, F.R., Santos, C.D. et al. Mandibular exercises improve mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath 15, 717–727 (2011). https://doi.org/10.1007/s11325-010-0428-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0428-2