Abstract
Purpose
The purpose of the study was to investigate the trajectory and determinants of changes in health-related quality of life (HRQoL) in the first year after lumbar spine surgery.
Methods
A total of 154 consecutive patients who underwent lumbar spine surgery were included in this prospective longitudinal observational study. All participants were asked to complete a battery of questionnaires (Taiwanese version of World Health Organization Quality of Life-BREF, Numerical Rating Scale for leg and back pain, Mandarin Chinese version of the Clinically Useful Depression Outcome Scale, and Chinese version of the Pittsburgh Sleep Quality Index). The Japanese Orthopedic Association score was evaluated by neurosurgeons. The measurement time points were 1 week before and on the first, sixth, and twelfth month after lumbar spinal surgery. A linear mix model was used for data analyses.
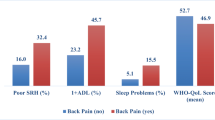
Results
The analyses revealed significant upward trends in HRQoL, particularly in physical health and social relationships during the study period. Patients who aged < 65 years and reported a higher level of functional status experienced a more favorable HRQoL in physical health over time (p = .002 and .02, respectively). Participants who complained of poor sleep quality yielded poorer HRQoL in physical health over time (p = .03). More severe depressive symptom was associated with the poorer HRQoL in social relationships over time (p < .001).
Conclusions
To improve the HRQoL, healthcare providers need to pay attention to changes in sleep quality, neurological functions, and depressive symptoms in people receiving lumbar surgery, particularly individuals with increasing age. Concrete interventions and strategies aimed to enhancing HRQoL in these patients are essential.

Similar content being viewed by others
References
Tian, W., Lv, Y., Liu, Y., Xiao, B., & Han, X. (2014). The high prevalence of symptomatic degenerative lumbar osteoarthritis in Chinese adults: A population-based study. Spine (Phila Pa 1976), 39(16), 1301–1310.
Yoshimura, N., Dennison, E., Wilman, C., Hashimoto, T., & Cooper, C. (2000). Epidemiology of chronic disc degeneration and osteoarthritis of the lumbar spine in Britain and Japan: A comparative study. Journal of Rheumatology, 27(2), 429–433.
Katz, J. N. (2006). Lumbar disc disorders and low-back pain: Socioeconomic factors and consequences. Journal of Bone and Joint Surgry, 88(Suppl 2), 21–24.
Sinikallio, S., Aalto, T., Airaksinen, O., Herno, A., Kroger, H., Savolainen, S.et al (2006). Depression and associated factors in patients with lumbar spinal stenosis. Disability and Rehabilitation, 28(7), 415–422.
Parker, S. L., Godil, S. S., Mendenhall, S. K., Zuckerman, S. L., Shau, D. N., & McGirt, M. J. (2014). Two-year comprehensive medical management of degenerative lumbar spine disease (lumbar spondylolisthesis, stenosis, or disc herniation): A value analysis of cost, pain, disability, and quality of life: Clinical article. Journal of Neurosurgery: Spine, 21(2), 143–149. https://doi.org/10.3171/2014.3.SPINE1320.
Whittle, I. R., Scotland, J., Dengu, F., Anpalakhan, S., & Deary, I. J. (2012). Preoperative quality of life in patients with degenerative spinal disorders: Many are worse than patients with brain tumours and cancer. British Journal of Neurosurgery, 26(4), 460–465. https://doi.org/10.3109/02688697.2011.641618.
Hakkinen, A., Kautiainen, H., Sintonen, H., & Ylinen, J. (2005). Health related quality of life after lumbar disc surgery: A prospective study of 145 patients. Disability and Rehabilitation, 27(3), 94–100.
Azimi, P. (2013). Quality of life in patients before and after surgery for a lumbar spinal stenosis. Journal of Research in Medical Sciences. Retrieved May 14, 2018 from http://jrms.mui.ac.ir/index.php/jrms/article/view/9744.
