Abstract
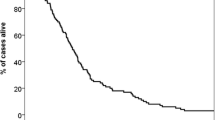
Patients treated with stereotactic radiosurgery (SRS) for brain metastases (BM) are at increased risk of distant brain failure (DBF). Two nomograms have been recently published to predict individualized risk of DBF after SRS. The goal of this study was to assess the external validity of these nomograms in an independent patient cohort. The records of consecutive patients with BM treated with SRS at Levine Cancer Institute and Emory University between 2005 and 2013 were reviewed. Three validation cohorts were generated based on the specific nomogram or recursive partitioning analysis (RPA) entry criteria: Wake Forest nomogram (n = 281), Canadian nomogram (n = 282), and Canadian RPA (n = 303) validation cohorts. Freedom from DBF at 1-year in the Wake Forest study was 30% compared with 50% in the validation cohort. The validation c-index for both the 6-month and 9-month freedom from DBF Wake Forest nomograms was 0.55, indicating poor discrimination ability, and the goodness-of-fit test for both nomograms was highly significant (p < 0.001), indicating poor calibration. The 1-year actuarial DBF in the Canadian nomogram study was 43.9% compared with 50.9% in the validation cohort. The validation c-index for the Canadian 1-year DBF nomogram was 0.56, and the goodness-of-fit test was also highly significant (p < 0.001). The validation accuracy and c-index of the Canadian RPA classification was 53% and 0.61, respectively. The Wake Forest and Canadian nomograms for predicting risk of DBF after SRS were found to have limited predictive ability in an independent bi-institutional validation cohort. These results reinforce the importance of validating predictive models in independent patient cohorts.



Similar content being viewed by others
References
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491. https://doi.org/10.1001/jama.295.21.2483
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044. https://doi.org/10.1016/S1470-2045(09)70263-3
Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Ben Hassel M, Kouri M, Valeinis E, van den Berge D, Collette S, Collette L, Mueller RP (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29:134–141. https://doi.org/10.1200/JCO.2010.30.1655
Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK, Carrero XW, Barker FG 2nd, Deming R, Burri SH, Menard C, Chung C, Stieber VW, Pollock BE, Galanis E, Buckner JC, Asher AL (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316: 401–409 https://doi.org/10.1001/jama.2016.9839
Soffietti R, Kocher M, Abacioglu UM, Villa S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Ben Hassel M, Kouri M, Valeinis E, van den Berge D, Mueller RP, Tridello G, Collette L, Bottomley A (2013) A European Organisation for Research and Treatment of Cancer phase III trial of adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: quality-of-life results. J Clin Oncol 31:65–72. https://doi.org/10.1200/JCO.2011.41.0639
Ayala-Peacock DN, Peiffer AM, Lucas JT, Isom S, Kuremsky JG, Urbanic JJ, Bourland JD, Laxton AW, Tatter SB, Shaw EG, Chan MD (2014) A nomogram for predicting distant brain failure in patients treated with gamma knife stereotactic radiosurgery without whole brain radiotherapy. Neuro-oncology 16:1283–1288. https://doi.org/10.1093/neuonc/nou018
Rodrigues G, Warner A, Zindler J, Slotman B, Lagerwaard F (2014) A clinical nomogram and recursive partitioning analysis to determine the risk of regional failure after radiosurgery alone for brain metastases. Radiother Oncol 111:52–58. https://doi.org/10.1016/j.radonc.2013.11.015
Altman DG, Royston P (2000) What do we mean by validating a prognostic model? Stat Med 19:453–473
Altman DG, Vergouwe Y, Royston P, Moons KG (2009) Prognosis and prognostic research: validating a prognostic model. BMJ 338:b605. https://doi.org/10.1136/bmj.b605
Steyerberg EW, Moons KG, van der Windt DA, Hayden JA, Perel P, Schroter S, Riley RD, Hemingway H, Altman DG, Group P (2013) Prognosis Research Strategy (PROGRESS) 3: prognostic model research. PLoS Med 10:e1001381. https://doi.org/10.1371/journal.pmed.1001381
Press RH, Prabhu RS, Nickleach DC, Liu Y, Shu HK, Kandula S, Patel KR, Curran WJ, Crocker I (2015) Novel risk stratification score for predicting early distant brain failure and salvage whole-brain radiotherapy after stereotactic radiosurgery for brain metastases. Cancer 121:3836–3843. https://doi.org/10.1002/cncr.29590
Prabhu RS, Dhabaan A, Hall WA, Ogunleye T, Crocker I, Curran WJ, Shu HK (2013) Clinical outcomes for a novel 6 degrees of freedom image guided localization method for frameless radiosurgery for intracranial brain metastases. J Neuro-Oncol 113:93–99. https://doi.org/10.1007/s11060-013-1093-7
Patel KR, Burri SH, Asher AL, Crocker IR, Fraser RW, Zhang C, Chen Z, Kandula S, Zhong J, Press RH, Olson JJ, Oyesiku NM, Wait SD, Curran WJ, Shu HK, Prabhu RS (2016) Comparing preoperative with postoperative stereotactic radiosurgery for resectable brain metastases: a multi-institutional analysis. Neurosurgery 79:279–285. https://doi.org/10.1227/NEU.0000000000001096
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90 – 05. Int J Radiat Oncol Biol Phys 47:291–298
D’Agostino RB, Nam B-H (2003) Evaluation of the performance of survival analysis models: discrimination and calibration measures. Handbook of Statistics, Elsevier, pp 1–25
Halasz LM, Weeks JC, Neville BA, Taback N, Punglia RS (2013) Use of stereotactic radiosurgery for brain metastases from non-small cell lung cancer in the United States. Int J Radiat Oncol Biol Phys 85:e109–e116. https://doi.org/10.1016/j.ijrobp.2012.08.007
Austin PC, Lee DS, Fine JP (2016) Introduction to the analysis of survival data in the presence of competing risks. Circulation 133:601–609. https://doi.org/10.1161/CIRCULATIONAHA.115.017719
Berry SD, Ngo L, Samelson EJ, Kiel DP (2010) Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc 58:783–787. https://doi.org/10.1111/j.1532-5415.20
Wolkewitz M, Cooper BS, Bonten MJ, Barnett AG, Schumacher M (2014) Interpreting and comparing risks in the presence of competing events. BMJ 349:g5060. https://doi.org/10.1136/bmj.g5060
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prabhu, R.S., Press, R.H., Boselli, D.M. et al. External validity of two nomograms for predicting distant brain failure after radiosurgery for brain metastases in a bi-institutional independent patient cohort. J Neurooncol 137, 147–154 (2018). https://doi.org/10.1007/s11060-017-2707-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2707-2