Abstract
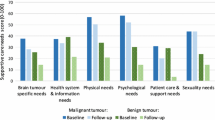
Objective of this study aimed at assessing glioma patients’ supportive care needs in a neurosurgical outpatient setting and identifying factors that are associated with needs for support. In three neuro-oncological outpatient departments, glioma patients were assessed for their psychosocial needs using the Supportive Care Needs Survey short-form (SCNS-SF34-G). Associations between clinical, sociodemographic, treatment related factors as well as distress (measured with the distress thermometer) and supportive care needs were explored using multivariable general linear models. One-hundred and seventy three of 244 eligible glioma patients participated, most of them with primary diagnoses of a high-grade glioma (81%). Highest need for support was observed in ‘psychological needs’ (median 17.5, range 5–45) followed by ‘physical and daily living needs’ (median 12.5, range 0–25) and ‘health system and information needs’ (median 11.3, range 0–36). Needs in the psychological area were associated with distress (R2 = 0.36) but not with age, sex, Karnofsky performance status (KPS), extend of resection, currently undergoing chemotherapy and whether guidance during assessment was offered. Regarding ‘health system and information needs’, we observed associations with distress, age, currently undergoing chemotherapy and guidance (R2 = 0.31). In the domain ‘physical and daily living needs’ we found associations with KPS, residual tumor, as well as with distress (R2 = 0.37). Glioma patients in neuro-oncological departments report unmet supportive care needs, especially in the psychological domain. Distress is the factor most consistently associated with unmet needs requiring support and could serve as indicator for clinical neuro-oncologists to initiate support.


Similar content being viewed by others
References
Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R et al (2015) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol 17(Suppl 4):iv1–iv62
Robin AM, Kalkanis SN, Rock J, Lee I, Rosenblum ML (2014) Through the patient’s eyes: an emphasis on patient-centered values in operative decision making in the management of malignant glioma. J Neurooncol 119:473–479
Rooney AG, Carson A, Grant R (2011) Depression in cerebral glioma patients: a systematic review of observational studies. J Natl Cancer Inst 103:61–76
Ford E, Catt S, Chalmers A, Fallowfield L (2012) Systematic review of supportive care needs in patients with primary malignant brain tumors. Neuro Oncol 14:392–404
Goebel S, Stark AM, Kaup L, von Harscher M, Mehdorn HM (2011) Distress in patients with newly diagnosed brain tumours. Psychooncology 20:623–630
Janda M, Steginga S, Langbecker D, Dunn J, Walker D et al (2007) Quality of life among patients with a brain tumor and their carers. J Psychosom Res 63:617–623
Struik K, Klein M, Heimans JJ, Gielissen MF, Bleijenberg G et al (2009) Fatigue in low-grade glioma. J Neurooncol 92:73–78
Walbert T (2014) Integration of palliative care into the neuro-oncology practice: patterns in the United States. Neurooncol Pract 1:3–7
Dirven L, Taphoorn MJ, Reijneveld JC, Blazeby J, Jacobs M et al (2014) The level of patient-reported outcome reporting in randomised controlled trials of brain tumour patients: a systematic review. Eur J Cancer 50:2432–2448
Koekkoek JA, Dirven L, Reijneveld JC, Sizoo EM, Pasman HR et al (2014) End of life care in high-grade glioma patients in three European countries: a comparative study. J Neurooncol 120:303–310
Taphoorn MJ, Sizoo EM, Bottomley A (2010) Review on quality of life issues in patients with primary brain tumors. Oncologist 15:618–626
Luckett T, King MT, Butow PN, Oguchi M, Rankin N et al (2011) Choosing between the EORTC QLQ-C30 and FACT-G for measuring health-related quality of life in cancer clinical research: issues, evidence and recommendations. Ann Oncol 22:2179–2190
Heimans JJ, Taphoorn MJ (2002) Impact of brain tumour treatment on quality of life. J Neurol 249:955–960
