Abstract
Purpose
The present study was designed to determine the cutoff points for the diagnosis of mild-to-moderate and severe protein–energy wasting (PEW) based on dialysis malnutrition score (DMS) and malnutrition inflammation score (MIS), and the sensitivity, specificity, accuracy, area under receiver operating characteristic (ROC) curve, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+) and negative likelihood ratio (LR−) of DMS and MIS in comparison with subjective global assessment (SGA) in hemodialysis (HD) patients.
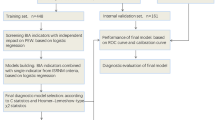
Methods
In this study, 291 HD patients were randomly selected from among 2,302 adult HD patients in Tehran hemodialysis centers. The PEW in these patients was determined by SGA, DMS and MIS.
Results
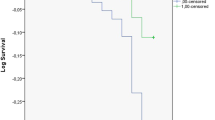
According to the cutoff points derived from the area under ROC curves, scores of 7–13 for DMS represented normal status or without PEW; 14–23, mild-to-moderate PEW; and 24–35, severe PEW. For MIS, scores of 0–7 represented normal status or without PEW; 8–18, mild-to-moderate PEW; and 19–30, severe PEW. In comparison with SGA, the sensitivity, specificity, accuracy, area under ROC curve, PPV, NPV, LR+ and LR− of DMS were 94 %, 88 %, 92 %, 97 %, 93 %, 92 %, 7.8 and 0.07, respectively. Those of MIS were 87 %, 96 %, 91 %, 97 %, 97 %, 83 %, 22.0 and 0.13 in comparison with SGA, respectively.
Conclusion
The results of the present study indicate that the DMS and MIS are almost similar to SGA for identifying PEW in HD patients, but it seems that the DMS is a more appropriate alternative tool for SGA in hospital routine assessments.


Similar content being viewed by others
References
Dukkipati R, Kopple JD (2009) Causes and prevention of protein–energy wasting in chronic kidney failure. Semin Nephrol 29:39–49
Mak RH, Ikizler AT, Kovesdy CP, Raj DS, Stenvinkel P, Kalantar-Zadeh K (2011) Wasting in chronic kidney disease. J Cachex Sarcopenia Muscle 2:9–25
Guarnieri G, Barazzoni R (2011) Fighting protein–energy wasting in chronic kidney disease: a challenge of complexity. J Ren Nutr 21:2–6
Kopple JD (1997) McCollum Award, 1996: protein–energy malnutrition in maintenance dialysis patients. Am J Clin Nutr 65:1544–1557
Kalantar-Zadeh K, Kopple JD (2004) Malnutrition as a risk factor of morbidity and mortality in patients undergoing maintenance dialysis. In: Kopple JD, Massry SG (eds) Kopple and Massry’s nutritional management of renal disease, 2nd edn. Lippincott Williams & Wilkins, Philadelphia, pp 183–198
Kalantar-Zadeh K, Kopple JD (2001) Relative contributions of nutrition and inflammation to clinical outcome in dialysis patients. Am J Kidney Dis 38:1343–1350
Mehrotra R, Kopple JD (2004) Causes of protein–energy malnutrition in chronic renal failure. In: Kopple JD, Massry SG (eds) Kopple and Massry’s nutritional management of renal disease, 2nd edn. Lippincott Williams & Wilkins, Philadelphia, pp 168–182
Morais AAC, Silva MAT, Faintuch J, Vidigal EJ, Costa RA, Lyrio DC, Trindade CR, Pitanga KK (2005) Correlation of nutritional status and food intake in hemodialysis patients. Clinics 60:185–192
Aparicio M, Cano N, Chauveau P, Azar R, Canaud B, Flory A, Laville M, Leverve X (1999) Nutritional status of haemodialysis patients: a French national cooperative study. Nephrol Dial Transplant 14:1679–1686
Pupim LB, Ikizler TA (2004) Assessment and monitoring of uremic malnutrition. J Ren Nutr 14:6–19
