Abstract
In a selected patient population, we evaluated the glycemic response to different infusional policies in the management of posterior cranial fossa tumor (PFT) removal. We analyzed the perioperative course, prospectically collected, of 137 children undergoing 150 surgical procedures. Patients were divided in two groups according to different intraoperative fluids (group A, 2.5% glucose; group B, crystalloids). In group B glycemia remained below 125 mg dl−1, while group A showed persistently supranormal glycemic plasma values, reaching statistical significance at the end of surgery (P < 0.018). As no perioperative mortality occurred and no differences were found between groups regarding PICU respiratory or infectious complications, PICU length of stay (LOS) was assumed as the main outcome indicator. LOS was not influenced by group A or B inclusion, while a new indicator, namely the Glycemic Stress Index (GSI), representing both glycemic intraoperative change and procedure length, showed significantly different results in the study groups (P = 0.004). Our clinical experience suggests that both intraoperative glucose-free solutions are safe, and GSI can be a useful tool to identify prolonged PICU stay patients.
Similar content being viewed by others
Introduction
It has been appreciated for over a century that severe illness is associated with hyperglycemia. However, for most of that time, “stress hyperglycemia” has been either largely ignored or assumed to be adaptive. It is now well established that both the degree and the duration of hyperglycemia are independent risk factors for adverse outcome [1–3].
Although similar studies have rarely been published in the pediatric population, critically ill infants and children may benefit from glycemic control during the perioperative period. To date, few studies have been published investigating blood glucose trends in pediatrics throughout critical illness. Available data suggest that pediatric patients are at risk of becoming hyperglycemic when undergoing physiologic stress and therefore may be exposed to similar risks as adult patients [4, 5]. According to these findings, it seems reasonable to make every effort to control glucose plasma levels during major surgical procedures, especially in the neurosurgical setting, due to the possible correlation between hyperglycemia and poor outcome. The infusional policies should be considered the cornerstone of this strategy. As 5% dextrose solutions are associated with hyperglycemia [6, 7], solutions with a lower glucose concentrations (from 2.5% to 0.9%) have been evaluated [8–10]. However, one of the major obstacles encountered in designing a pediatric intervention trial for tight glycemic control is the concern about hypoglycemia due to the reduced glycogen reserve, especially in the setting of physiologic stress [11].
Our aim was to evaluate the glycemic response to two different infusional policies in the critical care management of a selected population of children (with posterior cranial fossa tumors, PFT). We also proposed a new scoring system related to glycemic stress called the Glycemic Stress Index (GSI).
Materials and methods
From January 1993 to December 2003, 137 children (69 males, 68 females) aged from 1 to 194 months underwent 150 surgical procedures for infratentorial tumor resection at the Catholic University Medical School, Rome, Italy. Throughout the time period, the surgical goal was the most extensive tumor resection with the best possible neurological outcome.
All patients were admitted to the PICU in the postoperative period. The main patient data are shown in Table 1. Forty children (group A) received 2.5% glucose in balanced electrolyte solution, while 110 patients (group B) were given only saline solutions intraoperatively. Both groups received 5% glucose solution in saline after PICU admission. Thirty-six children (22 males, 14 females) were transfused with homologous packed red blood cells (PRBC) intraoperatively and 2 postoperatively. The following laboratory variables, glucose, Na, Ht, Hb, pH, BE and NaHCO3, were recorded before surgery (T0), at dural closure (T1), at PICU admission (T2) and 24 h after surgery (T3). Histopathology, tumor location and the number of procedures for each patient were also collected.
Normoglycemia (<110 mg dl−1), reduced tolerance to glucose (110–125 mg dl−1), hyperglycemia (>125 mg dl−1) and hypoglycemia (<50 mg dl−1 in infants, <60 mg dl−1 in children over 12 months) levels were established according to National Diabetes Data Group and WHO criteria [12].
