Abstract
Purpose
Previous research has demonstrated that lower health-related quality of life (HRQoL) is associated with higher morbidity and mortality, especially in-patient groups. The association of HRQoL with all-cause mortality in community samples requires further investigation. This study aimed to examine whether HRQoL predicts all-cause mortality in older healthy community-dwelling people from Australia and the United States (U.S.) enrolled in the Aspirin in Reducing Events in the Elderly (ASPREE) trial. We also explored whether this association varies by gender or country.
Method
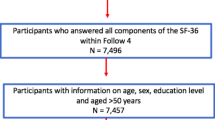
A prospective cohort of 19,106 individuals aged 65–98 years, who were without a dementia diagnosis or a known major life-limiting disease, and completed the 12-item short-form-HRQoL at recruitment (2010–2014). They were followed until June 2017. Cox proportional-hazard models were used to determine the association between the physical (PCS) and mental component scores (MCS) of HRQoL and all-cause mortality, adjusting for sociodemographic factors, health-related behaviours and clinical measures. Hazards ratios were estimated for every 10-unit increase in PCS or MCS.
Results
There were 1052 deaths over a median 4.7-years (interquartile range 3.6–5.7) of follow-up, with 11.9 events per 1000 person-years. Higher PCS was associated with lower all-cause mortality (HR 0.83, 95% CI 0.77, 0.89) in the entire sample, while higher MCS was associated with lower mortality among U.S. participants only (HR 0.78, 95% CI 0.63, 0.95). Gender differences in the association of either PCS or MCS with mortality were not observed.
Conclusion
Our large study provides evidence that HRQoL is inversely associated with all-cause mortality among initially healthy older people.


Similar content being viewed by others
Data availability
All individual participant data (re-identifiable) that underlie the results reported in this Manuscript, are available upon request to qualified researchers without limit of time, subject to approval of the analyses by the Principal Investigators and a standard data sharing agreement. Details regarding requests to access the data will be available through the web site (www.ASPREE.org). The data will then be made available through a web-based data portal safe haven at Monash University, Australia.
Code availability
Not applicable.
References
World Health Organization. (2011). Global Health and Aging. Retrieved 9 September, 2019, from https://www.who.int/ageing/publications/global_health.pdf.
World Health Organization. (2020). Aging and Health. Retrieved 5 January, 2020, from https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
Salomon, J. A., Wang, H., Freeman, M. K., Vos, T., Flaxman, A. D., Lopez, A. D., et al. (2012). Healthy life expectancy for 187 countries, 1990–2010: A systematic analysis for the Global Burden Disease Study 2010. The Lancet, 380(9859), 2144–2162.
Gandek, B., Ware, J. E., Aaronson, N. K., Apolone, G., Bjorner, J. B., Brazier, J. E., et al. (1998). Cross-validation of item selection and scoring for the SF-12 Health Survey In Nine Countries: Results from the IQOLA project. Journal of Clinical Epidemiology, 51(11), 1171–1178.
Ferrans, C. E. (2005). Definitions and conceptual models quality of life. In J. Lipscomb, C. C. Gotay, & C. Snyder (Eds.), Outcomes assessment in cancer: Measures, methods, and applications (pp. 14–30). Cambridge: Cambridge University Press.
Karimi, M., & Brazier, J. (2016). Health, health-related quality of life, and quality of life: What is the difference? PharmacoEconomics, 34(7), 645–649.
Gill, T. M., & Feinstein, A. R. (1994). A critical appraisal of the quality of quality-of-life measurements. JAMA, 272(8), 619–626.
Mehanna, H. M., & Morton, R. P. (2006). Does quality of life predict long-term survival in patients with head and neck cancer? Archives of Otolaryngology: Head & Neck Surgery, 132(1), 27–31.
