Abstract
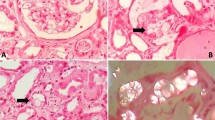
Renal Fanconi syndromes are both clinically challenging and physiologically fascinating. The diagnosis requires a certain index of suspicion to correctly identify the clinical symptomatology and pursue the appropriate laboratory evaluations. The renal Fanconi syndrome (FS) is a defect of proximal tubular function attributable to different rare inherited diseases or acquired disorders caused by a multitude of exogenous agents. It can manifest as complete or incomplete FS, characterized by low molecular weight proteinuria, glucosuria, aminoaciduria, and loss of electrolytes, bicarbonate and lactate. Implementation of new methods and recent findings from urinary proteome pattern in patients with renal FS has led to the identification of new markers for proximal tubular dysfunction. Future combined proteomic and metabonomic studies will provide additional potential biomarkers and may help to gain novel insights in the diagnosis and differentiation of the various forms of FS. Moreover, the observation of poor renal uptake of 99 mTc-DMSA in patients with tubular proteinuria, which is not fully understood yet, may also help to elucidate the individual basis of FS in early stages. This review focuses on the new advances in the evaluation of proximal tubular dysfunction in various forms of Fanconi syndrome.
Similar content being viewed by others
References
Bagga A, Sinha A (2007) Evaluation of renal tubular acidosis. Indian J Pediatr 74:679–686
Bökenkamp A, Ludwig M (2011) Disorders of the renal proximal tubule. Nephron Physiol 118:1–6
Monnens L, Levtchenko E (2008) Evaluation of the proximal tubular function in hereditary renal Fanconi syndrome. Nephrol Dial Transplant 23:2719–2722
Norden AG, Scheinman SJ, Deschodt-Lanckman MM et al (2000) Tubular proteinuria defined by a study of Dent’s (CLCN5 mutation) and other tubular diseases. Kidney Int 57:240–249
Sethi SK, Bagga A, Gulati A et al (2008) Mutations in OCRL1 gene in Indian children with Lowe syndrome. Clin Exp Nephrol 12:358–362
Sethi SK, Ludwig M, Kabra M et al (2009) Vitamin A responsive night blindness in Dent’s disease. Pediatr Nephrol 24:1765–1770
Vilasi A, Cutillas PR, Maher AD et al (2007) Combined proteomic and metabonomic studies in three genetic forms of the renal Fanconi syndrome. Am J Physiol Renal Physiol 293:F456–F467
Norden AG, Gardner SC, Van’t Hoff W et al (2008) Lysosomal enzymuria is a feature of hereditary Fanconi syndrome and is related to elevated CI-mannose-6-P-receptor excretion. Nephrol Dial Transplant 23:2795–2803
Lee BH, Lee SH, Choi HJ et al (2009) Decreased renal uptake of (99 m)Tc-DMSA in patients with tubular proteinuria. Pediatr Nephrol 24:2211–2216
Wu J, Chen YD, Gu W (2010) Urinary proteomics as a novel tool for biomarker discovery in kidney diseases. J Zhejiang Univ-Sci B (Biomed & Biotechnol) 11:227–237
Caubet C, Lacroix C, Decramer S et al (2010) Advances in urinary proteome analysis and biomarker discovery in pediatric renal disease. Pediatr Nephrol 25:27–35
Nesterova G, Gahl W (2008) Nephropathic cystinosis: late complications of a multisystemic disease. Pediatr Nephrol 23:863–878
Wilmer MJG, de Graaf-Hess A, Blom HJ et al (2005) Elevated oxidized glutathione in cystinotic proximal tubular epithelial cells. Bichem Biophys Res Commun 337:610–614
Drube J, Schiffer E, Mischak H et al (2009) Urinary proteome pattern in children with renal Fanconi syndrome. Nephrol Dial Transplant 24:2161–2169
Nielsen R, Courtoy PJ, Jacobsen C et al (2007) Endocytosis provides a major alternative pathway for lysosomal biogenesis in kidney proximal tubular cells. Proc Natl Acad Sci USA 104:5407–5411
Xaidara A, Karavitakis EM, Kosma K, Emma F, Dimitriou E, Michelakakis H (2010) chitotriosidase plasma activity in nephropathic cystinosis. J Inherit Metab Dis: Short report, #168, online. doi:10.1007/s10545-009-1118-8
Bockenhauer D, Bokenkamp A, van’t Hoff W, Levtchenko E, Kist-van Holthe JE, Tasic V, Ludwig M (2008) Renal phenotype in Lowe syndrome: a selective proximal tubular dysfunction. Clin J Am Soc Nephrol 3:1430–1436
Bökenkamp A, Böckenhauer D, Cheong HI, Hoppe B, Tasic V, Unwin R, Ludwig M (2009) Dent-2 disease: a mild variant of Lowe syndrome. J Pediatr 155:94–99