Jansson, K. A., Nemeth, G., Granath, F., Jonsson, B., & Blomqvist, P. (2005). Health-related quality of life in patients before and after surgery for a herniated lumbar disc. Journal of Bone and Joint Surgery, 87(7), 959–964.
Jansson, K. A., Nemeth, G., Granath, F., Jonsson, B., & Blomqvist, P. (2009). Health-related quality of life (EQ-5D) before and one year after surgery for lumbar spinal stenosis. Journal of Bone and Joint Surgry, 91(2), 210–216. https://doi.org/10.1302/0301-620X.91B2.21119.
Silverplats, K., Lind, B., Zoega, B., Halldin, K., Gellerstedt, M., Rutberg, L., et al. (2011). Health-related quality of life in patients with surgically treated lumbar disc herniation: 2- and 7-year follow-up of 117 patients. Acta Orthopaedica, 82(2), 198–203. https://doi.org/10.3109/17453674.2011.566136.
Kagaya, H., Takahashi, H., Sugawara, K., Kuroda, T., & Takahama, M. (2005). Quality of life assessment before and after lumbar disc surgery. Journal of Orthopaedic Science, 10(5), 486–489.
Ma, Y., Mazumdar, M., & Memtsoudis, S. G. (2012). Beyond repeated-measures analysis of variance: Advanced statistical methods for the analysis of longitudinal data in anesthesia research. Regional Anesthesia and Pain Medicine, 37(1), 99–105. https://doi.org/10.1097/AAP.0b013e31823ebc74.
Heider, D., Kitze, K., Zieger, M., Riedel-Heller, S. G., & Angermeyer, M. C. (2007). Health-related quality of life in patients after lumbar disc surgery: A longitudinal observational study. Quality of Life Research, 16(9), 1453–1460.
Robinson, Y., Michaelsson, K., & Sanden, B. (2013). Instrumentation in lumbar fusion improves back pain but not quality of life 2 years after surgery. A study of 1,310 patients with degenerative disc disease from the Swedish Spine Register SWESPINE. Acta Orthopaedic, 84(1), 7–11. https://doi.org/10.3109/17453674.2013.771300.
Juricek, M., Rehak, L., Horvath, J., & Tisovsky, P. (2010). Quality of life after elective lumbar spinal fusions. Bratislavske Lekarske Listy, 111(5), 290–295.
Miller, J. A., Derakhshan, A., Lubelski, D., Alvin, M. D., McGirt, M. J., Benzel, E. C., et al. (2015). The impact of preoperative depression on quality of life outcomes after lumbar surgery. Spine Journal, 15(1), 58–64. https://doi.org/10.1016/j.spinee.2014.06.020.
Slover, J., Abdu, W. A., Hanscom, B., & Weinstein, J. N. (2006). The impact of comorbidities on the change in short-form 36 and oswestry scores following lumbar spine surgery. Spine (Phila Pa 1976), 31(17), 1974–1980.
Sezgin, M., Hasanefendioglu, E. Z., Ali Sungur, M., Incel, N. A., Cimen, O., Kanik, A., et al. (2014). Sleep quality in patients with chronic low back pain: A cross-sectional study assesing its relations with pain, functional status and quality of life. Journal of Back and Musculoskeletal Rehabilitation, 28(3), 433–411. https://doi.org/10.3233/BMR-140537.
Solberg, T. K., Nygaard, O. P., Sjaavik, K., Hofoss, D., & Ingebrigtsen, T. (2005). The risk of “getting worse” after lumbar microdiscectomy. European Spine Journal, 14(1), 49–54.
Hedeker, D., Gibbons, R. D., & Waternaux, C. (1999). Sample size estimation for longitudinal designs with attrition: Comparing time-related contrasts between two groups. Journal of Educational and Behavioral Statistics, 24, 70–93.
The WHOQOL Taiwan Group. (2005). Manual of the Taiwanese version of WHOQOL-BREF. Taipei Taiwan: Taiwan WHOQOL Group.
