Abstract
Purpose
Management of patients with large brain metastases poses a clinical challenge, with poor local control and high risk of adverse radiation events when treated with single-fraction stereotactic radiosurgery (SF-SRS). Hypofractionated SRS (HF-SRS) may be considered, but clinical data remains limited, particularly with Gamma Knife (GK) radiosurgery. We report our experience with GK to deliver mask-based HF-SRS to brain metastases greater than 10 cc in volume and present our control and toxicity outcomes.
Methods
Patients who received hypofractionated GK radiosurgery (HF-GKRS) for the treatment of brain metastases greater than 10 cc between January 2017 and June 2022 were retrospectively identified. Local failure (LF) and adverse radiation events of CTCAE grade 2 or higher (ARE) were identified. Clinical, treatment, and radiological information was collected to identify parameters associated with clinical outcomes.
Results
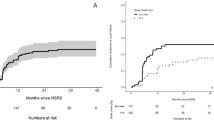
Ninety lesions (in 78 patients) greater than 10 cc were identified. The median gross tumor volume was 16.0 cc (range 10.1-56.0 cc). Prior surgical resection was performed on 49 lesions (54.4%). Six- and 12-month LF rates were 7.3% and 17.6%; comparable ARE rates were 1.9% and 6.5%. In multivariate analysis, tumor volume larger than 33.5 cc (p = 0.029) and radioresistant histology (p = 0.047) were associated with increased risk of LF (p = 0.018). Target volume was not associated with increased risk of ARE (p = 0.511).
Conclusions
We present our institutional experience treating large brain metastases using mask-based HF-GKRS, representing one of the largest studies implementing this platform and technique. Our LF and ARE compare favorably with the literature, suggesting that target volumes less than 33.5 cc demonstrate excellent control rates with low ARE. Further investigation is needed to optimize treatment technique for larger tumors.


Similar content being viewed by others
Data availability
All data and analysis script(s) generated during the current study are available from the corresponding author on reasonable request.
References
Fox BD, Cheung VJ, Patel AJ et al (2011) Epidemiology of metastatic brain tumors. Neurosurg Clin N Am 22:1–6. https://doi.org/10.1016/j.nec.2010.08.007
Shaw E, Scott C, Souhami L et al (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90 – 05. Int J Radiat Oncol 47:291–298. https://doi.org/10.1016/S0360-3016(99)00507-6
Nieder C, Berberich W, Schnabel K (1997) Tumor-related prognostic factors for remission of brain metastases after radiotherapy. Int J Radiat Oncol 39:25–30. https://doi.org/10.1016/S0360-3016(97)00154-5
Han JH, Kim DG, Chung H-T et al (2012) Radiosurgery for large brain metastases. Int J Radiat Oncol 83:113–120. https://doi.org/10.1016/j.ijrobp.2011.06.1965
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of Radiosurgery alone vs Radiosurgery with Whole Brain Radiation Therapy on cognitive function in patients with 1 to 3 brain metastases: a Randomized Clinical Trial. JAMA 316:401. https://doi.org/10.1001/jama.2016.9839
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044. https://doi.org/10.1016/S1470-2045(09)70263-3
Aoyama H, Tago M, Kato N et al (2007) Neurocognitive function of patients with Brain Metastasis who received either whole brain Radiotherapy Plus stereotactic radiosurgery or radiosurgery alone. Int J Radiat Oncol 68:1388–1395. https://doi.org/10.1016/j.ijrobp.2007.03.048
Lehrer EJ, Peterson JL, Zaorsky NG et al (2019) Single versus Multifraction Stereotactic Radiosurgery for large brain metastases: an International Meta-analysis of 24 trials. Int J Radiat Oncol 103:618–630. https://doi.org/10.1016/j.ijrobp.2018.10.038
Dohm AE, Hughes R, Wheless W et al (2018) Surgical resection and postoperative radiosurgery versus staged radiosurgery for large brain metastases. J Neurooncol 140:749–756. https://doi.org/10.1007/s11060-018-03008-8
Navarria P, Pessina F, Cozzi L et al (2016) Hypo-fractionated stereotactic radiotherapy alone using volumetric modulated arc therapy for patients with single, large brain metastases unsuitable for surgical resection. Radiat Oncol 11:76. https://doi.org/10.1186/s13014-016-0653-3
Tuleasca C, Negretti L, Faouzi M et al (2018) Radiosurgery in the management of brain metastasis: a retrospective single-center study comparing Gamma Knife and LINAC treatment. J Neurosurg 128:352–361. https://doi.org/10.3171/2016.10.JNS161480
Kennedy WR, DeWees TA, Acharya S et al (2021) Internal dose escalation associated with increased local control for melanoma brain metastases treated with stereotactic radiosurgery. J Neurosurg 135:855–861. https://doi.org/10.3171/2020.7.JNS192210