Sprangers MA, Cull A, Bjordal K, Groenvold M, Aaronson NK (1993) The European Organization for Research and Treatment of Cancer. Approach to quality of life assessment: guidelines for developing questionnaire modules. EORTC Study Group on Quality of Life. Qual Life Res 2:287–295
Taphoorn MJ, Claassens L, Aaronson NK, Coens C, Mauer M et al (2010) An international validation study of the EORTC brain cancer module (EORTC QLQ-BN20) for assessing health-related quality of life and symptoms in brain cancer patients. Eur J Cancer 46:1033–1040
Mehnert A, Lehmann C, Schulte T, Koch U (2007) Presence of symptom distress and prostate cancer-related anxiety in patients at the beginning of cancer rehabilitation. Onkologie 30:551–556
National Comprehensive Cancer Network (2003) Distress management. Clinical practice guidelines. J Natl Compr Canc Netw 1:344–374
Goebel S, Mehdorn HM (2011) Measurement of psychological distress in patients with intracranial tumours: the NCCN distress thermometer. J Neurooncol 104:357–364
Lehmann C, Koch U, Mehnert A (2012) Psychometric properties of the German version of the Short-Form Supportive Care Needs Survey Questionnaire (SCNS-SF34-G). Support Care Cancer 20:2415–2424
Schildmann EK, Groeneveld EI, Denzel J, Brown A, Bernhardt F et al (2016) Discovering the hidden benefits of cognitive interviewing in two languages: the first phase of a validation study of the Integrated Palliative care Outcome Scale. Palliat Med 30:599–610
Catt S, Chalmers A, Fallowfield L (2008) Psychosocial and supportive-care needs in high-grade glioma. Lancet Oncol 9:884–891
Piil K, Juhler M, Jakobsen J, Jarden M (2015) Daily life experiences of patients with a high-grade glioma and their caregivers: a longitudinal exploration of rehabilitation and supportive care needs. J Neurosci Nurs 47:271–284
Sterckx W, Coolbrandt A, Clement P, Borgenon S, Decruyenaere M et al (2015) Living with a high-grade glioma: a qualitative study of patients’ experiences and care needs. Eur J Oncol Nurs 19:383–390
Philip J, Collins A, Brand CA, Moore G, Lethborg C et al (2014) “I’m just waiting...”: an exploration of the experience of living and dying with primary malignant glioma. Support Care Cancer 22:389–397
Halkett GK, Lobb EA, Rogers MM, Shaw T, Long AP et al (2015) Predictors of distress and poorer quality of life in high grade glioma patients. Patient Educ Couns 98:525–532
Goebel S, von Harscher M, Mehdorn HM (2011) Comorbid mental disorders and psychosocial distress in patients with brain tumours and their spouses in the early treatment phase. Support Care Cancer 19:1797–1805
Ostgathe C, Gaertner J, Kotterba M, Klein S, Lindena G et al (2010) Differential palliative care issues in patients with primary and secondary brain tumours. Support Care Cancer 18:1157–1163
Snyder CF, Herman JM, White SM, Luber BS, Blackford AL et al (2014) When using patient-reported outcomes in clinical practice, the measure matters: a randomized controlled trial. J Oncol Pract 10:e299–e306
Mitchell AJ, Lord K, Slattery J, Grainger L, Symonds P (2012) How feasible is implementation of distress screening by cancer clinicians in routine clinical care? Cancer 118:6260–6269
Hickmann AK, Hechtner M, Nadji-Ohl M, Janko M, Reuter AK et al (2016) Evaluating patients for psychosocial distress and supportive care needs based on health-related quality of life in primary brain tumors: a prospective multicenter analysis of patients with gliomas in an outpatient setting. J Neurooncol 131(1):135–151. doi:10.1007/s11060-016-2280-0
Renovanz M, Hickmann AK, Coburger J, Kohlmann K, Janko M et al (2016) Assessing psychological and supportive care needs in glioma patients—feasibility study on the use of the Supportive Care Needs Survey Short Form (SCNS-SF34-G) and the Supportive Care Needs Survey Screening Tool (SCNS-ST9) in clinical practice. Eur J Cancer Care (Engl). doi:10.1111/ecc.12598
Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L et al (2000) The unmet supportive care needs of patients with cancer. Support Care Rev Group Cancer 88:226–237
