Abstract
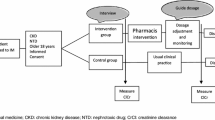
Background In France, community pharmacists do not have free access to patients’ lab results, and it is therefore impossible for them to identify patients with renal impairment. Objective (1) to evaluate the ability of community pharmacists (CPs) to identify drug related problems (DRP) in patients at risk for or suffering from renal impairment; (2) to evaluate the proportions of recommendations by CPs that lead to a modification by GP. Setting A prospective and observational study involving 24 community pharmacists in France. Methods Following special training, community pharmacists were asked to select 52 patients with the following characteristics: ≥65 years of age; prescribed at least two diabetic and/or antihypertensive drugs. Serum creatinine value was obtained for each patient and glomerular filtration rate estimated (eGFR) with the aMDRD formula. Those with a eGFR 60 ml/min/1.73 m² were considered having chronic kidney disease (CKD). Data was collected concerning whether the community pharmacists identified drug related problems and tried to inform the GP who prescribed the medications. Identified DRP were reviewed by a team of nephrologists and hospital clinical pharmacists. Primary outcome The proportion of CKD patients and those without serum creatinine monitoring, the number of drug related problems identified by community pharmacists, and the proportion of drug related problems resolved by the community pharmacists intervention to the GP. Results Of the total 791 patients identified, 180 (22.8 %) exhibited CKD, and 57 (7.2 %) had not undergone serum creatinine monitoring. Among the 1297 drugs prescribed, 260 had to be adapted to eGFR. The proportion of DRP was 21.5 % (56/260), of which 40 % (20) were identified by community pharmacists. Once the GP was informed, 33.3 % (6/18) of DRP were resolved. Conclusion Community pharmacists identified 40 % of DRP related to CKD prescriptions, leading to prescription modification by GPs in a third of the cases. These interventions are likely to decrease drug-related morbidity and mortality.

Similar content being viewed by others
References
HAS December 2011. Evaluation du débit de filtration glomérulaire et du dosage de la créatininémie dans le diagnostic de la maladie rénale chronique chez l’adulte [Glomerular filtration rate evaluation and serum creatinine in the diagnosis of chronic kidney disease in adults]. ISBN: 978-2-11-128508-8. http://www.has-sante.fr/portail/upload/docs/application/pdf/2011-12/rapport_dfg_creatininemie.pdf. Accessed 14 Feb 2014.
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–47.
HAS février 2012 guide du parcours de soins. Maladie Rénale Chronique de l’adulte [Internet]. ISBN: 978-11-128521-7. http://www.has-sante.fr/portail/upload/docs/application/pdf/2012-4/guide_parcours_de_soins_mrc_web.pdf. Accessed 14 Feb 2014.
Cogneau J, Blanchecotte F, Halimi J. BIRD: base de données sur la fonction rénale en région Centre [BIRD: database on renal function in the Centre Region]. Ann Biol Clin. 2008;66(3):285–90.
Stengel B, Couchoud C, Helmer C, Loos-Ayav C. Épidémiologie de l’insuffisance rénale chronique en France [Epidemiology of chronic renal failure in France]. Presse Med. 2007;36(12):1811–21.
Bouattar T, Benasila S, Mattous M, Ezzaitouni F, Ouzeddoun N, Rhou H, et al. L’atteinte rénale chez le diabétique âgé [Renal disease in elderly diabetic]. NPG. 2010;10(55):43–9.
Verbeeck RK, Musuamba FT. Pharmacokinetics and dosage adjustment in patients with renal dysfunction. Eur J Clin Pharmacol. 2009;65(8):757–73.
Long CL, Raebel MA, Price DW, Magid DJ. Compliance with dosing guidelines in patients with chronic kidney disease. Ann Pharmacother. 2004;38(5):853–8.
Pourrat X, Sipert AS, Sautenet B, Merieau E, Grassin J, Halimi JM. Drugs adjustment dosage at hospital discharge for patients with renal failure: study of 326 medical records. Presse Med. 2012;41(4):e189–94.
Nash Kevin, Hafeez Abdul, Hou Susan. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39(5):930–6.