Rodríguez-Artalejo, F., Guallar-Castillón, P., Pascual, C. R., Otero, C. M., Montes, A. O., García, A. N., et al. (2005). Health-related quality of life as a predictor of hospital readmission and death among patients with heart failure. Archives of Internal Medicine, 165(11), 1274–1279.
Phyo, A. Z. Z., Freak-Poli, R., Craig, H., Gasevic, D., Stocks, N., Gonzalez-Chica, D. A., et al. (2020). Quality of Life and mortality in the general population: A systematic review and meta-analysis. BMC Public Health, 20, 1596.
Nilsson, E., Festin, K., Lowén, M., & Kristenson, M. (2019). SF-36 predicts 13-year CHD incidence in a middle-aged Swedish general population. Quality of Life Research, 29(4), 971–975.
Vlassoff, C. (2007). Gender differences in determinants and consequences of health and illness. Journal of Health, Population, and Nutrition, 25(1), 47.
World Health Organization. (2019). Global Health Observatory (GHO) data: World Health Statistics 2019: Monitoring health for the SDGs. Retrieved 28 January, 2020, from https://www.who.int/gho/publications/world_health_statistics/2019/en/.
Cherepanov, D., Palta, M., Fryback, D. G., & Robert, S. A. (2010). Gender differences in health-related quality-of-life are partly explained by sociodemographic and socioeconomic variation between adult men and women in the US: Evidence from four US nationally representative data sets. Quality of Life Research, 19(8), 1115–1124.
Grimm, R., Mcneil, J. J., Applegate, W., Beilin, L., Espinoza, S., Johnston, C. I., et al. (2013). Study design of ASPirin in reducing events in the elderly (ASPREE): A randomized, controlled trial. Contemporary Clinical Trials, 36(2), 555–564.
Index Mundi - Country Facts. (2020). United States vs. Australia. Retrieved October 2020, from https://www.indexmundi.com/factbook/compare/united-states.australia.
Mcneil, J. J., Woods, R. L., Nelson, M. R., Murray, A. M., Reid, C. M., Kirpach, B., et al. (2017). Baseline characteristics of participants in the ASPREE (ASPirin in reducing events in the elderly) study. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 72(11), 1586–1593.
Ware, J. E., Jr., Kosinski, M., & Keller, S. D. (1996). A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
Ware, J. E., Jr., Kosinski, M., Turner-Bowker, D. M., & Gandek, B. (2002). User’s manual for the SF-12v2® health survey with a supplement documenting SF-12® health survey). Lincoln, RI: QualityMetric Incorporated.
Mcneil, J. J., Nelson, M. R., Woods, R. L., Lockery, J. E., Wolfe, R., Reid, C. M., et al. (2018). Effect of aspirin on all-cause mortality in the healthy elderly. The New England Journal of Medicine, 379(16), 1519–1528.
Ryerson Index Inc. The Ryerson Index home page. Retrieved 11 November, 2019, from http://www.ryersonindex.org/.
Idler, E., & Amini, Y. (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38(1), 21–37.
Stocks, N., González-Chica, D., Woods, R., Lockery, J., Wolfe, R., Murray, A., et al. (2019). Quality of Life for 19,114 participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study and their association with sociodemographic and modifiable lifestyle risk factors. Quality of Life Research, 28(4), 935–946.
World Health Organization. (2000). Obesity: Preventing and managing the global epidemic. Report of a WHO Consultation on Obesity. Retrieved 20 February, 2020, from https://www.who.int/gho/ncd/risk_factors/bmi_text/en/.
Hawthorne, G., Osborne, R., Taylor, A., & Sansoni, J. (2007). The SF36 Version 2: Critical analyses of population weights, scoring algorithms and population norms. An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 16(4), 661–673.
Mancuso, S. (2017). SF-12 v2 Scoring using Australian Population Weights (Sam Mancuso in Scoring Algorithm, Self-Report Measures). Retrieved 5 October, 2020, from https://sammancuso.com/2017/11/08/sf-12-v2-scoring-using-australia-population-weights/.