Yao, G., Chung, C. W., Yu, C. F., & Wang, J. D. (2002). Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. Journal of Formosan Medical Association, 101(5), 342–351.
Bentsen, S. B., Wahl, A. K., Strand, L. I., & Hanestad, B. R. (2007). Relationships between demographic, clinical and pain variables and health-related quality of life in patients with chronic low back pain treated with instrumented fusion. Scandinavian Journal of Caring Science, 21(1), 134–143.
Saban, K. L., Penckofer, S. M., Androwich, I., & Bryant, F. B. (2007). Health-related quality of life of patients following selected types of lumbar spinal surgery: A pilot study. Health and Quality of Life Outcomes, 5, 71. https://doi.org/10.1186/1477-7525-5-71.
Charlson, M. E., Pompei, P., Ales, K. L., & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383.
Deyo, R. A., Cherkin, D. C., & Ciol, M. A. (1992). Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology, 45(6), 613–619.
Romano, P. S., Roost, L. L., & Jollis, J. G. (1993). Presentation adapting a clinical comorbidity index for use with ICD-9-CM administrative data: Differing perspectives. Journal of Clinical Epidemiology, 46(10), 1075–1079.
Schneeweiss, S., Wang, P. S., Avorn, J., & Glynn, R. J. (2003). Improved comorbidity adjustment for predicting mortality in Medicare populations. Health Service Research, 38(4), 1103–1120.
Ondeck, N. T., Bohl, D. D., Bovonratwet, P., McLynn, R. P., Cui, J. J., Shultz, B. N., et al. (2018). Discriminative ability of commonly used indices to predict adverse outcomes after poster lumbar fusion: A comparison of demographics, ASA, the modified Charlson Comorbidity Index, and the modified Frailty Index. Spine, 18(1), 44–52. https://doi.org/10.1016/j.spinee.2017.05.028.
Bijur, P. E., Latimer, C. T., & Gallagher, E. J. (2003). Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Academic Emergency Medicine, 10(4), 390–392.
Taylor, L. J., & Herr, K. (2003). Pain intensity assessment: A comparison of selected pain intensity scales for use in cognitively intact and cognitively impaired African American older adults. Pain Management Nursing, 4(2), 87–95.
Hsu, L. F., Kao, C. C., Wang, M. Y., Chang, C. J., & Tsai, P. S. (2014). Psychometric testing of a Mandarin Chinese Version of the Clinically Useful Depression Outcome Scale for patients diagnosed with type 2 diabetes mellitus. International Journal of Nursing Studies, 51(12), 1595–1604. https://doi.org/10.1016/j.ijnurstu.2014.05.004.
Buysse, D. J., Reynolds, C. F. 3rd, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213.
Tsai, P. S., Wang, S. Y., Wang, M. Y., Su, C. T., Yang, T. T., Huang, C. J., et al. (2005). Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Quality of Life Research, 14(8), 1943–1952.
Osawa, T., Ogura, T., Hayashida, T., Mori, M., & Hase, H. (2003). Evaluation of lumbosacral nerve root lesions using evoked potentials recorded by a surface electrode technique. Spine (Phila Pa 1976), 28(5), 496–501.
West, B. T., Welch, K. B., & Galecki, A. T. (2007). Linear mixed models: A practical guide using statistical software. FL, Chapman Hall: CRC Press.
Dammers, R., & Koehler, P. J. (2002). Lumbar disc herniation: Level increases with age. Surgical Neurology, 58(3–4), 209–212 (discussion 212–203).
Otani, K., Kikuchi, S., Yabuki, S., Igarashi, T., Nikaido, T., Watanabe, K., & Konno, S. (2013). Lumbar spinal stenosis has a negative impact on quality of life compared with other comorbidities: An Epidemiological Cross-Sectional Study of 1862 community-dwelling individuals. Scientific World Journal, 2013, 590652.
