Abstract
Purpose
Neurosurgeons use three main surgical approaches for left-sided glioblastoma (GB) in eloquent areas: biopsy, tumor resection under general anesthesia (GA), and awake craniotomy (AC) with brain mapping for maximal safe resection. We performed a retrospective study of functional and survival outcomes for left-sided eloquent GB, comparing these surgical approaches.
Methods
We included 87 patients with primary left-sided eloquent GB from two centers, one performing AC and the other biopsy or resection under GA. We assessed Karnofsky performance score (KPS), language and motor deficits one month after surgery, progression-free survival (PFS) and overall survival (OS).
Results
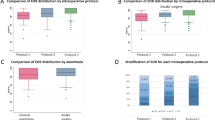
The 87 patients had a median PFS of 8.6 months [95% CI: 7.3–11.6] and a median OS of 20.2 months [17-3-24.4], with no significant differences between the three surgical approaches. One month after surgery, functional outcomes for language were similar for all approaches, but motor function was poorer in the biopsy group than in other patients. The proportion of patients with a KPS score > 80 was higher in the resection with AC group than in the other patients at this timepoint.
Conclusion
We detected no real benefit of a resection with AC over resection under GA for left-sided eloquent GB in terms of survival or functional outcomes for language. However, given the poorer motor function of biopsy patients, resection with AC should be proposed, when possible, to patients ineligible for surgical resection under GA, to improve functional outcomes and patient autonomy.


Similar content being viewed by others
Abbreviations
- AC:
-
awake craniotomy
- EOR:
-
extent of resection
- GA:
-
general anesthesia
- GB:
-
glioblastoma
- GTR:
-
gross total resection
- KPS:
-
Karnofsky performance score
- PFS:
-
progression-free survival
- STR:
-
subtotal resection
References
Miller KD, Ostrom QT, Kruchko C et al (2021) Brain and other central nervous system tumor statistics, 2021. CA Cancer J Clin 71:381–406. https://doi.org/10.3322/caac.21693
Grochans S, Cybulska AM, Simińska D et al (2022) Epidemiology of Glioblastoma Multiforme-Literature Review. https://doi.org/10.3390/cancers14102412. Cancers 14:
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466. https://doi.org/10.1016/S1470-2045(09)70025-7
Chaichana KL, Jusue-Torres I, Navarro-Ramirez R et al (2014) Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro-Oncol 16:113–122. https://doi.org/10.1093/neuonc/not137
Keime-Guibert F, Chinot O, Taillandier L et al (2007) Radiotherapy for glioblastoma in the elderly. N Engl J Med 356:1527–1535. https://doi.org/10.1056/NEJMoa065901
Lacroix M, Abi-Said D, Fourney DR et al (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95:190–198. https://doi.org/10.3171/jns.2001.95.2.0190
Li YM, Suki D, Hess K, Sawaya R (2016) The influence of maximum safe resection of glioblastoma on survival in 1229 patients: Can we do better than gross-total resection? J Neurosurg 124:977–988. https://doi.org/10.3171/2015.5.JNS142087
Orringer D, Lau D, Khatri S et al (2012) Extent of resection in patients with glioblastoma: limiting factors, perception of resectability, and effect on survival. J Neurosurg 117:851–859. https://doi.org/10.3171/2012.8.JNS12234
Stummer W, van den Bent MJ, Westphal M (2011) Cytoreductive surgery of glioblastoma as the key to successful adjuvant therapies: new arguments in an old discussion. Acta Neurochir (Wien) 153:1211–1218. https://doi.org/10.1007/s00701-011-1001-x
Giussani C, Di Cristofori A (2020) Awake craniotomy for glioblastomas: is it worth it? Considerations about the article entitled “Impact of intraoperative stimulation mapping on high-grade glioma surgery outcome: a meta-analysis”. Acta Neurochir (Wien) 162:427–428. https://doi.org/10.1007/s00701-019-04173-z
Müller DMJ, Robe PAJT, Eijgelaar RS et al (2019) Comparing Glioblastoma Surgery Decisions Between Teams Using Brain Maps of Tumor Locations, Biopsies, and Resections. JCO Clin Cancer Inform 3:1–12. https://doi.org/10.1200/CCI.18.00089
BROWN JW, HÉCAEN H (1976) Lateralization and language representation. Neurology 26:183. https://doi.org/10.1212/WNL.26.2.183
Lemée J-M, Berro DH, Bernard F et al (2019) Resting-state functional magnetic resonance imaging versus task-based activity for language mapping and correlation with perioperative cortical mapping. Brain Behav 9:e01362. https://doi.org/10.1002/brb3.1362
Bernard F, Lemée J-M, Ter Minassian A, Menei P (2018) Right Hemisphere Cognitive Functions: From Clinical and Anatomic Bases to Brain Mapping During Awake Craniotomy Part I: Clinical and Functional Anatomy. World Neurosurg 118:348–359. https://doi.org/10.1016/j.wneu.2018.05.024