The two groups were homogeneous for age, sex, weight, steroid treatment, rate of fluid intake (intra- and postoperative) and duration of surgery (Table 1). The review of the medical records was approved by the institutional Ethical Committee.
Anesthesia management
General anesthesia was induced through a face mask with sevoflurane or halothane and O2 in non-cooperative patients and by means of thiopentone (3–4 mg kg−1) or propofol (2 mg kg−1) in the older children. Two cannulas were positioned into large-size peripheral veins (large saphenous venous if possible) together with a central venous line (G 18/20/22 depending on patient age) in the internal jugular vein. Since 2001, central venous access has been achieved through echo-guided procedures. Intraoperative monitoring consisted of:
-
Heart rate (HR)
-
Invasive arterial blood pressure (IABP)
-
Central venous pressure (CVP)
-
Superior vena cava mixed venous saturation (SVCSVO2)
-
Pulse-oximetry (SpO2)
-
End tidal halogenated agents (EtHA)
-
End tidal carbon dioxide (EtCO2)
-
Spirometry
-
Peripheral and core temperature
-
Urine output
-
Acid–base status, Hb/Hct/Plt, serial determinations
Body temperature was maintained by a hot air warming mattress; fluid infusions were warmed by a thermostatic system. Muscle relaxation was obtained by vecuronium bromide (0.07 mg kg−1) or cisatracurium (0.1 mg kg−1 bolus, 2 μg kg−1 min−1 continuous infusion). Endotracheal intubation was executed using cuffed tracheal tubes. General anesthesia was maintained by isoflurane (MAC 1) and fentanyl (1–3 μg−1 kg−1 h−1 according to patient status), while ventilation was performed through Servo Ventilator 900 C (Siemens Elema, Sweden) on the volume-controlled mode.
Fluid balance and blood loss management
Fluid balance was maintained with crystalloids at the rate of 4 ml kg−1 h−1 until dura opening, then 8–10 ml kg−1 h−1 subsequently. Intraoperatively warmed fluids were infused by means of volumetric pumps (Abbott). Until 1996, balanced electrolyte solutions with 5% glucose were infused [Normosol R with glucose 5% (50% of fluid intake) plus Normosol R without glucose for the remaining 50%] to provide appropriate total glucose requirements for healthy children (group A) (6]; since 1997, glucose solutions have not been infused during surgery due to a different policy of intraoperative fluid management (group B).
For all patients we estimated EBV according to the following formula: K * Body Weight (BW) where K is a factor depending on age (80 ml in infants, 75 in children under 3 years, 70 in patients over 3 years, 65 in obese patients). Intraoperative red cell volume loss was calculated according to the Kearney formula: ERCMloss = ERCMi − ERCMe + ERCMtrasf where i is before surgery, e is end of surgery, and transf is red cell volume transfused [13]. We also determined ERCM loss ratio (i.e., ERCMloss/ERCMi * 100).
During surgery, blood loss was calculated, on the basis of estimated red cell volume, by serial measurements of Hct [14], provided a constant central venous pressure was maintained. Vital signs, monitoring systems and laboratory data, such as IABP, CVP, SpO2, EtCO2, core and peripheral temperature, urine output, serum osmolality, acid–base status and serum proteins, were also considered to clinically assess the volemic status of the patient. Intraoperatively, according to international guidelines on blood loss [15], clotting function was controlled when the EBL was more than 70% of the EBV, while a control of coagulative parameters was performed anyway at the end of surgery.
Restoration of volemia was achieved with colloid infusions (Hemacell® or starches at the maximum IO rate of 15–20 ml kg−1, then 5% human albumin).
Intraoperatively, when bleeding was ongoing, the minimum acceptable Hct of the patient was 21% (postoperatively 18% on stable cardiorespiratory status). When necessary, PBRCs were transfused to restore Hct or when signs of inadequate O2 tissue delivery appeared (metabolic acidosis, lactic acidosis with hemodynamic instability). In the postoperative period, we continued a careful monitoring of fluid balance and blood loss during the following 72 h.