Mancuso, S. Personal communication with Rosanne Freak-Poli and Aung Zaw Zaw Phyo. 29th September 2020 to 4th October 2020.
Brazier, E. J., & Roberts, E. J. (2004). The estimation of a preference-based measure of health from the SF-12. Medical Care, 42(9), 851–859.
Haring, R., Feng, Y.-S., Moock, J., Völzke, H., Dörr, M., Nauck, M., et al. (2011). Self-perceived quality of life predicts mortality risk better than a multi-biomarker panel, but the combination of both does best. BMC Medical Research Methodology, 11(1), 103.
Munoz, M. A., Subirana, I., Elosua, R., Covas, M. I., Baena-Diez, J. M., Ramos, R., et al. (2011). Utility of a short quality of life questionnaire to predict cardiovascular events. International Journal of Cardiology, 151(3), 392–394.
Ul-Haq, Z., Mackay, D. F., & Pell, J. P. (2014). Association between physical and mental health-related quality of life and adverse outcomes: A retrospective cohort study of 5,272 Scottish adults. BMC Public Health, 14, 1197.
Dorr, D. A., Jones, S. S., Burns, L., Donnelly, S. M., Brunker, C. P., Wilcox, A., et al. (2006). Use of health-related, quality-of-life metrics to predict mortality and hospitalizations in community-dwelling seniors. Journal of the American Geriatrics Society, 54(4), 667–673.
Fan, V. S., Au, D. H., Mcdonell, M. B., & Fihn, S. D. (2004). Intraindividual change in SF-36 in ambulatory clinic primary care patients predicted mortality and hospitalizations. Journal of Clinical Epidemiology, 57(3), 277–283.
Singh, J. A., Borowsky, S. J., Nugent, S., Murdoch, M., Zhao, Y., Nelson, D. B., et al. (2005). Health-related quality of life, functional impairment, and healthcare utilization by veterans: Veterans’ quality of life study. Journal of the American Geriatrics Society, 53(1), 108–113.
Myint, P. K., Luben, R. N., Surtees, P. G., Wainwright, N. W. J., Welch, A. A., Bingham, S. A., et al. (2007). Self-reported mental health-related quality of life and mortality in men and women in the European Prospective Investigation into Cancer (EPIC-Norfolk): A prospective population study. Psychosomatic Medicine, 69(5), 410–414.
Tsai, S. Y., Chi, L. Y., Lee, C. H., & Chou, P. (2007). Health-related quality of life as a predictor of mortality among community-dwelling older persons. European Journal of Epidemiology, 22(1), 19–26.
Leigh, L., Hudson, I. L., & Byles, J. E. (2015). Sleeping difficulty, disease and mortality in older women: A latent class analysis and distal survival analysis. Journal of Sleep Research, 24(6), 648–657.
Williams, E. D., Rawal, L., Oldenburg, B. F., Renwick, C., Shaw, J. E., & Tapp, R. J. (2012). Risk of cardiovascular and all-cause mortality: Impact of impaired health-related functioning and diabetes—The Australian Diabetes, Obesity and Lifestyle (AusDiab) study. Diabetes Care, 35(5), 1067–1073.
Otero-Rodriguez, A., Leon-Munoz, L. M., Balboa-Castillo, T., Banegas, J. R., Rodriguez-Artalejo, F., & Guallar-Castillon, P. (2010). Change in health-related quality of life as a predictor of mortality in the older adults. Quality of Life Research, 19(1), 15–23.
Govindaraju, T., Sahle, B. W., Mccaffrey, T. A., Mcneil, J. J., & Owen, A. J. (2018). Dietary patterns and quality of life in older adults: A systematic review. Nutrients. https://doi.org/10.3390/nu10080971.
Afshin, A., Sur, P. J., Fay, K. A., Cornaby, L., Ferrara, G., Salama, J. S., et al. (2019). Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 393(10184), 1958–1972.