Dong P, Pérez-Andújar A, Pinnaduwage D et al (2016) Dosimetric characterization of hypofractionated Gamma Knife radiosurgery of large or complex brain tumors versus linear accelerator–based treatments. J Neurosurg 125:97–103. https://doi.org/10.3171/2016.7.GKS16881
Yan M, Holden L, Wang M et al (2022) Gamma knife icon based hypofractionated stereotactic radiosurgery (GKI-HSRS) for brain metastases: impact of dose and volume. J Neurooncol 159:705–712. https://doi.org/10.1007/s11060-022-04115-3
Mendel JT, Schroeder S, Plitt A et al (2021) Expanded Radiosurgery Capabilities utilizing Gamma Knife Icon™. Cureus. https://doi.org/10.7759/cureus.13998
Harris PA, Taylor R, Minor BL et al (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans: technical note. J Neurosurg 93:219–222. https://doi.org/10.3171/jns.2000.93.supplement_3.0219
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105:194–201. https://doi.org/10.3171/sup.2006.105.7.194
Sperduto PW, Mesko S, Li J et al (2020) Survival in patients with brain metastases: Summary Report on the updated diagnosis-specific graded Prognostic Assessment and Definition of the eligibility quotient. J Clin Oncol 38:3773–3784. https://doi.org/10.1200/JCO.20.01255
Lin NU, Lee EQ, Aoyama H et al (2015) Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16:e270–e278. https://doi.org/10.1016/S1470-2045(15)70057-4
U.S Department of Health and Human Services Common terminology criteria for adverse events (CTCAE)
Minniti G, Scaringi C, Paolini S et al (2016) Single-fraction Versus Multifraction (3 × 9 gy) stereotactic radiosurgery for large (> 2 cm) brain metastases: a comparative analysis of local control and risk of Radiation-Induced Brain Necrosis. Int J Radiat Oncol 95:1142–1148. https://doi.org/10.1016/j.ijrobp.2016.03.013
Samanci Y, Sisman U, Altintas A et al (2021) Hypofractionated frameless gamma knife radiosurgery for large metastatic brain tumors. Clin Exp Metastasis 38:31–46. https://doi.org/10.1007/s10585-020-10068-6
Lee EJ, Choi K-S, Park ES, Cho YH (2021) Single- and hypofractionated stereotactic radiosurgery for large (> 2 cm) brain metastases: a systematic review. J Neurooncol 154:25–34. https://doi.org/10.1007/s11060-021-03805-8
Park HR, Park K-W, Lee JM et al (2019) Frameless Fractionated Gamma Knife Radiosurgery with ICON™ for large metastatic brain tumors. J Korean Med Sci 34:e57. https://doi.org/10.3346/jkms.2019.34.e57
Murai T, Ogino H, Manabe Y et al (2014) Fractionated stereotactic radiotherapy using CyberKnife for the treatment of large brain metastases: a dose escalation study. Clin Oncol 26:151–158. https://doi.org/10.1016/j.clon.2013.11.027
Milano MT, Grimm J, Niemierko A et al (2021) Single- and multifraction stereotactic radiosurgery Dose/Volume tolerances of the brain. Int J Radiat Oncol 110:68–86. https://doi.org/10.1016/j.ijrobp.2020.08.013
Masucci GL (2018) Hypofractionated Radiation Therapy for large brain metastases. Front Oncol 8:379. https://doi.org/10.3389/fonc.2018.00379
Helis CA, Hughes RT, Glenn CW et al (2020) Predictors of adverse Radiation Effect in Brain Metastasis Patients treated with stereotactic radiosurgery and Immune checkpoint inhibitor therapy. Int J Radiat Oncol 108:295–303. https://doi.org/10.1016/j.ijrobp.2020.06.057
Borius P-Y, Régis J, Carpentier A et al (2021) Safety of radiosurgery concurrent with systemic therapy (chemotherapy, targeted therapy, and/or immunotherapy) in brain metastases: a systematic review. Cancer Metastasis Rev 40:341–354. https://doi.org/10.1007/s10555-020-09949-9
Tonse R, Tom MC, Mehta MP et al (2021) Integration of systemic therapy and stereotactic radiosurgery for Brain Metastases. Cancers 13:3682. https://doi.org/10.3390/cancers13153682
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Akash Mishra, Daniel Koffler, Michael Schulder and Anuj Goenka contributed to study conception and design. Data collection was performed by Akash Mishra, Daniel Koffler, Emel Calugaru, Niara Rowe, Sirisha Devi Viswanatha, Sabrina Begley, and Vikram Bajaj. Data analysis was performed by Akash Mishra. The first draft of the manuscript was written by Akash Mishra, Daniel Koffler, and Anuj Goenka. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The database utilized for the current study was approved by the Northwell Health Institutional Review Board.
Consent to participate
This retrospective database analysis did not require patient consent to participate as determined by the Northwell Health Institutional Review Board.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mishra, A., Koffler, D., Calugaru, E. et al. Let’s make size not matter: tumor control and toxicity outcomes of hypofractionated Gamma Knife radiosurgery for large brain metastases. J Neurooncol 163, 587–595 (2023). https://doi.org/10.1007/s11060-023-04365-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04365-9