Abstract
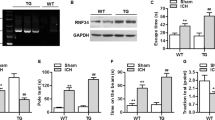
Intracerebral hemorrhage (ICH) causes long term neurological abnormality or death. Oxidative stress is closely involved in ICH mediated brain damage. Steroid receptor cofactor 3 (SRC-3), a p160 family member, is widely expressed in the brain and regulates transactivation of Nrf2, a key component of antioxidant response. Our study aims to test if SRC-3 is implicated in ICH mediated brain injury. We first examined levels of SRC-3 and oxidative stress in the brain of mice following ICH and analyzed their correlation. Then ICH was induced in wild type (WT) and SRC-3 knock out mice and how SRC-3 deletion affected ICH induced brain damage, oxidative stress and behavioral outcome was assessed. We found that SRC-3 mRNA and protein expression levels were reduced gradually after ICH induction in WT mice along with an increase in oxidative stress levels. Correlation analysis revealed that SRC-3 mRNA levels negatively correlated with oxidative stress. Deletion of SRC-3 further increased ICH induced brain edema, neurological deficit score and oxidative stress and exacerbated ICH induced behavioral abnormality including motor dysfunction and cognitive impairment. Our findings suggest that SRC-3 is involved in ICH induced brain injury, probably through modulation of oxidative stress.







Similar content being viewed by others
Data Availability
Data could be achieved upon reasonable request to the corresponding author.
References
An SJ, Kim TJ, Yoon BW (2017) Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: an update. J Stroke 19:3–10
Jolink WM, Klijn CJ, Brouwers PJ, Kappelle LJ, Vaartjes I (2015) Time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology 85:1318–1324
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ (2010) Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 9:167–176
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D, American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:2032–2060
Lok J, Leung W, Murphy S, Butler W, Noviski N, Lo EH (2011) Intracranial hemorrhage: mechanisms of secondary brain injury. Acta Neurochir Suppl 111:63–69
Duan X, Wen Z, Shen H, Shen M, Chen G (2016) Intracerebral hemorrhage, oxidative stress, and antioxidant therapy. Oxid Med Cell Longev 2016:1203285
Qi B, Hu L, Zhu L, Shang L, Wang X, Liu N, Wen N, Hong Y, Fang D (2017) Metformin attenuates neurological deficit after intracerebral hemorrhage by inhibiting apoptosis, oxidative stress and neuroinflammation in rats. Neurochem Res 42:2912–2920
Yuan R, Fan H, Cheng S, Gao W, Xu X, Lv S, Ye M, Wu M, Zhu X, Zhang Y (2017) Silymarin prevents NLRP3 inflammasome activation and protects against intracerebral hemorrhage. Biomed Pharmacother 93:308–315
Xu J, Liao L, Ning G, Yoshida-Komiya H, Deng C, O’Malley BW (2000) The steroid receptor coactivator SRC-3 (p/CIP/RAC3/AIB1/ACTR/TRAM-1) is required for normal growth, puberty, female reproductive function, and mammary gland development. Proc Natl Acad Sci USA 97:6379–6384
Kim JH, Yu S, Chen JD, Kong AN (2013) The nuclear cofactor RAC3/AIB1/SRC-3 enhances Nrf2 signaling by interacting with transactivation domains. Oncogene 32:514–527
Kuramoto Y, Takagi T, Tatebayashi K, Beppu M, Doe N, Fujita M, Yoshimura S (2019) Intravenous administration of human adipose-derived stem cells ameliorates motor and cognitive function for intracerebral hemorrhage mouse model. Brain Res 1711:58–67
Zhang H, Wang Y, Lv Q, Gao J, Hu L, He Z (2018) MicroRNA-21 overexpression promotes the neuroprotective efficacy of mesenchymal stem cells for treatment of intracerebral hemorrhage. Front Neurol 9:931