The patients were transferred to the pediatric neurosurgery ward according to an institutional PICU discharge protocol (i.e., when hemodynamic parameters, metabolic conditions and neurological status were stable for at least 8 h). No transferred patient was re-admitted to the PICU in the first 7 days after discharge.
Statistical analysis
All data were analyzed with SPSS for Windows rel. 13.0 (SPSS Inc., Chicago, IL), and P-values < 0.05 were considered statistically significant. Proportions were compared by χ2 test or Fisher’s exact test where appropriate. Normal distribution of data was primarily tested with Kolmogorov–Smirnov test, then continuous variables were contrasted by the Mann–Whitney U-test or the Student's t-test, as appropriate.
Variables that were significantly different between the two study groups at the univariate analysis were used to derive a new index, the “Glycemic Stress Index,” which is proposed as an indicator of the perioperative metabolic stress, calculated as follows:
To analyze the association with PICU LOS, the index was analyzed with multiple linear regression, using the backward-stepwise technique. Factors included in the model were patient age, weight, sex and tumor site. GSI was then subjected to receiver-operator characteristics (ROC) analysis to study the index reliability for predicting PICU stay. The threshold of 200 h was selected as a cutoff for the ROC analysis because of our PICU length of stay (considering the mean stay and its standard deviation, the majority of patients had a PICU stay <190 h).
Results
Baseline characteristics of the study population are shown in Table 1. Transfusion rate and blood loss were similar in the two groups (P > 0.11 and P > 0.707, respectively), as was for other demographic and clinical variables. Following PICU admission, no differences were recorded regarding infectious or metabolic complications and time on ventilator.
Table 2 shows the glycemic trends of groups A and B recorded at selected time points [i.e., baseline (T0), at dural closure (T1), on PICU admission (T2) and at 24 h after surgery (T3), respectively]. Although group A glucose plasma levels resulted in being higher at all time points (Figs. 1, 2, 3), the only statistically significant difference was recorded at dural closure (P = 0.018). Of note, group B glucose plasma levels remained below 125 mg dl−1 throughout the whole treatment period. On the contrary, group A patients showed abnormal glycemia values both at T1 and T2: in fact, 57% and 60% of group A patients showed glycemic levels higher than 125 mg% at T1 and T2, respectively, while in group B (no glucose patients) only 28% and 38% of the patients were above this threshold (Figs. 1, 2).
The no-glucose strategy also resulted in being safe, avoiding dangerous hypoglycemic drops: Figures 1 and 2 illustrate the distribution of individual glucose plasma levels of groups A and B patients at T1 and T2, respectively. Interestingly, no patients who did not receive glucose infusions during surgery showed glycemic values below the hypoglycemic threshold (60 mg dl−1). Intraoperative glucose levels have not been systematically checked out, though patients had intraoperative glucose determinations (as glucose level is determined simultaneously with arterial gas analysis and electrolytes). Moreover, upon careful examination of anesthesiological records, no intraoperative hypoglycemic episodes were registered, and no hypertonic glucose was needed intraoperatively. The median intraoperative glucose level for group A and group B is 108 and 105 mg dl−1, respectively. A global comparison of glycemic values between groups has been added in Fig. 3.
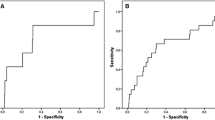
As in our study population, no intraoperative or early/late postoperative mortality occurred (within the first week and 7–30 days after surgery, respectively), and no respiratory or infectious complications (two patients in group A vs. five patients in group B, P = 0.899); the PICU LOS was assumed to be the main outcome indicator. LOS was not influenced significantly by the simple group A or B inclusion (Table 1). We then identified a new index—called the Glycemic Stress Index (GSI)—describing the intraoperative glycemic variation corrected by the duration of surgery. This index was significantly different between the two study groups (A: 6.1 ± 3.2 vs. B: 4.7 ± 2.4; P = 0.004): on multiple linear regression analysis, PICU LOS was significantly influenced by GSI (st. β coefficient: 0.25, P = 0.022), while patient age, body weight, sex, blood loss and tumor location were not significant.