Lemée J-M, Bernard F, Ter Minassian A, Menei P (2018) Right Hemisphere Cognitive Functions: From Clinical and Anatomical Bases to Brain Mapping During Awake Craniotomy. Part II: Neuropsychological Tasks and Brain Mapping. World Neurosurg 118:360–367. https://doi.org/10.1016/j.wneu.2018.07.099
Duffau H (2018) Is non-awake surgery for supratentorial adult low-grade glioma treatment still feasible? Neurosurg Rev 41:133–139. https://doi.org/10.1007/s10143-017-0918-9
Clavreul A, Aubin G, Delion M et al (2021) What effects does awake craniotomy have on functional and survival outcomes for glioblastoma patients? J Neurooncol 151:113–121. https://doi.org/10.1007/s11060-020-03666-7
Gerritsen JKW, Viëtor CL, Rizopoulos D et al (2019) Awake craniotomy versus craniotomy under general anesthesia without surgery adjuncts for supratentorial glioblastoma in eloquent areas: a retrospective matched case-control study. Acta Neurochir (Wien) 161:307–315. https://doi.org/10.1007/s00701-018-03788-y
Gerritsen JKW, Arends L, Klimek M et al (2019) Impact of intraoperative stimulation mapping on high-grade glioma surgery outcome: a meta-analysis. Acta Neurochir (Wien) 161:99–107. https://doi.org/10.1007/s00701-018-3732-4
Li Y-C, Chiu H-Y, Lin Y-J et al (2021) The Merits of Awake Craniotomy for Glioblastoma in the Left Hemispheric Eloquent Area: One Institution Experience. Clin Neurol Neurosurg 200:106343. https://doi.org/10.1016/j.clineuro.2020.106343
Moiraghi A, Roux A, Peeters S et al (2021) Feasibility, Safety and Impact on Overall Survival of Awake Resection for Newly Diagnosed Supratentorial IDH-Wildtype Glioblastomas in Adults. Cancers 13. https://doi.org/10.3390/cancers13122911
Nakajima R, Kinoshita M, Okita H et al (2019) Awake surgery for glioblastoma can preserve independence level, but is dependent on age and the preoperative condition. J Neurooncol. https://doi.org/10.1007/s11060-019-03216-w
Zhang JJY, Lee KS, Voisin MR et al (2020) Awake craniotomy for resection of supratentorial glioblastoma: a systematic review and meta-analysis. Neuro-Oncol Adv 2:vdaa111. https://doi.org/10.1093/noajnl/vdaa111
Zigiotto L, Annicchiarico L, Corsini F et al (2020) Effects of supra-total resection in neurocognitive and oncological outcome of high-grade gliomas comparing asleep and awake surgery. J Neurooncol 148:97–108. https://doi.org/10.1007/s11060-020-03494-9
Delion M, Klinger E, Bernard F et al (2020) Immersing Patients in a Virtual Reality Environment for Brain Mapping During Awake Surgery: Safety Study. World Neurosurg 134:e937–e943. https://doi.org/10.1016/j.wneu.2019.11.047
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol Off J Am Soc Clin Oncol 28:1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Coluccia D, Roth T, Marbacher S, Fandino J (2018) Impact of Laterality on Surgical Outcome of Glioblastoma Patients: A Retrospective Single-Center Study. World Neurosurg 114:e121–e128. https://doi.org/10.1016/j.wneu.2018.02.084
Hrabalek L, Kalita O, Vaverka M et al (2015) Resection versus biopsy of glioblastomas in eloquent brain areas. Biomed Pap Med Fac Univ Palacky Olomouc Czechoslov 159:150–155. https://doi.org/10.5507/bp.2013.052
McGirt MJ, Mukherjee D, Chaichana KL et al (2009) Association of surgically acquired motor and language deficits on overall survival after resection of glioblastoma multiforme. Neurosurgery 65:463–469 discussion 469–470. https://doi.org/10.1227/01.NEU.0000349763.42238.E9
Rahman M, Abbatematteo J, De Leo EK et al (2017) The effects of new or worsened postoperative neurological deficits on survival of patients with glioblastoma. J Neurosurg 127:123–131. https://doi.org/10.3171/2016.7.JNS16396
Sanai N, Martino J, Berger MS (2012) Morbidity profile following aggressive resection of parietal lobe gliomas. J Neurosurg 116:1182–1186. https://doi.org/10.3171/2012.2.JNS111228
Kim Y-J, Lee DJ, Park C-K, Kim IA (2019) Optimal extent of resection for glioblastoma according to site, extension, and size: a population-based study in the temozolomide era. Neurosurg Rev 42:937–950. https://doi.org/10.1007/s10143-018-01071-3
Paiva WS, Fonoff ET, Beer-Furlan A et al (2019) Evaluation of Postoperative Deficits following Motor Cortex Tumor Resection using Small Craniotomy. Surg J N Y N 5:e8–e13. https://doi.org/10.1055/s-0039-1679931
Serletis D, Bernstein M (2007) Prospective study of awake craniotomy used routinely and nonselectively for supratentorial tumors. J Neurosurg 107:1–6. https://doi.org/10.3171/JNS-07/07/0001
