Abstract
Purpose
To analyze the clinical characteristics of acromegalic patients with empty sella (ES, herniation of the subarachnoid space within the sella turcica) and the impact of ES on transsphenoidal surgery in such patients.
Methods
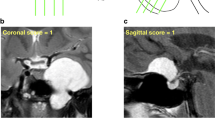
Seventy-eight patients, newly diagnosed with acromegaly who underwent transsphenoidal surgery were included. ES was defined as the pituitary gland and adenoma occupying less than 50% of the sella turcica on midsagittal magnetic resonance (MR) imaging.
Results
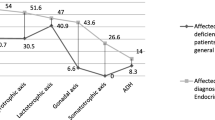
Twelve patients (15.4%), predominantly female (10 women, p = .047), had ES in preoperative MR imaging. ES patients had smaller mean tumor diameter (6.3 mm) than non-ES patients (11.2 mm, p = .001). In preoperative MR imaging, occult adenoma was found in three (25%) ES and three (4.5%) non-ES patients (p = .044). Intraoperative cerebrospinal fluid (CSF) leakage was more frequent in the ES patients than in the non-ES patients (58.3 vs. 25.8%, p = .024). This led to an increased rate of sellar floor reconstruction using abdominal fat and/or postoperative lumber drainage in the ES patients (ES: 41.7 vs. non-ES: 16.7%, p = .063). Endocrinological remission after surgery was more frequent in the non-ES patients (72.7%) than in the ES patients (58.3%) (p = .248).
Conclusions
Co-existence of acromegaly with ES is not rare, and is associated with occult adenoma, intra/postoperative CSF leakage, and a worse endocrinological outcome after transsphenoidal surgery; although, the underlying mechanism remains unclear.


Similar content being viewed by others
References
De Marinis L, Bonadonna S, Bianchi A, Maira G, Giustina A (2005) Primary empty sella. J Clin Endocrinol Metab 90:5471–5277
Yücesoy K, Yüceer N, Göktay Y (2000) Empty sella syndrome following pituitary apoplexy. Acta Neurochir. 142:355–356 (Wien)
Guitelman M, Garcia, Basavilbaso, N., Vitale M, Chervin A, Katz D, Miragaya K, Herrera J, Cornalo D, Servidio M, Boero L, Manavela M, Danilowicz K, Alfieri A, Stalldecker G, Glerean M, Day P, Ballarino C, Gil MS, Rogozinski A (2013) Primary empty sella (PES): a review of 175 cases. Pituitary 16:270–274
Bergland RM, Ray BS, Torack RM (1968) Anatomical variations in the pituitary gland and adjacent structures in 225 human autopsy cases. J Neurosurg 28:93–99
Coulson CJ, Siddiq MA, Johnson AP (2007) Empty sella syndrome associated with a hyperfunctioning microadenoma invading the clivus. Br J Neurosurg 21:623–625
Iwai Y, Yamanaka K, Yoshioka K, Kanai M (2004) Gamma knife radiosurgery for GH-secreting microadenoma with empty sella. J Clin Neurosci 11:418–421
Agrawal NK, Jain P, Garg S (2012) Primary empty sella with isolated ACTH deficiency and microprolactinoma. Gynecol Endocrinol 28:568–569
Manavela MP, Goodall CM, Katz SB, Moncet D, Bruno OD (2001) The association of Cushing’s disease and primary empty sella turcica. Pituitary 4:145–151
Mehta GU, Bakhtian KD (2014) Oldfield EH. Effect of primary empty sella syndrome on pituitary surgery for Cushing’s disease. J Neurosurg 121:518–526
Liu W, Zhou H, Neidert MC, Schmid C, Bernays RL, Ni M, Zhou D, Jia W, Jia G (2014) Growth hormone secreting pituitary microadenomas and empty sella-An under-recognized association? Clin Neurol Neurosurg 126:18–23
Giustina A, Barkan A, Casanueva FF, Cavagnini F, Frohman L, Ho K, Veldhuis J, Wass J, Von, Werder, K., Melmed S (2000) Criteria for cure of acromegaly: a consensus statement. J Clin Endocrinol Metab 85:526–529
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:610–618
Zada G, Lin N, Laws ER Jr (2010) Patterns of extrasellar extension in growth hormone-secreting and nonfunctional pituitary macroadenomas. Neurosurg Focus 29:E4
Lee JY, Bohman LE, Bergsneider M (2014) Contemporary neurosurgical techniques for pituitary tumor resection. J Neurooncol 117:437–444
Esposito F, Dusick JR, Fatemi N, Kelly DF (2007) Graded repair of cranial base defects and cerebrospinal fluid leaks in transsphenoidal surgery. Neurosurgery 60 (4 Suppl 2):295–303 discussion 303–304
Yoshino A, Katayama Y, Watanabe T, Hirota H (2005) Vanishing pituitary mass revealed by timely magnetic resonance imaging: examples of spontaneous resolution of nonfunctioning pituitary adenoma. Acta Neurochir. 147:253–257 (Wien) discussion 257
Potorac I, Petrossians P, Daly AF, Schillo F, Slama BC, Nagi S, Sahnoun M, Brue T, Girard N, Chanson P, Nasser G, Caron P, Bonneville F, Raverot G, Lapras V, Cotton F, Delemer B, Higel B, Boulin A, Gaillard S, Luca F, Goichot B, Dietemann JL, Beckers A, Bonneville JF (2015) Pituitary MRI characteristics in 297 acromegaly patients based on T2-weighted sequences. Endocr Relat Cancer 22:169–177
Kinoshita M, Tanaka H, Arita H, Goto Y, Oshino S, Watanabe Y, Yoshimine T, Saitoh Y (2015) Pituitary-targeted dynamic contrast-enhanced multisection CT for detecting MR imaging-occult functional pituitary microadenoma. AJNR. 36:904–908
Mehta GU, Oldfield EH (2012) Prevention of intraoperative cerebrospinal fluid leaks by lumbar cerebrospinal fluid drainage during surgery for pituitary macroadenomas: Clinical article. J Neurosurg 116:1299–1303
Funding
No specific funding was provided for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sasagawa, Y., Hayashi, Y., Tachibana, O. et al. Clinical characteristics of acromegalic patients with empty sella and their outcomes following transsphenoidal surgery. Pituitary 20, 403–408 (2017). https://doi.org/10.1007/s11102-017-0798-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-017-0798-6