Figure 4 illustrates GSI performance for predicting PICU stay over 200 h. Reliability of such ROC analysis is statistically significant (AUC = 0.792; P = 0.016); all patients with a GSI >4.11 had a PICU LOS longer than 200 h (sensitivity 100%, specificity 35%). Figure 5 illustrates GSI performance for predicting PICU stay over 200 h in groups A (AUC = 0.790) and B (AUC = 0.721), respectively.
Discussion and conclusions
This study demonstrates that the no-glucose strategy allows the maintenance of normal glucose plasma levels in children undergoing PFT surgery, avoiding dangerous hypoglycemic episodes. The comparison with the previous low-glucose strategy showed clinically different glycemic trends in our patients. By taking into account also the duration of surgery, we proposed a new index, the GSI, for the metabolic evaluation of our patient population. The GSI was a significant predictor of the postoperative intensive care need, expressed as PICU LOS.
Glucose requirements in pediatric patients have been reassessed recently with consideration of the hazards of both hyperglycemia and hypoglycemia, and the changes of glucose levels during surgery. The prevalence of hyperglycemia in the PICU varies from 17% to 75% within the first 10 days of admission, and a threefold increase in mortality over matched euglycemic controls and a longer length of stay was identified [12]. However, in the pediatric population it may have different effects on morbidity or mortality compared with adults as a consequence of different metabolic demands, comorbid conditions or age dependence [16].
A proinflammatory effect of hyperglycemia has been recently postulated [17]; this may be relevant in critically ill children, yet affected by proinflammatory events, such as intracranial surgery and significant blood transfusion, as in our setting.
The uncertainty regarding acceptable age-related norms for euglycemia in critically ill children may cause reluctance to accept strict glucose control, with the potential for complications related to hypoglycemia being highest in children 3–5 years old [5].
Data from neurotrauma studies in adults revealed that hyperglycemia markedly influences the clinical outcome [18, 19], as was the case for experimental ischemic/anoxic models [19]. Hyperglycemia is also known to exacerbate ischemic neurologic injury [19–21], as demonstrated for SAH patients [22, 23]. An association between poor outcome and hyperglycemia has been proposed also in pediatric neurotrauma patients [24].
As hyperglycemia should be considered harmful in brain damage from all causes, every effort should be made to control glucose plasma levels during invasive neurosurgical procedures. Our data are in agreement with the Leelanukrom statement against unnecessary glucose administration in patients at risk of hypoxic–ischemic episodes, since hyperglycemia can worsen the neurological outcome and hyperglycemia per se may cause cerebral damage [25]. The exact mechanisms of such neurological deterioration are not clearly defined; intracellular acidosis caused by increased tissue lactate concentration and anaerobic glycolysis has been proposed. Interestingly, in our experience, a significant increase in arterial BE was observed only in group A children (Table 1). A threshold value of 180–216 mg dl−1 of pre-ischemic plasma glucose has been suggested experimentally [26] and 125–140 mg dl−1 in the clinical practice [27–29].
However, the risk of hypoglycemia resulting from perioperative starvation has been extensively studied since the early 1970s with conflicting results. Hypoglycemic events can be difficult to detect under anesthesia and can produce severe brain damage if not corrected in a timely manner, mostly in the developing child [30].
The incidence of hypoglycemia at the beginning of surgery has been estimated at 0.5–2%, excluding neonates and premature babies [6, 8, 31], increasing to 31% in children below the third percentile body weight [32]. As shorter preoperative fasting periods are now recommended, hypoglycemia now may be less common than previously. Notwithstanding, most pediatric anesthesiologists continue to administer glucose, even if its amount has been dramatically reduced since the 1990s. As 5% dextrose solutions can be associated with hyperglycemia [6, 7], lower glucose concentration solutions (from 2.5% to 0.9%) have been introduced following some convincing clinical trials [8–10].