Richardson A, Medina J, Brown V, Sitzia J (2007) Patients’ needs assessment in cancer care: a review of assessment tools. Support Care Cancer 15:1125–1144
Reeve BB, Wyrwich KW, Wu AW, Velikova G, Terwee CB et al (2013) ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual Life Res 22:1889–1905
Armstrong TS, Gilbert MR (2014) Patient reported endpoints for measuring clinical benefit in (high grade glioma) primary brain tumor patients. Curr Treat Options Oncol 15:519–528
Snyder CF, Garrett-Mayer E, Blackford AL, Brahmer JR, Carducci MA et al (2009) Concordance of cancer patients’ function, symptoms, and supportive care needs. Qual Life Res 18:991–998
Janda M, Steginga S, Dunn J, Langbecker D, Walker D et al (2008) Unmet supportive care needs and interest in services among patients with a brain tumour and their carers. Patient Educ Couns 71:251–258
Heese O, Schmidt M, Nickel S, Berger H, Goldbrunner R et al (2010) Complementary therapy use in patients with glioma: an observational study. Neurology 75:2229–2235
Mulpur BH, Nabors LB, Thompson RC, Olson JJ, LaRocca RV et al (2015) Complementary therapy and survival in glioblastoma. Neurooncol Pract 2:122–126
Gaertner J, Wolf J, Frechen S, Klein U, Scheicht D et al (2012) Recommending early integration of palliative care: does it work? Support Care Cancer 20:507–513
Gaertner J, Wolf J, Hallek M, Glossmann JP, Voltz R (2011) Standardizing integration of palliative care into comprehensive cancer therapy: a disease specific approach. Support Care Cancer 19:1037–1043
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Rooney AG, McNamara S, Mackinnon M, Fraser M, Rampling R et al (2013) The frequency, longitudinal course, clinical associations, and causes of emotional distress during primary treatment of cerebral glioma. Neuro Oncol 15:635–643
Sinclair S, Norris JM, McConnell SJ, Chochinov HM, Hack TF et al (2016) Compassion: a scoping review of the healthcare literature. BMC Palliat Care 15:6
Tanco K, Rhondali W, Perez-Cruz P, Tanzi S, Chisholm GB et al (2015) Patient perception of physician compassion after a more optimistic vs. a less optimistic message: a randomized clinical trial. JAMA Oncol 1:176–183
Faller H, Weis J, Koch U, Brahler E, Harter M et al (2016) Perceived need for psychosocial support depending on emotional distress and mental comorbidity in men and women with cancer. J Psychosom Res 81:24–30
Rooney AG, van Nieuwenhuizen D, Reijneveld JC, Grant R (2009) Female gender is not a proven risk factor for depression in glioma. J Neurooncol 95:449
Quinten C, Coens C, Ghislain I, Zikos E, Sprangers MA et al (2015) The effects of age on health-related quality of life in cancer populations: a pooled analysis of randomized controlled trials using the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 involving 6024 cancer patients. Eur J Cancer 51:2808–2819
Boele FW, Klein M, Reijneveld JC, Verdonck-de Leeuw IM, Heimans JJ (2014) Symptom management and quality of life in glioma patients. CNS Oncol 3:37–47
Peters KB, West MJ, Hornsby WE, Waner E, Coan AD et al (2014) Impact of health-related quality of life and fatigue on survival of recurrent high-grade glioma patients. J Neurooncol 120:499–506
Acknowledgements
We acknowledge all further members of our study group—Monika Deininger, Markus Haug, Sonja Grüninger, Linda Stöckelmaier, Katrin Nickel and Güler Savas—for their tremendous support. This work contains parts of the dissertation of Mareile Janko and Karoline Kohlmann.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest and no disclosures.
Ethical approval
The study was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Renovanz, M., Hechtner, M., Janko, M. et al. Factors associated with supportive care needs in glioma patients in the neuro-oncological outpatient setting. J Neurooncol 133, 653–662 (2017). https://doi.org/10.1007/s11060-017-2484-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2484-y