Jänne PA, Suchy SF, Bernard DJ et al (1998) Functional overlap between murine Inpp5b and OCRL1 may explain why deficiency of the murine ortholog for OCRL1 does not cause Lowe syndrome in mice. J Clin Invest 101:2042–2053
Bothwell SP, Farber LW, Hoagland A, Nussbaum RL (2010) Species-specific difference in expression and splice-site choice in Inpp5b, an inositol polyphosphate 5-phosphatase paralogous to the enzyme deficient in Lowe syndrome. Mammal Genome 21:458–466
Bothwell SP, Chan E, Bernardini IM, Kuo YM, Gahl WA, Nussbaum RL (2011) Mouse model for Lowe syndrome/Dent disease 2 renal tubulopathy. J Am Soc Nephrol 22. doi:10.1681/ASN2010050565
Carr G, Simmons NL, Sayer JA (2006) Disruption of clc-5 leads to a redistribution of annexin A2 and promotes calcium crystal agglomeration in collecting duct epithelial cells. Cell Mol Life Sci 63:367–377
Smith AJ, Reed AAC, Loh NY, Thakker RV, Lippiat JD (2009) Characterization of Dent’s disease mutations of CLC-5 reveals a correlation between functional and cell biological consequences and protein structure. Am J Physiol Renal Physiol 296:F390–F397
Wang Y, Bartlett MC, Loo TW, Clarke TM (2006) Specific rescue of cystic fibrosis transmembrane conductance regulator processing mutants using pharmacological chaperones. Mol Pharmacol 70:297–302
Cutillas PR, Norden AGW, Cramer R, Burlingame AL, Unwin RJ (2003) Detection and analysis of urinary peptides by on-line liquid chromatography and mass spectrometry: application to patients with renal Fanconi syndrome. Clin Sci 104:483–490
Cutillas PR, Chalkley RJ, Hansen KC et al (2004) The urinary proteome in Fanconi syndrome implies specifity in the reabsorption of proteins by renal proximal tubule cells. Am J Physiol Renal Physiol 287:F353–F364
Norden AG, Lapsley M, Igarashi T et al (2002) Urinary megalin deficiency implicates abnormal tubular endocytic function in Fanconi syndrome. J Am Soc Nephrol 13:125–133
Tanuma A, Sato H, Takeda T et al (2007) Functional characterization of a novel missense CLCN5 mutation causing alterations in proximal tubular endocytotic machinery in Dent’s disease. Nephron Physiol 107:87–97
Cho HY, Lee BH, Choi HJ, Ha IS, Choi Y, Cheong HI (2008) Renal manifestations of Dent disease and Lowe syndrome. Pediatr Nephrol 23:243–249
Vezzoli G, Zerbi S, Baragetti I, Soldati L, Mora S, Dell’Antonio G, Bianchi G (1997) Nonacidotic proximal tubulopathy transmitted as autosomal dominant trait. Am J Kidney Dis 29:490–495
Bosch AM (2006) Classical galactosaemia revisited. J Inherit Metab Dis 29:516–525
Holton JB, Walter HJ, Tyfield LA (2001) Galactosemia. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The metabolic and molecular basis of inherited disease, vol 8. McGraw-Hill, New York, pp 1553–1583
Alonso-Fernandez JR, Carpinteiro MI, Baleato J, Fidalgo J (2010) Vertical sandwich-type continuous/evaporative TLC with fixed mobile phase volume for separating sugars of clinical relevance in paper-borne urine and blood samples in newborn screening. J Clin Lab Anal 24:106–112
Sturiale L, Barone R, Palmigiano A et al (2008) Multiplexed glycoproteomic analysis of glycosylation disorders by sequential yolk immunoglobulins immunoseparation and MALDI-TOF MS. Proteomics 8:3822–3832
Van Dyk E, Pretorius PJ (2005) DNA damage and repair in mammalian cells exposed to p-hydroxyphenylpyruvic acid. Biochem Biophys Res Commun 338:815–819
Held PK (2006) Disorders of tyrosine metabolism. Mol Genet Metab 88:103–106
Al-Dirbashi OY, Jacob M, Al-Ahaidib LJ et al (2006) Quantification of succinylacetone in urine of hepatorenal tyrosinemia patients by HPLC with fluorescence detection. Clin Chim Acta 365:243–248
Turgeon C, Magera MJ, Allard P et al (2008) Combined newborn screening for succinylacetone, amino acids, and acylcarnitines in dried blood spots. Clin Chem 54:657–664
Bouteldja N, Timson DJ (2010) The biochemical basis of hereditary fructose intolerance. J Inherit Metab Dis 33:105–112
Pronicka E, Adamowicz M, Kowalik A et al (2007) Elevated carbohydrate-deficient transferring (CDT) and its normalization on dietary treatment as a useful biochemical test for hereditary fructose intolerance and galactosemia. Pediatr Res 62:101–105