However, in the present study, also children receiving 2.5% dextrose solutions (group A) showed a statistically significant increase in the glucose plasma level at T1 (P > 0.018, Table 2) and similar trends at other time points, if compared with group B (no glucose). The different setting of our study should be considered, in comparison with previous experiences focused on minor, non-hemorrhagic surgical procedures [8–10]. As a consequence, our patient population—representing a very homogenous sample—is quite different and not fully comparable. Another major point is that we never detected hypoglycemia in group B patients throughout the whole perioperative period (Figs. 1, 2]. However, at dural closure only 28% of group B patients were above 125 mg dl−1 versus 57% of glucose-receiving patients.
Blood products contain glucose in the preservative solution (270/360 mg dl−1 of PRBC); consequently, they represent an exogenous source of glucose supply, leading to increased glycemia in transfused patients [33, 34]. In our patient population, groups A and B were not statistically different regarding the transfusion rate and ERCM-loss ratio, a reliable marker of blood loss (Table 1).
Given the short postoperative PICU course, the absence of other hyperglycemia-related side effects (e.g., infections, metabolic derangements) is not surprising. A major finding of our study is that the glycemic increase (over a period of surgical stress), not the glycemic level per se, is relevant [5] and appears to influence the PICU stay. In fact, even if the PICU LOS was not different between groups, it appears strongly related to GSI, which significantly varied between patients receiving glucose or not. We could determine a cutoff value for this indicator, predicting a PICULOS > 200 h, suggesting that GSI could be useful to individuate patients at higher risk for prolonged PICU LOS (Figs. 4, 5). Since group A received 2.5% glucose, showing higher serum glucose levels, and was treated earlier than group B, the ROC curve might merely represent the difference in timing, and the GSI an association phenomenon. To eliminate this potential bias, and to demonstrate that GSI is a viable concept, we separate ROC curves within each group, thus eliminating the influence of a timing effect. Anyway, AUC values are very similar both if we consider the whole study population or the two groups according to infusion policy.
This study has some limitations that need to be addressed: first of all, it is a retrospective analysis of prospectically collected data; however, it is important to note that, as already mentioned, we considered a very homogenous population. Moreover, we did not evaluate other metabolic data, such as lipid mobilization during prolonged surgery [7, 10], this being a matter of ongoing studies based on indirect calorimetry. Thus, we cannot suggest to extend our findings to longer neurosurgical procedures—lasting >6 h—because, in the absence of data coming from a specific study, we cannot exclude the risk of intraoperative hypoglycemia.
In fact, GSI efficaciously represents the intraoperative dynamic glycemic variation, not glycemic fluctuations. This will be accomplished by multiple—or even continuous—glucose determinations [35]. Another main point is that an association between two variables (GSI and PICU-LOS) does not automatically mean a causal relationship, while future wider randomized studies are warranted to better define the role of other glycemic parameters and to clarify a possible causal relationship between glycemia and PICU stay.
In conclusion, the results of our study suggest that an intraoperative infusion of glucose-free balanced solution is safe in pediatric neurosurgical patients, as it allows maintaining blood glucose levels within normal range and does not expose the children to a significant risk of hypoglycemia. GSI can be a useful tool to identify patients who will have prolonged PICU stays.