Qu X, Wang N, Chen W, Qi M, Xue Y, Cheng W (2019) RNF34 overexpression exacerbates neurological deficits and brain injury in a mouse model of intracerebral hemorrhage by potentiating mitochondrial dysfunction-mediated oxidative stress. Sci Rep 9:16296
Zhou H, Zhang H, Yan Z, Xu R (2016) Transplantation of human amniotic mesenchymal stem cells promotes neurological recovery in an intracerebral hemorrhage rat model. Biochem Biophys Res Commun 475:202–208
Krafft PR, Rolland WB, Duris K, Lekic T, Campbell A, Tang J, Zhang JH (2012) Modeling intracerebral hemorrhage in mice: injection of autologous blood or bacterial collagenase. J Vis Exp. https://doi.org/10.3791/4289
Sansing LH, Kasner SE, McCullough L, Agarwal P, Welsh FA, Kariko K (2011) Autologous blood injection to model spontaneous intracerebral hemorrhage in mice. J Vis Exp. https://doi.org/10.3791/2618
Li M, Zhang Z, Sun W, Koehler RC, Huang J (2011) 17beta-estradiol attenuates breakdown of blood-brain barrier and hemorrhagic transformation induced by tissue plasminogen activator in cerebral ischemia. Neurobiol Dis 44:277–283
Yang SH, Shi J, Day AL, Simpkins JW (2000) Estradiol exerts neuroprotective effects when administered after ischemic insult. Stroke 31:745–749; discussion 749–750
Xiao H, Deng M, Yang B, Hu Z, Tang J (2018) Pretreatment with 17beta-estradiol attenuates cerebral ischemia-induced blood-brain barrier disruption in aged rats: involvement of antioxidant signaling. Neuroendocrinology 106:20–29
Yuan Y, Liao L, Tulis DA, Xu J (2002) Steroid receptor coactivator-3 is required for inhibition of neointima formation by estrogen. Circulation 105:2653–2659
Zheng FF, Wu RC, Smith CL, O’Malley BW (2005) Rapid estrogen-induced phosphorylation of the SRC-3 coactivator occurs in an extranuclear complex containing estrogen receptor. Mol Cell Biol 25:8273–8284
Nakamura T, Xi G, Keep RF, Wang M, Nagao S, Hoff JT, Hua Y (2006) Effects of endogenous and exogenous estrogen on intracerebral hemorrhage-induced brain damage in rats. Acta Neurochir Suppl 96:218–221
Hernandez I, Delgado JL, Diaz J, Quesada T, Teruel MJ, Llanos MC, Carbonell LF (2000) 17beta-estradiol prevents oxidative stress and decreases blood pressure in ovariectomized rats. Am J Physiol Regul Integr Comp Physiol 279:R1599-1605
Brotfain E, Gruenbaum SE, Boyko M, Kutz R, Zlotnik A, Klein M (2016) Neuroprotection by estrogen and progesterone in traumatic brain injury and spinal cord injury. Curr Neuropharmacol 14:641–653
Chakrabarti M, Das A, Samantaray S, Smith JA, Banik NL, Haque A, Ray SK (2016) Molecular mechanisms of estrogen for neuroprotection in spinal cord injury and traumatic brain injury. Rev Neurosci 27:271–281
Dang J, Brandenburg LO, Rosen C, Fragoulis A, Kipp M, Pufe T, Beyer C, Wruck CJ (2012) Nrf2 expression by neurons, astroglia, and microglia in the cerebral cortical penumbra of ischemic rats. J Mol Neurosci 46:578–584
Shao Z, Tu S, Shao A (2019) Pathophysiological mechanisms and potential therapeutic targets in intracerebral hemorrhage. Front Pharmacol 10:1079
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 81801188) and the Natural Science Foundation of Hunan Province (No. 2019JJ40421).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Deng, M., Liu, J., He, J. et al. SRC-3 Deficiency Exacerbates Neurological Deficits in a Mouse Model of Intracerebral Hemorrhage: Role of Oxidative Stress. Neurochem Res 46, 2969–2978 (2021). https://doi.org/10.1007/s11064-021-03399-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-021-03399-7