Abstract
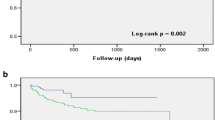
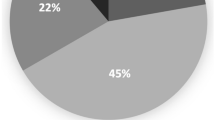
Objective Evidence from pivotal clinical trials conducted more than a decade ago supports the use of antithrombotic therapy, particularly warfarin, for stroke prevention in atrial fibrillation (AF). Despite the wide dissemination of this evidence since that time, there is anecdotal evidence that utilisation of therapy remains suboptimal, especially in the target elderly population, which is reflected in the development of practice tools such as the TAG Clinical Indicator (‘Antithrombotics in AF’ Indicator 1.6, 2007). Therefore, the objective of this study was to determine the current utilisation of antithrombotic therapy for elderly patients with AF in the local setting, and to compare this utilisation with the results of a prior audit (AUDIT 1), as well as against the recommendations of the TAG Clinical Indicator (TAG IND). Setting A major teaching hospital in Sydney, Australia. Method A retrospective audit (AUDIT 2) of medical records of hospital inpatients (aged 65 years, with a significant diagnosis of AF), pertaining to admissions over the 12-month period 1st June 2006–31st May 2007, was conducted. Main outcome measure Proportion of patients receiving antithrombotic therapy at the point of discharge from hospital. Results A total of 201 patients (mean age 79.8 ± 7.8 years) were reviewed in AUDIT 2. Most (85%) patients received antithrombotic therapy (vs. 79.2%, AUDIT 1), with “warfarin ± antiplatelets” most frequently (46.3%) used (vs. 34.5%, AUDIT 1), followed by “aspirin ± other antiplatelet” (33.3% AUDIT 2 vs. 43.1% AUDIT 1). Patients aged 80 years were significantly less likely to receive warfarin therapy, compared to those <80 years (40.2% vs. 52.5%, P = 0.01). Of those patients who were deemed ‘eligible’ for warfarin according to AUDIT 2 (n = 155), only 55.0% of patients were actually prescribed this treatment. Results obtained by AUDIT 2 and TAG IND were overall comparable. Conclusion Whilst there have been temporal improvements in the overall utilisation of antithrombotic therapy, including warfarin, there are still significant gaps in the translation of evidence from clinical trials to clinical practice. Further sustainable intervention is warranted to help apply treatment recommendations to the target population.

Similar content being viewed by others
References
Atrial Fibrillation Investigators. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. [erratum appears in Arch Intern Med 1994 Oct 10;154(19):2254]. Arch Intern Med. 1994;154:1449–57.
Bajorek BV. Stroke prevention in elderly patients with atrial fibrillation. University of Sydney, 2006, Australia: Faculty of Pharmacy; (2002).
Bajorek BV, Krass I, Ogle SJ, Duguid MJ, Shenfield GM. The impact of age on antithrombotic use in elderly patients with non-valvular atrial fibrillation. Australas J Ageing. 2002;21:36–41.
Bajorek BV, Krass I, Ogle SJ, Duguid MJ, Shenfield GM. Optimizing the use of antithrombotic therapy for atrial fibrillation in older people: a pharmacist-led multidisciplinary intervention. J Am Geriatr Soc. 2005;53:1912–20.
Bradley BC, Perdue KS, Tisdel KA, Gilligan DM. Frequency of anticoagulation for atrial fibrillation and reasons for its non-use at a Veterans Affairs medical center. Am J Cardiol. 2000;85:568–72.
Cohen N, Almoznino-Sarafian D, Alon I, Gorelik O, Koopfer M, Chachashvily S, et al. Warfarin for stroke prevention still underused in atrial fibrillation: patterns of omission. Stroke. 2000;31:1217–22.
Connolly SJ, Laupacis A, Gent M, Roberts RS, Cairns JA, Joyner C. Canadian atrial fibrillation anticoagulation (CAFA) study. J Am Coll Cardiol. 1991;18:349–55.
European Atrial Fibrillation Trial Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet. 1993;342:1255–62.
Ezekowitz MD, Bridgers SL, James KE, Carliner NH, Colling CL, Gornick CC, et al. Warfarin in the prevention of stroke associated with nonrheumatic atrial fibrillation. Veterans affairs stroke prevention in nonrheumatic atrial fibrillation investigators. N Engl J Med. 1992;327:1406–12.
Gottlieb LK, Salem-Schatz S. Anticoagulation in atrial fibrillation. Does efficacy in clinical trials translate into effectiveness in practice? Arch Intern Med. 1994;154:1945–53.
Jackson SL, Peterson GM, Vial JH. A community-based educational intervention to improve antithrombotic drug use in atrial fibrillation. Ann Pharmacother. 2004;38:1794–9.
Johnston JA, Cluxton RJ, Heaton PC, Guo JJ, Moomaw CJ, Eckman MH. Predictors of warfarin use among Ohio Medicaid patients with new-onset nonvalvular atrial fibrillation. Arch Intern Med. 2003;163:1705–10.
Lok NS, Lau CP. Presentation and management of patients admitted with atrial fibrillation: a review of 291 cases in a regional hospital. Int J Cardiol. 1995;48:271–8.
Mahmud A, Bennett K, Okechukwu I, Feely J. National underuse of anti-thrombotic therapy in chronic atrial fibrillation identified from digoxin prescribing. Br J Clin Pharmacol. 2007;64:706–9.
McNulty SJ, Hutchinson D, Hardy KJ. Implementation of antithrombotic management in atrial fibrillation. Postgrad Med J. 2000;76:783–6.
Mead GE, Wardlaw JM, Lewis SC, McDowall M, Dennis MS. The influence of randomized trials on the use of anticoagulants for atrial fibrillation. [see comment]. Age Ageing. 1999;28:441–6.
National Centre for Classification in Health (Sydney N.S.W.). The International statistical classification of diseases and related health problems, tenth revision, Australian modification (ICD-10-AM). 5th edn. National Centre for Classification in Health: Lidcombe, NSW, 2006. ISBN: 186451271.
New South Wales Therapeutic Advisory Group. Indicators for quality use of medicines in Australian hospitals. NSW TAG Inc., Australia, 2007, ISBN: 9780958606950.
Partington SL, Abid S, Teo K, Oczkowski W, O’Donnell MJ. Pre-admission warfarin use in patients with acute ischemic stroke and atrial fibrillation: the appropriate use and barriers to oral anticoagulant therapy. Thromb Res. 2007;120:663–9.
Petersen P, Boysen G, Godtfredsen J, Andersen ED, Andersen B. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Lancet. 1989;1:175–9.
Stroke Prevention in Atrial Fibrillation Investigators. Stroke prevention in atrial fibrillation study. Final results. Circulation. 1991;84:527–39.
The Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. The effect of low-dose warfarin on the risk of stroke in patients with nonrheumatic atrial fibrillation. N Engl J Med. 1990;323:1505–11.
Acknowledgments
The authors thank the Medical Records staff of Royal North Shore Hospital, as well as Niels Vermeer, for their assistance with the data collection process.
Funding
None.
Conflicts of interest
The authors declare no conflicts of interest in undertaking this study.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 4.
Rights and permissions
About this article
Cite this article
Bajorek, B.V., Ren, S. Utilisation of antithrombotic therapy for stroke prevention in atrial fibrillation in a Sydney hospital: then and now. Int J Clin Pharm 34, 88–97 (2012). https://doi.org/10.1007/s11096-011-9594-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-011-9594-y