Abbreviations
- BE:
-
Base excess
- BW:
-
Body weight
- CVP:
-
Central venous pressure
- EBL:
-
Estimated blood loss
- EBV:
-
Estimated blood volume
- ERCM:
-
Estimated red cell mass
- ERCMf :
-
Endoperative estimated red cell mass
- ERCMi :
-
Preoperative estimated red cell mass
- ERCMloss :
-
Estimated red cell mass loss
- ERCMtrasf :
-
Estimated red cell mass transfused
- EtCO2 :
-
End tidal carbon dioxide
- EtHA:
-
End tidal halogenated agents
- GSI:
-
Glycemic Stress Index
- Hb:
-
Hemoglobin
- Hct:
-
Hematocrit
- HR:
-
Heart rate
- IABP:
-
Invasive arterial blood pressure
- ICU:
-
Intensive care unit
- LOS:
-
Length of stay
- MAC:
-
Minimum alveolar concentration
- Na:
-
Sodium
- NaHCO3 :
-
Sodium bicarbonate
- PFT:
-
Posterior cranial fossa tumor
- PICU:
-
Pediatric intensive care unit
- PRBC:
-
Packed red blood cells
- SAH:
-
Sub-arachnoid hemorrhage
- SpO2 :
-
Pulse-oximetry
- SVCSVO2 :
-
Superior vena cava mixed venous saturation
- TBI:
-
Traumatic brain injury
- WHO:
-
World Health Organization
References
Krinsley JS (2003) Association between hyperglycemia and increased hospital mortality in a heterogenous population of critically ill patients. Mayo Clin Proc 78(12):1471–1478
Lam AM, Winn HR, Cullen BF et al (1991) Hyperglycemia and neurological outcome in patients with head injury. J Neurosurg 75(4):545–551
Van den Berghe G, Wilmer A, Hermans G et al (2006) Intensive insulin therapy in the medical ICU. N Engl J Med 354(5):449–461. doi:10.1056/NEJMoa052521
Srinivasan V, Spinella P, Drott HR et al (2004) Association of timing, duration and intensity of hyperglycemia with intensive care unit mortality in critically ill children. Pediatr Crit Care Med 5(4):329–336. doi:10.1097/01.PCC.0000128607.68261.7C
Klein JW, Hojsak JM, Rapaport R (2007) Hyperglycemia in the pediatric intensive care unit. Curr Opin Clin Nutr Metab Care 10(2):187–192. doi:10.1097/MCO.0b013e3280147d3e
Welborn LG, Hannallah RS, MGill WA (1987) Glucose concentrations for routine intravenous infusion in pediatric outpatient surgery. Anesthesiology 67(3):427–430. doi:10.1097/00000542-198709000-00027
Mikawa K, Maekawa N, Goto R et al (1991) Effects of exogenous intravenous glucose on plasma glucose and lipid homeostasis in anesthetized children. Anesthesiology 74:1017–1022. doi:10.1097/00000542-199106000-00008
Hongnat JM, Murat I, Saint-Maurice C (1991) Evaluation of current paediatric guidelines for fluid therapy using two different dextrose hydrating solutions. Pediatr Anesth 1(2):95–100. doi:10.1111/j.1460-9592.1991.tb00018.x
Dubois M, Gouyet I, Murat I (1992) Lactated Ringer with 1% dextrose: an appropriate solution for perioperative fluid therapy in children. Pediatr Anesth 2(2):99–104. doi:10.1111/j.1460-9592.1992.tb00183.x
Nishina K, Mikawa K, Maekawa N et al (1995) Effect of exogenous intravenous glucose on plasma glucose and lipid homeostasis in anesthetized infants. Anesthesiology 83(2):258–263. doi:10.1097/00000542-199508000-00004
Jaksic T (2002) Effective and efficient nutritional support for the injured child. Surg Clin North Am 82(2):379–391. doi:10.1016/S0039-6109(02)00005-1
American Diabetes Association (2000) Supplement 1. American Diabetes Association: clinical practice recommendations 2000. Diabetes Care 23(Suppl 1):S4–S19
Kearney RA, Rosales JK, Howes WJ (1989) Craniosynostosis: an assessment of blood loss and transfusion practices. Can J Anaesth 36(4):473–477