Austad, S. N., & Fischer, K. E. (2016). Sex differences in lifespan. Cell Metabolism, 23(6), 1022–1033.
Williams, K., Sansoni, J., Morris, D., Grootemaat, P., & Thompson, C. (2016). Patient-reported outcome measures: Literature review. Sydney: Australian Commission on Safety and Quality in Health Care (ACSQHC).
Acknowledgements
We would like to thank the ASPREE participants who volunteered for this study, the general practitioners and staff of the medical clinics who support the study participants, and the trial staff and management team of the ASPREE study in Australia and the United States, and the ASPREE Investigator Group listed on www.aspree.org.
Funding
The ASPREE (ASPirin in Reducing Events in the Elderly) trial was mainly supported by grants from the National Institute on Aging and the National Cancer Institute at the National Institutes of Health (Grant Number U01AG029824); the National Health and Medical Research Council of Australia (Grant Numbers 334047 and 1127060); Monash University (Australia) and the Victorian Cancer Agency (Australia). Other funding resources and collaborating organizations of the ASPREE study are listed on http://www.aspree.org. AZZP is supported by Monash International Tuition Scholarship (Medicine, Nursing, and Health Sciences) and Monash Graduate Scholarship (30072360). RFP is supported by a National Heart Foundation of Australia Postdoctoral Fellowship (101927). JR and CMR are supported by a National Health and Medical Research Council Dementia Research Leader Fellowship (APP 1135727) and Principal Research Fellowship (APP1136372) respectively. Funders had no role in the design and conduct of the study, in the collection, analysis, and interpretation of data and in the writing, review and submission of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
AMM, RLW, CMR, and MRN designed and conceptualized the ASPREE study. CMR designed process associated with acquisition of ASPREE data. NPS provided major role in the health-related quality of life component of ASPREE study. RLW provided major roles in the acquisition of ASPREE data. RF-P conceived the current study. RF-P, JR, and AZZP designed the current study. AZZP had full access to all the data in the study and analysed the data. AZZP, RF-P, and JR interpreted the data, with input from DAG-C, NPS and DG. AZZP wrote the initial manuscript draft and undertook revisions. All authors provided critical comments and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
ASPREE (ASPirin in Reducing Events in the Elderly) trial is being conducted in accordance with the Declaration of Helsinki 1964 as revised in 2008, the NHMRC Guidelines on Human Experimentation, the federal patient privacy (HIPAA) law and ICH-GCP guidelines and the International Conference of Harmonization Guidelines for Good Clinical Practice. ASPREE also follows the Code of Federal Regulations as it relates to areas of clinical research. The overall management and conduct of the ASPREE clinical trial is the responsibility of the ASPREE Steering Committee. The data of the present secondary data-analysis study was from a five-year ASPREE clinical trial (Trial Registration: International Standard Randomized Controlled Trial Number Register (ISRCTN 83772183) and clinicaltrials.gov (NCT 01038583)). The current secondary data analysis has been approved by the Monash University Human Research Ethics Committee (project ID: 21714). The ASPREE trial has been approved by multiple Institutional Review Boards in Australia and the U.S. (www.aspree.org).
Consent to participate
This study used data from a five-year ASPREE (ASPirin in Reducing Events in the Elderly) clinical trial (Trial Registration: International Standard Randomized Controlled Trial Number Register (ISRCTN 83772183) and clinicaltrials.gov (NCT 01038583)). All individual participants of ASPREE clinical trial signed informed consent on participation.
Consent for publication
All authors gave their approval for submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
ASPREE Investigator Group listed on www.aspree.org.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Phyo, A.Z.Z., Ryan, J., Gonzalez-Chica, D.A. et al. Health-related quality of life and all-cause mortality among older healthy individuals in Australia and the United States: a prospective cohort study. Qual Life Res 30, 1037–1048 (2021). https://doi.org/10.1007/s11136-020-02723-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02723-y