Rapport de l’Académie nationale de Pharmacie: Bonnes pratiques de dispensation du médicament par le pharmacien d’officine [Report of the National Academy of Pharmacy: Good practices for drug dispensing by the pharmacist]. http://www.acadpharm.org/dos_public/Rapport_Bonnes_pratiques_de_dispensation__adoptEpar_le_Conseil_du_27_11_2013_VF.pdf. Accessed 22 Feb 2015.
Leape LL, Cullen DJ, Clapp MD, Burdick E, Demonaco HJ, Erickson JI, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282(3):267–70.
Hassan Y, Al-Ramahi RJ, Aziz NA, Ghazali R. Impact of a renal drug dosing service on dose adjustment in hospitalized patients with chronic kidney disease. Ann Pharmacother. 2009;43(10):1598–605.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–70.
National Kidney Foundation. Guidelines and commentaries. https://www.kidney.org/professionals/guidelines/guidelines_commentaries. Accessed 07 Jul 2015.
Prat L, Caille A, Sautenet B, Merieau E, Leger J, Giraudeau B, et al. L’insuffisance rénale en milieu hospitalier: est-ce fréquent? Est-ce grave? Chez qui? Etude Néphrovigilance [Renal failure in hospital: is it common? Is it serious? For whom? Nephrovigilance study]. Soc Néphrol Brux Ther. 2010;5(6):462–468.
Blicklé JF, Doucet J, Krummel T, Hannedouche T. Diabetic nephropathy in the elderly. Diabetes Metab. 2007;33:S40–55.
Pozuelos Estrada G, Molina Martínez L, Romero Perera JJ, Díaz Herrera N, Cañón Barroso L, Buitrago Ramírez F. Prevalence of hidden renal failure calculated through formulas on the degree of renal function in hypertense patients over 60 referred to out-patients for blood pressure monitoring. Aten Prim. 2007;39(5):247–53.
Chanard J. Insuffisance rénale chronique et hypertension en pratique cardiologique de ville [Chronic renal failure and hypertension in community, experience of cardiology practice]. Presse Med. 2001;30(26):1288–94.
Froissart M, Rossert J, Jacquot C, Paillard M, Houillier P. Predictive performance of the modification of diet in renal disease and Cockcroft–Gault equations for estimating renal function. J Am Soc Nephrol. 2005;16:763–73.
Via-Sosa MA, Lopes N, March M. Effectiveness of a drug dosing service provided by community pharmacists in polymedicated elderly patients with renal impairment—a comparative study. BMC Fam Pract. 2013;14:96.
Lefèvre T. Analyse des interventions pharmaceutiques réalisées lors de la validation des prescriptions médicales, au sein d’une officine de pharmacie [Analysis of pharmaceutical interventions during the review of medical prescriptions in a community pharmacy]. J Pharm Clin. 2011;30(3):155–8.
Bryant LJM, Coster G, Gamble GD, McCormick RN. The General Practitioner–Pharmacist Collaboration (GPPC) study: a randomised controlled trial of clinical medication reviews in community pharmacy. Int J Pharm Pract. 2011;19(2):94–105.
Schlecht-Bauer D, Sautenet B, Emonet M, Hay N, Guegan F, Rosset P, et al. Insuffisance rénale et médicaments: suivis patients coordonnés entre pharmaciens officinaux et hospitaliers [Renal impairment and drugs: coordination between community pharmacists and hospital pharmacists]. Pharm Hosp Clin. 2012;47(2):123–6.
Rubio-Valera M, Jové AM, Hughes CM, Guillen-Solà M, Rovira M, Fernández A. Factors affecting collaboration between general practitioners and community pharmacists: a qualitative study. BMC Health Serv Res. 2012;7(12):188.
Funding
The study had been financed by the URPS Pharmacists of Center region.
Conflicts of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pourrat, X., Sipert, AS., Gatault, P. et al. Community pharmacist intervention in patients with renal impairment. Int J Clin Pharm 37, 1172–1179 (2015). https://doi.org/10.1007/s11096-015-0182-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-015-0182-4