De Witt Hamer PC, Robles SG, Zwinderman AH et al (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol Off J Am Soc Clin Oncol 30:2559–2565. https://doi.org/10.1200/JCO.2011.38.4818
Duffau H (2005) Lessons from brain mapping in surgery for low-grade glioma: insights into associations between tumour and brain plasticity. Lancet Neurol 4:476–486. https://doi.org/10.1016/S1474-4422(05)70140-X
Eseonu CI, Rincon-Torroella J, ReFaey K et al (2017) Awake Craniotomy vs Craniotomy Under General Anesthesia for Perirolandic Gliomas: Evaluating Perioperative Complications and Extent of Resection. Neurosurgery 81:481–489. https://doi.org/10.1093/neuros/nyx023
Sacko O, Lauwers-Cances V, Brauge D et al (2011) Awake craniotomy vs surgery under general anesthesia for resection of supratentorial lesions. Neurosurgery 68:1192–1198 discussion 1198–1199. https://doi.org/10.1227/NEU.0b013e31820c02a3
Berger MS, Ojemann GA, Lettich E (1990) Neurophysiological monitoring during astrocytoma surgery. Neurosurg Clin N Am 1:65–80
Ojemann JG, Miller JW, Silbergeld DL (1996) Preserved function in brain invaded by tumor. Neurosurgery 39:253–258 discussion 258–259. https://doi.org/10.1097/00006123-199608000-00003
Schupper AJ, Rao M, Mohammadi N et al (2021) Fluorescence-Guided Surgery: A Review on Timing and Use in Brain Tumor Surgery. Front Neurol 12:682151. https://doi.org/10.3389/fneur.2021.682151
Sanai N, Mirzadeh Z, Berger MS (2008) Functional outcome after language mapping for glioma resection. N Engl J Med 358:18–27. https://doi.org/10.1056/NEJMoa067819
Saito T, Muragaki Y, Tamura M et al (2022) Awake craniotomy with transcortical motor evoked potential monitoring for resection of gliomas within or close to motor-related areas: validation of utility for predicting motor function. J Neurosurg 136:1052–1061. https://doi.org/10.3171/2021.3.JNS21374
Szelényi A, Hattingen E, Weidauer S et al (2010) Intraoperative motor evoked potential alteration in intracranial tumor surgery and its relation to signal alteration in postoperative magnetic resonance imaging. Neurosurgery 67:302–313. https://doi.org/10.1227/01.NEU.0000371973.46234.46
Brown TJ, Glantz M (2016) Extent of Resection and Survival in Glioblastoma Multiforme-Reply. JAMA Oncol 2:1509–1510. https://doi.org/10.1001/jamaoncol.2016.3812
Incekara F, Smits M, van der Voort SR et al (2020) The Association Between the Extent of Glioblastoma Resection and Survival in Light of MGMT Promoter Methylation in 326 Patients With Newly Diagnosed IDH-Wildtype Glioblastoma. Front Oncol 10:1087. https://doi.org/10.3389/fonc.2020.01087
Revilla-Pacheco F, Rodríguez-Salgado P, Barrera-Ramírez M et al (2021) Extent of resection and survival in patients with glioblastoma multiforme: Systematic review and meta-analysis. Med (Baltim) 100:e26432. https://doi.org/10.1097/MD.0000000000026432
Clavreul A, Soulard G, Lemée J-M et al (2019) The French glioblastoma biobank (FGB): a national clinicobiological database. J Transl Med 17:133. https://doi.org/10.1186/s12967-019-1859-6
Jakola AS, Gulati S, Weber C et al (2011) Postoperative deterioration in health related quality of life as predictor for survival in patients with glioblastoma: a prospective study. PLoS ONE 6:e28592. https://doi.org/10.1371/journal.pone.0028592
Gerritsen JKW, Klimek M, Dirven CMF et al (2019) The SAFE-trial: Safe surgery for glioblastoma multiforme: Awake craniotomy versus surgery under general anesthesia. Study protocol for a multicenter prospective randomized controlled trial. Contemp Clin Trials 88:105876. https://doi.org/10.1016/j.cct.2019.105876
Acknowledgements
We thank the neuroradiologists, neuropathologists, radiation oncologists and medical oncologists who followed patients. We also thank Ghislaine Aubin and Gwénaëlle Soulard for their help in data recovery and exploitation and Alex Edelman and Associates for correcting the manuscript. We would like also to thank the French Glioblastoma Biobank (CHU Angers, Angers, France).
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to study conception and design. The data were collected and analyzed by Clémentine Gallet, Anne Clavreul and Jean-Michel Lemée. The first draft of the manuscript was written by Clémentine Gallet and all the authors commented on intermediate versions of the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gallet, C., Clavreul, A., Morandi, X. et al. What surgical approach for left-sided eloquent glioblastoma: biopsy, resection under general anesthesia or awake craniotomy?. J Neurooncol 160, 445–454 (2022). https://doi.org/10.1007/s11060-022-04163-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-022-04163-9