Marty, M., Rozenberg, S., Duplan, B., Thomas, P., Duquesnoy, B., Allaert, F., & The Section Rachis de la Société Française de Rhumatologie. (2008). Quality of sleep in patients with chronic low back pain: A case-control study. European Spine Journal, 17(6), 839–844.
Luca, G., Haba Rubio, J., Andries, D., Tobback, N., Vollenweider, P., Waeber, G., Vidal, P. M., Preisig, M., Heinzer, R., & Tafti, M. (2015). Age and gender variations of sleep in subjects without sleep disorders. Annals of Medicine, 47(6), 482–491. https://doi.org/10.3109/07853890.2015.1074271.
Wang, H. Y., Fu, T. S., Hsu, S. C., & Hung, C. I. (2016). Association of depression with sleep quality might be greater than that of pain intensity among outpatients with chronic low back pain. Neuropsychiatric Disease and Treatment, 12, 1993–1998. https://doi.org/10.2147/NDT.S110162.
Sezgin, M., Hasanefendioglu, E. Z., Sungur, M. A., Incel, N. A., Cimen, O. B., Kanik, A., et al. (2015). Sleep quality in patients with chronic low back pain: A cross-sectional study assesing its relations with pain, functional status and quality of life. Journal of Back and Musculoskeletal Rehabilitation, 28(3), 433–441. https://doi.org/10.3233/BMR-140537.
Auvinen, J. P., Tammelin, T. H., Taimela, S. P., Zitting, P. J., Jarvelin, M. R., Taanila, A. M., et al. (2010). Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. European Spine Journal, 19(4), 641–649. https://doi.org/10.1007/s00586-009-1215-2.
Kovacs, F. M., Abraira, V., Zamora, J., Teresa Gil del Real, M., Llobera, J., Fernandez, C., et al. (2004). Correlation between pain, disability, and quality of life in patients with common low back pain. Spine (Phila Pa 1976), 29(2), 206–210.
Gu, Y., Shi, J., Cao, P., Yuan, W., Wu, H., Yang, L.et al (2015). Clinical and imaging predictors of surgical outcome in multilevel cervical ossification of posterior longitudinal ligament: An analysis of 184 patients. PLoS ONE, 10(9), e0136042. https://doi.org/10.1371/journal.pone.0136042.
Chang, Y.-C., Yao, G., Hu, S. C., & Wang, J.-D. (2015). Depression affects the scores of all facets of the WHOQOL-BREF and may mediate the effects of physical disability among community-dwelling older adults. PLoS ONE, 10(5), e0128356. https://doi.org/10.1371/journal.pone.0128356.
Cao, W., Guo, C., Ping, W., Tan, Z., Guo, Y., & Zheng, J. (2016). A community-based study of quality of life and depression among older adults. International Journal of Environmental Research and Public Health, 13(7), 693. https://doi.org/10.3390/ijerph13070693.
Steger, M. F., & Kashdan, T. B. (2009). Depression and everyday social activity, belonging, and well-being. Journal of Counseling Psychology, 56(2), 289–300.
Fried, E. I., & Nesse, R. M. (2014). The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS ONE, 9(2), e90311. https://doi.org/10.1371/journal.pone.0090311.
Funding
This study was supported by Grants to H.Y. Chiu by the Taipei Medical University-Taipei Medical University Hospital (104TMU-TMUH-15) and the Ministry of Science and Technology, Taiwan (MOST 106-2314-B-038 -058 -MY3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no potential conflict of interest regarding the authorship and publication of this study and have no financial disclosures to report.
Rights and permissions
About this article
Cite this article
Lin, EY., Chen, PY., Tsai, PS. et al. Trajectory of health-related quality of life and its determinants in patients who underwent lumbar spine surgery: a 1-year longitudinal study. Qual Life Res 27, 2251–2259 (2018). https://doi.org/10.1007/s11136-018-1888-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1888-2