Steiber AL, Kalantar-Zadeh K, Secker D, McCarthy M, Sehgal A, McCann L (2004) Subjective global assessment in chronic Kidney disease: a review. J Ren Nutr 14:191–200
de Mutsert R, Grootendorst DC, Boeschoten EW, Brandts H, van Manen JG, Krediet RT, Dekker FW (2009) Subjective global assessment of nutritional status is strongly associated with mortality in chronic dialysis patients. Am J Clin Nutr 89:787–793
Vegine PM, Fernandes AC, Torres MR, Silva MI, Avesani CM (2011) Assessment of methods to identify protein–energy wasting in patients on hemodialysis. J Bras Nefrol 33:55–61
Hull A (2004) Renal Nutrition, 5th edn. Nutrition Dimension, Ashland
Kalantar-Zadeh K, Kleiner M, Dunne E, Lee GH, Luft FC (1999) A modified quantitative subjective global assessment of nutrition for dialysis patients. Nephrol Dial Transplant 14:1732–1738
Kalantar-Zadeh K, Kopple JD, Michael H, Humphreys MH, Block G (2004) Comparing outcome predictability of markers of malnutrition-inflammation complex syndrome in haemodialysis patients. Nephrol Dial Transplant 19:1507–1519
Sacks GS, Dearman K, Replogle WH, Cora VL, Meeks M, Canada T (2000) Use of subjective global assessment to identify nutrition-associated complications and death in geriatric long-term care facility residents. J Am Coll Nutr 19:570–577
McCann L (2005) Pocket guide to nutrition assessment of the patient with chronic kidney disease, 3rd edn. National Kidney Foundation, New York
Burleigh KS (2001) Associations among plasma homocysteine, amino acids and nutritional status in hemodialysis patients [dissertation]. University of Toronto, Toronto
Yamada K, Furuya R, Takita T, Maruyama Y, Yamaguchi Y, Ohkawa S, Kumagai H (2008) Simplified nutritional screening tools for patients on maintenance hemodialysis. Am J Clin Nutr 87:106–113
Beaglehole R, Bonita R, Kjellstrom T (1993) Basic epidemiology. World Health Organization, Geneva
Daugirdas JT, Stone JCV (2001) Physiologic principles and urea kinetic modeling. In: Daugirdas JT, Blake PG, Ing TS (eds) Handbook of dialysis, 3rd edn. Lippincott Williams & Wilkins, Philadelphia, pp 15–45
Tayyem RF, Mrayyan MT, Heath DD, Bawadi HA (2008) Assessment of nutritional status among ESRD patients in Jordanian hospitals. J Ren Nutr 18:281–287
Tapiawala S, Vora H, Patel Z, Badve S, Shah B (2006) Subjective global assessment of nutritional status of patients with chronic renal insufficiency and end stage renal disease on dialysis. J Assoc Physician India 54:923–926
Qureshi AR, Alvestrand A, Danielsson A, Divino-Filho JC, Gutierrez A, Lindholm B, Bergstrom J (1998) Factors predicting malnutrition in hemodialysis patients: a cross-sectional study. Kidney Int 53:773–782
Afshar R, Sanavi S, Izadi-Khah A (2007) Assessment of nutritional status in patients undergoing maintenance hemodialysis: a single-center study from Iran. Saudi J Kidney Dis Transplant 18:397–404
Jahromi SR, Hosseini S, Razeghi E, Ap M, Sadrzadeh H (2010) Malnutrition predicting factors in hemodialysis patients. Saudi J Kidney Dis Transplant 21:846–851
Prasad N, Gupta A, Sinha A, Sharma RK, Kumar A, Kumar R (2008) Changes in nutritional status on follow-up of an incident cohort of continuous ambulatory peritoneal dialysis patients. J Ren Nutr 18:195–201
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
As’habi, A., Tabibi, H., Nozary-Heshmati, B. et al. Comparison of various scoring methods for the diagnosis of protein–energy wasting in hemodialysis patients. Int Urol Nephrol 46, 999–1004 (2014). https://doi.org/10.1007/s11255-013-0638-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-013-0638-1