Abstract
Purpose
Urinary tract infection (UTI) often causes bacteremia, resulting in shock. The purpose of this study is to investigate urological bacteremia and bacteremia shock cases and seek for the clinical factors associated with urological bacteremic shock.
Methods
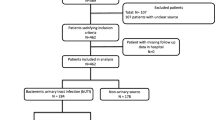
Seventy consecutive cases with bacteremia caused by UTI from the Department of Urology, Kobe University Hospital were studied. These cases were diagnosed from 2000 to 2010 and had full data available for analysis. We investigated the potential clinical factors associated with bacteremic shock (systolic blood pressure ≤90 mmHg with UTI), including: (1) the number of basal general diseases (such as diabetes, malignancy, immune diseases, heart diseases, liver diseases, and kidney diseases), (2) causative bacteria, (3) antibiotics and therapeutic intervention, (4) gram-negative bacteria, (5) resistance to imipenem (which is often used in this infection), and (6) serum white blood cell counts and C-reactive protein (CRP) at the time of diagnosis of bacteremic UTI.
Results
A total of 81 causative bacteria were isolated: 42 cases were gram-negative and 39 were gram-positive bacteria. In detail, Escherichia coli was the most common, followed by Methicillin-resistant Staphylococcus aureus. The comparison data revealed that urological bacteremic shock cases had significantly increased CRP (p < 0.001). Our univariate analyses showed indwelling urinary tract catheters (p = 0.02) as a significant clinical factor associated with urological bacteremic shock and multivariate analyses showed that the presence of indwelling urinary tract catheters before UTI was a significant clinical factor associated with urological bacteremic shock (p = 0.04).
Conclusions
Indwelling urinary catheters before UTI and high CRP were clinical factors associated with urological bacteremic shock. This result should be considered during decision-making for UTI treatments in high risk cases or urological bacteremia cases.
Similar content being viewed by others
References
Bader MS, Hawboldt J, Brooks A (2010) Management of complicated urinary tract infections in the era of antimicrobial resistance. Postgrad Med 122:7–15
Matsumoto T (2001) Urinary tract infections in the elderly. Curr Urol Rep 2:330–333
Ronald A (2003) The etiology of urinary tract infection: traditional and emerging pathogens. Dis Mon 49:71–82
Heyns CF (2012) Urinary tract infection associated with conditions causing urinary tract obstruction and stasis, excluding urolithiasis and neuropathic bladder. World J Urol 30:77–83
Brown PD (2010) Management of urinary tract infections associated with nephrolithiasis. Curr Infect Dis Rep 12:450–454
Geerlings SE (2008) Urinary tract infections in patients with diabetes mellitus: epidemiology, pathogenesis and treatment. Int J Antimicrob Agents 31:S54–S57
Geerlings SE, Stolk RP, Camps MJ et al (2000) Asymptomatic bacteriuria may be considered a complication in women with diabetes. Diabetes Mellitus Women Asymptomatic Bacteriuria Utrecht Study Group. Diabetes Care 23:744–749
Lever A, Mackenzie I (2007) Sepsis: definition, epidemiology, and diagnosis. BMJ 335:879–883
Shubin H, Weil MH (1976) Bacterial shock. JAMA 235:421–424
Dellinger RP, Levy MM, Rhodes A et al (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septicshock, 2012. Intensive Care Med 39:165–228
Clinical and Laboratory Standards Institute (2008) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard 8th edition. Document M07-A8 CLSI, Wayne, PA
YokooA Kumamoto Y, Hirose T (1994) Study on intractable factors in urinary tract infections–multiple regression analysis. Kansenshogaku Zasshi 68:905–915
Nicolle LE (2008) Short-term therapy for urinary tract infection: success and failure. Int J Antimicrob Agents 31:S40–S45
Shigemura K, Arakawa S, Tanaka K et al (2009) Clinical investigation of isolated bacteria from urinary tracts of hospitalized patients and their susceptibilities to antibiotics. J Infect Chemother 15:18–22
Wagenlehner FM, Pilatz A, Weidner W (2011) Urosepsis–from the view of the urologist. Int J Antimicrob Agents 38:S51–S57
Hori J, Yamaguchi S, Watanabe M et al (2008) Clinical investigation of extracorporeal endotoxin adsorption therapy in septic urinary tract infections. Nihon Hinyokika Gakkai Zasshi 99:578–583
Guzmàn CA, Pruzzo C, LiPira G et al (1989) Role of adherence in pathogenesis of Enterococcus faecalis urinary tract infection and endocarditis. Infect Immun 57:1834–1838
Tabibian JH, Gornbein J, Heidari A et al (2008) Uropathogens and host characteristics. J Clin Microbiol 46:3980–3986
Farajnia S, Alikhani MY, Ghotaslou R et al (2009) Causative agents and antimicrobial susceptibilities of urinary tract infections in the northwest of Iran. Int J Infect Dis 13:140–144
Campillo B, Dupeyron C, Richardet JP (2001) Epidemiology of hospital-acquired infections in cirrhotic patients: effect of carriage of methicillin-resistant Staphylococcus aureus and influence of previous antibiotic therapy and norfloxacin prophylaxis. Epidemiol Infect 127:443–450
Wagenlehner FM, Pilatz A, Naber KG et al (2008) Anti-infective treatment of bacterial urinary tract infections. Curr Med Chem 15:1412–1427
Amano T, Matsui F, Takashima H et al (2003) Analysis of patients with septic shock due to urosepsis brought on by ureteral calculi. Hinyokika Kiyo 49:1–4
Savas L, Guvel S, Onlen Y et al (2006) Nosocomial urinary tract infections: micro-organisms, antibiotic sensitivities and risk factors. West Indian Med J 55:188–193
Ludwig E (2008) Urinary tract infections in diabetes mellitus. Orv Hertil 149:597–600
Houdouin V, Bonacorsi S, Bidet P et al (2006) Phylogenetic background and carriage of pathogenicity island-like domains in relation to antibiotic resistance profiles among Escherichia coli urosepsis isolates. J Antimicrob Chemother 58:748–751
Tambyah PA, Oon J (2012) Catheter-associated urinary tract infection. Curr Opin Infect Dis 25:365–370
Acknowledgments
We thank Drs. Fukashi Yamamichi for drafting the manuscript and Yuzo Nakano for data analysis.
Conflict of interest
We have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shigemura, K., Tanaka, K., Osawa, K. et al. Clinical factors associated with shock in bacteremic UTI. Int Urol Nephrol 45, 653–657 (2013). https://doi.org/10.1007/s11255-013-0449-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-013-0449-4