Abstract
Purpose
Cerebral edema from brain tumors can cause neurological impairment. Steroids treat edema but with possible adverse effects. We surveyed providers regarding steroid use in newly diagnosed patients with brain tumors to determine if practices are standard or markedly variable.
Methods
An anonymous voluntary online survey was sent to members of neuro-oncology consortiums. Four clinical scenarios were provided and questions regarding initiation of steroids, type, dose, formulation, and duration were asked. Demographic information was collected.
Results
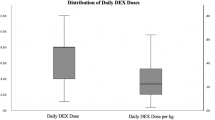
369 providers received the survey, 76 responded (20.6% response rate). The proportion of providers who would start steroids significantly differed among scenarios (scenario 1 vs 2, p < 0.001; 2 vs 3, p < 0.001; 1 vs 3, p < 0.001). 75 (98.7%) providers would start steroids for vasogenic edema (scenario 1) and 55 (72.4%) for obstructive hydrocephalus (scenario 2). 16 (21.1%) would start steroids for vasogenic edema but not obstructive hydrocephalus. The odds of choosing to start steroids in patients with obstructive hydrocephalus were 7.59 times more (95% CI: 2.29, 25.13) if providers felt symptoms would improve within 24 h. All would use dexamethasone. A significant difference was seen between the proportion of providers who would give a loading dose if vasogenic edema with neurological deficits were noted versus vasogenic edema alone (57.9% vs 43.4%; p = 0.002).
Conclusions
These results suggest that providers recommend dexamethasone for patients with vasogenic edema and obstructive hydrocephalus. Variability remains with dosing schedule. Further studies are needed to identify the most appropriate use of steroids for newly diagnosed CNS tumor patients with the goal to create steroid management guidelines.


Similar content being viewed by others
References
Kaal EC, Vecht CJ (2004) The management of brain edema in brain tumors. Curr Opin Oncol 16(6):593–600
Esquenazi Y, Lo VP, Lee K (2017) Critical care management of cerebral edema in brain tumors. J Intensive Care Med 32(1):15–24. https://doi.org/10.1177/0885066615619618
Ingraham FD, Matson DD, Mc LR (1952) Cortisone and ACTH as an adjunct to the surgery of craniopharyngiomas. N Engl J Med 246(15):568–571. https://doi.org/10.1056/nejm195204102461502
Batchelor TT, Byrne TN (2008) Neurological complications of primary brain tumors. In: Schiff D, Kesari S, Wen PY (eds) Cancer neurology in clinical practice: neurologic complications of cancer and its treatment. Humana Press, Totowa, pp 381–396. https://doi.org/10.1007/978-1-59745-412-4_20
Ryan R, Booth S, Price S (2012) Corticosteroid-use in primary and secondary brain tumour patients: a review. J Neuro-oncol 106(3):449–459. https://doi.org/10.1007/s11060-011-0713-3
Bebawy JF (2012) Perioperative steroids for peritumoral intracranial edema: a review of mechanisms, efficacy, and side effects. J Neurosurg Anesthesiol 24(3):173–177. https://doi.org/10.1097/ANA.0b013e3182578bb5
Kofman S, Garvin JS, Nagamani D, Taylor SG (1957) Treatment of cerebral metastases from breast carcinoma with prednisolone. J Am Med Assoc 163(16):1473–1476
Pollack IF (1994) Brain tumors in children. N Engl J Med 331(22):1500–1507. https://doi.org/10.1056/nejm199412013312207
Lindvall-Axelsson M, Hedner P, Owman C (1989) Corticosteroid action on choroid plexus: reduction in Na+-K+-ATPase activity, choline transport capacity, and rate of CSF formation. Exp Brain Res 77(3):605–610. https://doi.org/10.1007/bf00249613
Schmid UD, Seiler RW (1986) Management of obstructive hydrocephalus secondary to posterior fossa tumors by steroids and subcutaneous ventricular catheter reservoir. J Neurosurg 65(5):649–653. https://doi.org/10.3171/jns.1986.65.5.0649
Glaser AW, Buxton N, Walker D (1997) Corticosteroids in the management of central nervous system tumours. Kids Neuro-Oncology Workshop (KNOWS). Arch Dis Childhood 76(1):76–78
Sainte-Rose C, Cinalli G, Roux FE, Maixner R, Chumas PD, Mansour M, Carpentier A, Bourgeois M, Zerah M, Pierre-Kahn A, Renier D (2001) Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 95(5):791–797. https://doi.org/10.3171/jns.2001.95.5.0791
Di Rocco F, Juca CE, Zerah M, Sainte-Rose C (2013) Endoscopic third ventriculostomy and posterior fossa tumors. World Neurosurg 79(2 Suppl):S18.e15–19. https://doi.org/10.1016/j.wneu.2012.02.018
Sarin R, Murthy V (2003) Medical decompressive therapy for primary and metastatic intracranial tumours. Lancet Neurol 2(6):357–365. https://doi.org/10.1016/s1474-4422(03)00410-1
Stummer W (2007) Mechanisms of tumor-related brain edema. Neurosurg Focus 22(5):E8
Ryken TC, McDermott M, Robinson PD, Ammirati M, Andrews DW, Asher AL, Burri SH, Cobbs CS, Gaspar LE, Kondziolka D, Linskey ME, Loeffler JS, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Kalkanis SN (2010) The role of steroids in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neuro-Oncol 96(1):103–114. https://doi.org/10.1007/s11060-009-0057-4
Roth P, Wick W, Weller M (2010) Steroids in neurooncology: actions, indications, side-effects. Curr Opin Neurol 23(6):597–602. https://doi.org/10.1097/WCO.0b013e32833e5a5d
Sturdza A, Millar BA, Bana N, Laperriere N, Pond G, Wong RK, Bezjak A (2008) The use and toxicity of steroids in the management of patients with brain metastases. Support Care Cancer 16(9):1041–1048. https://doi.org/10.1007/s00520-007-0395-8
Ryken TC, Kuo JS, Prabhu RS, Sherman JH, Kalkanis SN, Olson JJ (2019) Congress of neurological surgeons systematic review and evidence-based guidelines on the role of steroids in the treatment of adults with metastatic brain tumors. Neurosurgery 84(3):E189–e191. https://doi.org/10.1093/neuros/nyy546
Alan N, Seicean A, Seicean S, Neuhauser D, Benzel EC, Weil RJ (2015) Preoperative steroid use and the incidence of perioperative complications in patients undergoing craniotomy for definitive resection of a malignant brain tumor. J Clin Neurosci 22(9):1413–1419. https://doi.org/10.1016/j.jocn.2015.03.009
Veldhuijzen van Zanten SE, Cruz O, Kaspers GJ, Hargrave DR, van Vuurden DG (2016) State of affairs in use of steroids in diffuse intrinsic pontine glioma: an international survey and a review of the literature. J Neuro-Oncol 128(3):387–394. https://doi.org/10.1007/s11060-016-2141-x
Packer RM, TJ and Vezina G. (2012) Tumors of the brain and spine. In: Swaiman KFAS, Ferriero DM, Schor NF (ed) Pediatric neurology principles and practice, vol 2. 5 edn. Elsevier, New York, pp 1339–1387
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Malbari, F., Staggers, K.A., Minard, C.G. et al. Provider views on perioperative steroid use for patients with newly diagnosed pediatric brain tumors. J Neurooncol 147, 205–212 (2020). https://doi.org/10.1007/s11060-020-03416-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03416-9