Abstract
Purpose
To investigate patient-reported outcome (PRO) measures in patients with relapsing–remitting multiple sclerosis (RRMS) who transition to secondary progressive multiple sclerosis (SPMS).
Methods
Subjects enrolled in the Comprehensive Longitudinal Investigation of Multiple Sclerosis at Brigham and Women’s Hospital (CLIMB) who completed PRO measures in the RRMS and SPMS phases were identified (n = 52). The PRO measures were Medical Outcomes Study Short-Form 36 Health Survey (SF-36), the Modified Fatigue Impact Scale (MFIS), and the Center for Epidemiologic Studies Depression Scale (CESD). Two control groups of RRMS CLIMB patients who did not progress to SPMS were identified based on different matching criteria related to age, sex, disease duration and Expanded Disability Status Scale (EDSS). Summary statistics for each PRO were calculated at the last RRMS measurement and first SPMS measurement, and the change over this transition was calculated using a paired t-test. Patients who transitioned were compared to the control groups using linear regression to adjust for age, disease duration and EDSS and a mixed model to further account for the matching with a random effect for matched group.
Results
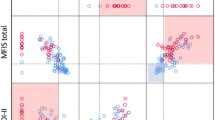
Patients who transitioned from RRMS to SPMS had noticeable deficits in terms of Quality of Life (QOL) and fatigue at the visit prior to the transition. Patients worsened in terms of SF-36 Role Physical (− 3.6 [− 6.6, − 0.7]), Social Functioning (− 3.7 [− 6.4, − 1.0]), and Physical Component Summary (− 2.3 [− 4.5, − 0.1]) during the transition from RRMS to SPMS. When patients who transitioned were compared to the matched subjects, they had worse scores on several outcomes, including Physical Functioning (adjusted mean difference = − 10.8 [− 14.1, − 7.5]), Physical Component Summary (− 5.2 [− 9.3, − 1.0]), fatigue (8.9 [1.7, 16.1]), and depression (3.1 [0.3, 5.9]).
Conclusions
Patients in the period closely preceding transition from RRMS to SPMS have worse physical QOL and fatigue compared to subjects who remain RRMS.
Similar content being viewed by others
Data availability
Anonymized data related to the findings of this analysis are available from the corresponding author, upon reasonable request from qualified investigators.
Code availability
R code for this analysis is available from the corresponding author, upon reasonable request from qualified investigators.
References
Reich, D. S., Lucchinetti, C. F., & Calabresi, P. A. (2018). Multiple sclerosis. New England Journal of Medicine, 378(2), 169–180.
Lublin, F. D., Reingold, S. C., Cohen, J. A., Cutter, G. R., Sørensen, P. S., Thompson, A. J., Wolinsky, J. S., Balcer, L. J., Banwell, B., Barkhof, F., Bebo, B., Jr., Calabresi, P. A., Clanet, M., Comi, G., Fox, R. J., Freedman, M. S., Goodman, A. D., Inglese, M., Kappos, L., Kieseier, B. C., et al. (2014). Defining the clinical course of multiple sclerosis: The 2013 revisions. Neurology, 83(3), 278–286.
Lublin, F. D., Baier, M., & Cutter, G. (2003). Effect of relapses on development of residual deficit in multiple sclerosis. Neurology, 61(11), 1528–1532.
Vukusic, S., & Confavreux, C. (2007). Natural history of multiple sclerosis: Risk factors and prognostic indicators. Current Opinion in Neurology, 20(3), 269–274.
Confavreux, C., & Vukusic, S. (2006). Age at disability milestones in multiple sclerosis. Brain, 129(Pt 3), 595–605.
Tremlett, H., Yinshan, Z., & Devonshire, V. (2008). Natural history of secondary-progressive multiple sclerosis. Multiple Sclerosis, 14(3), 314–324.
Hamidi, V., Couto, E., Ringerike, T., & Klemp, M. (2018). A multiple treatment comparison of eleven disease-modifying drugs used for multiple sclerosis. Journal of Clinical Medicine Research, 10(2), 88–105.
Tur, C., Kalincik, T., Oh, J., Sormani, M. P., Tintoré, M., Butzkueven, H., & Montalban, Xr. (2019). Head-to-head drug comparisons in multiple sclerosis: Urgent action needed. Neurology, 93(18), 793–809.
University of California San Francisco MS-EPIC Team, Cree, B. A. C., Gourraud, P.-A., Oksenberg, J. R., Bevan, C., Crabtree-Hartman, E., Gelfand, J. M., Goodin, D. S., Graves, J., Green, A. J., Mowry, E., Okuda, D. T., Pelletier, D., von Büdingen, H.-C., Zamvil, S. S., Agrawal, A., Caillier, S., Ciocca, C., Gomez, R., Kanner, R., et al. (2016). Long-term evolution of multiple sclerosis disability in the treatment era. Annals of Neurology, 80(4), 499–510.