Quintana E, Sturiale L, Montero R et al. (2009) Secondary disorders of glycosylation in inborn errors of fructose metabolism. J Inherit Metab Dis: Short report, #187, online. doi:10.1007/s10545-009-1219-4
Adamowicz M, Ploski R, Rokicki D et al (2007) Transferrin hypoglycosylation in hereditary fructose intolerance: using the clues and avoiding the pitfalls. J Inherit Metab Dis 30:407
Santer R, Steinmann B (2002) Schaub J (2002) Fanconi-Bickel syndrome—a congenital defect of facilitative glucose transport. Curr Mol Med 2:213–227
Furlan F, Santer R, Vismara E, Santus F, Sersale G, Menni F, Parini R (2006) Bilateral nuclear cataracts as the first neonatal sign of Fanconi-Bickel syndrome. J Inherit Metab Dis 29:685
Santer R, Schneppenheim R, Dombrowski A, Götze H, Steinmann B, Schaub J (1997) Mutations in GLUT2, the gene for the liver-type glucose transporter, in patients with Fanconi-Bickel syndrome. Nat Genet 17:324–326
De Bie P, Muller P, Wijmenga C, Klomp LW (2007) Molecular pathogenesis of Wilson and Menkes disease: correlation of mutations with molecular defects and disease phenotypes. J Med Genet 44:673–688
Roberts EA, Sarkar B (2008) Liver as a key organ in the supply, storage, and excretion of copper. Am J Clin Nutr 88(suppl):851S–854S
Roelofsen H, Balgobind R, Vonk RJ (2004) Proteomic analyzes of copper metabolism in an in vitro model of Wilson disease using surface enhanced laser desorption/ionization-time of flight-mass spectrometry. J Cell Biochem 93:732–740
Huster D, Purnat TD, Burkhead JL et al (2007) High copper selectively alters lipid metabolism and cell cycle machinery in the mouse model of Wilson disease. J Biol Chem 282:8343–8355
Ralle M, Huster D, Vogt S et al (2010) Wilson disease at a single cell level. Intracellular copper trafficking activates compartment-specific responses in hepatocytes. J Biol Chem 285:30875–30883
Skinner R, Pearson ADJ, Price L, Coulthard MG, Craft AW (1990) Nephrotoxicity after ifosfamide. Arch Dis Child 65:732–738
Yaseen Z, Michoudet C, Baverel G, Dubourg L (2008) Mechanisms of the ifosfamide induced inhibition of endocytosis in the rat proximal kidney tubule. Arch Toxicol 82:607–614
Foxall PJ, Singer JM, Hartley JM et al (1997) Urinary proton magnetic resonance studies of early ifosfamide-induced nephrotoxicity and encephalopathy. Clin Cancer Res 3:1507–1518
Ciarimboli G, Holle SK, Vollenbröcker B et al. (2010) New clues for nephrotoxicity induced by ifosfamide: preferential uptake via the human organic cation transporter 2. Mol Pharm. doi:10.1021/mp100329u
Suzuki S, Suzuki J, Kume K et al (1999) Poor renal accumulation of 99 mTc-DMSA in idiopathic tubular proteinuria. Nephron 81:49–54
Frishberg Y, Dinour D, Belostotsky R et al (2009) Dent’s disease manifesting as focal glomerulosclerosis: is it the tip of the iceberg? Pediatr Nehrol 24:2369–2373
Kim SE, Cho JT, Lee DS et al (1995) Poor renal uptake of Tc-99 m DMSA and Tc-99 m MDP in a patient with Fanconi syndrome and near normal glomerular filtration rate. Clin Nucl Med 20:215–219
Hecht H, Ohlsson J, Starck SA (1996) Poor renal uptake of 99mtechnetium-dimercaptosuccinic acid and near-normal 99mtechnetium-mercaptoacetyltriglycine renogram in nephronophthisis. Pediatr Nephrol 10:167–170
Caglar M, Topaloğlu R (2002) Reduced Tc-99m DMSA uptake in a patient with renal tubular acidosis: effect of acid-base imbalance. Ann Nucl Med 16:499–501
Tasic V, Lozanovski VJ, Korneti P, Ristoska-Bojkovska N, Sabolic-Avramovska V, Gucev Z, Ludwig M (2011) Clinical and laboratory features of Macedonian children with OCRL mutations. Pediatr Nephrol (in press)
van Luÿk WH, Ensing GJ, Piers DA (1983) Low renal uptake of 99mTc-DMSA in patients with proximal tubular dysfunction. Eur J Nucl Med 8:404–405
de Lange MJ, Piers DA, Kosterink JG et al (1989) Renal handling of technetium-99m DMSA: evidence for glomerular filtration and peritubular uptake. J Nucl Med 30:1219–1223
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ludwig, M., Sethi, S.K. Novel techniques and newer markers for the evaluation of “proximal tubular dysfunction”. Int Urol Nephrol 43, 1107–1115 (2011). https://doi.org/10.1007/s11255-011-9914-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-011-9914-0