Manouchehrinia, A., Zhu, F., Piani-Meier, D., Lange, M., Silva, D. G., Carruthers, R., Glaser, A., Kingwell, E., Tremlett, H., & Hillert, J. (2019). Predicting risk of secondary progression in multiple sclerosis: A nomogram. Multiple Sclerosis, 25(8), 1102–1112.
Law, M. T., Traboulsee, A. L., Li, D. K., Carruthers, R. L., Freedman, M. S., Kolind, S. H., & Tam, R. (2019). Machine learning in secondary progressive multiple sclerosis: An improved predictive model for short-term disability progression. Multiple Sclerosis Journal: Experimental Translational and Clinical, 5(4), 2055217319885983.
Lorscheider, J., Buzzard, K., Jokubaitis, V., Spelman, T., Havrdova, E., Horakova, D., Trojano, M., Izquierdo, G., Girard, M., Duquette, P., Prat, A., Lugaresi, A., Grand’Maison, F., Grammond, P., Hupperts, R., Alroughani, R., Sola, P., Boz, C., Pucci, E., & Lechner-Scott, J. (2016). Defining secondary progressive multiple sclerosis. Brain, 139(Pt 9), 2395–2405.
Mahad, D. H., Trapp, B. D., & Lassmann, H. (2015). Pathological mechanisms in progressive multiple sclerosis. Lancet Neurology, 14(2), 183–193.
Ascherio, A., Munger, K. L., Lennette, E. T., Spiegelman, D., Hernán, M. A., Olek, M. J., Hankinson, S. E., & Hunter, D. J. (2001). Epstein–Barr virus antibodies and risk of multiple sclerosis: A prospective study. JAMA, 286(24), 3083–3088.
Levin, L. I., Munger, K. L., Rubertone, M. V., Peck, C. A., Lennette, E. T., Spiegelman, D., & Ascherio, A. (2005). Temporal relationship between elevation of Epstein–Barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis. JAMA, 293(20), 2496–2500.
Gauthier, S. A., Glanz, B. I., Mandel, M., & Weiner, H. L. (2006). A model for the comprehensive investigation of a chronic autoimmune disease: The multiple sclerosis CLIMB study. Autoimmunity Review, 5(8), 532–536.
Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology, 33(11), 1444–1452.
Ware, J. E., Jr., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Fisk, J. D., Pontefract, A., Ritvo, P. G., Archibald, C. J., & Murray, T. J. (1994). The impact of fatigue on patients with multiple sclerosis. Canadian Journal of Neurological Science, 21(1), 9–14.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Patti, F., Cacopardo, M., Palermo, F., Ciancio, M. R., Lopes, R., Restivo, D., & Reggio, A. (2003). Health-related quality of life and depression in an Italian sample of multiple sclerosis patients. Journal of Neurological Sciences, 211(1–2), 55–62.
Pittock, S. J., Mayr, W. T., McClelland, R. L., Jorgensen, N. W., Weigand, S. D., Noseworthy, J. H., & Rodriguez, M. (2004). Quality of life is favorable for most patients with multiple sclerosis: A population-based cohort study. Archives of Neurology, 61(5), 679–686.
Bakshi, R. (2003). Fatigue associated with multiple sclerosis: Diagnosis, impact and management. Multiple Sclerosis, 9(3), 219–227.
Cavallari, M., Palotai, M., Glanz, B. I., Egorova, S., Prieto, J. C., Healy, B. C., Chitnis, T., & Guttmann, C. R. (2016). Fatigue predicts disease worsening in relapsing–remitting multiple sclerosis patients. Multiple Sclerosis, 22(14), 1841–1849.
Feinstein, A. (2011). Multiple sclerosis and depression. Multiple Sclerosis, 17(11), 1276–1281.
Funding
There is no funding source to report for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Brian Healy has received grant support from Analysis Group, Celgene (Bristol-Myers Squibb), Verily, Novartis, Merck Serono, and Genzyme. Jonathan Zurawski reports no disclosures relevant to the manuscript. Tanuja Chitnis has provided advisory board/consulting services to Biogen-Idec, Merck Serono, Novartis, Sanofi, Bayer, Celgene (Bristol-Myers Squibb), and Alexion and has received research support from Verily, Merck Serono, and Novartis. Howard Weiner has received grant support from National Institutes of Health, National Multiple Sclerosis Society, Verily, Google Life Sciences, EMD Serono, Biogen, Teva, and Novartis, has received grant support and provided consulting services to Sanofi and Genentech, has provided personal, consulting, and/or advising services to Tilos, Tiziana, IM Therapeutics, vTv Therapeutics, and MedDay. Bonnie Glanz has received research support from Merck Serono and Verily.
Ethical approval
This study was approved by the Mass General Brigham IRB.
Informed consent
All subjects provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Healy, B.C., Zurawski, J., Chitnis, T. et al. Patient-reported outcomes associated with transition to secondary progressive multiple sclerosis. Qual Life Res 31, 1799–1805 (2022). https://doi.org/10.1007/s11136-021-03034-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-03034-6