Faberowski LW, Black S, Mickle JP (1999) Blood loss and transfusion practice in the perioperative management of craniosynostosis repair. J Neurosurg Anesthesiol 11(3):167–172. doi:10.1097/00008506-199907000-00002
British Committee for Standards in Haematology, Blood Transfusion Task Force (J Duguid, Chairman) (2004) Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol 126(1):11–28. doi:10.1111/j.1365-2141.2004.04972.x
Faustino EV, Apkon M (2005) Persistent hyperglycemia in critically ill children. J Pediatr 146(1):30–34. doi:10.1016/j.jpeds.2004.08.076
Blondet JJ, Beilman GJ (2007) Glycemic control and prevention of perioperative infection. Curr Opin Crit Care 13(4):421–427. doi:10.1097/MCC.0b013e32826388a1
Rovlias A, Kotsou S (2000) The influence of hyperglycemia on neurological outcome in patients with severe head injury. Neurosurgery 46(2):335–342. doi:10.1097/00006123-200002000-00015
Wass CT, Lanier WL (1996) Glucose modulation of ischemic brain injury: review and clinical recommendations. Mayo Clin Proc 71(8):801–812
Van den Berghe G, Schoonheydt K, Becx P et al (2005) Insulin therapy protects the central and peripheral nervous system of intensive care patients. Neurology 64(8):1348–1352
Fukuda S, Warner DS (2007) Cerebral protection. Br J Anaesth 99(1):10–17. doi:10.1093/bja/aem140
Sato M, Nakano M, Asari J et al (2006) Admission blood glucose levels and early change of neurological grade in poor-grade patients with aneurismal subarachnoid haemorrhage. Acta Neurochir (Wien) 148(6):623–626. doi:10.1007/s00701-005-0717-x
Frontera JA, Fernandez A, Claassen J et al (2006) Hyperglycemia after SAH: predictors, associated complications, and impact on outcome. Stroke 37(1):199–203. doi:10.1161/01.STR.0000194960.73883.0f
Cochran A, Scaife ER, Hansen KW et al (2003) Hyperglycemia and outcomes from pediatric traumatic brain injury. J Trauma 55(6):1035–1038. doi:10.1097/01.TA.0000031175.96507.48
Leelanukrom R, Cunliffe M (2000) Intraoperative fluid and glucose management in children. Pediatr Anesth 10:353–359. doi:10.1046/j.1460-9592.2000.00536.x
Li PA, Siesjo BK (1997) Role of hyperglycaemia-related acidosis in ischaemic brain damage. Acta Physiol Scand 161:567–580. doi:10.1046/j.1365-201X.1997.00264.x
Bilotta F, Spinelli A, Giovannini F et al (2007) The effect of intensive insulin therapy on infection rate, vasospasm, neurologic outcome, and mortality in neurointensive care unit after intracranial aneurysm clipping in patients with acute subarachnoid hemorrhage: a randomized prospective pilot trial. J Neurosurg Anesthesiol 19(3):156–160. doi:10.1097/ANA.0b013e3180338e69
Badjatia N, Topcuoglu MA, Buonanno FS et al (2005) Relationship between hyperglycemia and symptomatic vasospasm after subarachnoid hemorrhage. Crit Care Med 33(7):1603–1609. doi:10.1097/01.CCM.0000168054.60538.2B
Dorhout Mees SM, van Dijk GW, Algra A et al (2003) Glucose level and outcome after subarachnoid hemorrhage. Neurology 61(8):1132–1133
Cornblath M, Hawdon JM, Williams AF et al (2000) Controversies regarding definition of neonatal hypoglycemia: suggested operational thresholds. Pediatrics 105(5):1141–1145. doi:10.1542/peds.105.5.1141
Jensen BH, Wernberg M, Andersen M (1982) Preoperative starvation and blood glucose concentrations in children undergoing inpatient and outpatient anaesthesia. Br J Anaesth 54:1071–1074. doi:10.1093/bja/54.10.1071
Payne K, Ireland P (1984) Plasma glucose level in the peri-operative period in children. Anaesthesia 39:868–872. doi:10.1111/j.1365-2044.1984.tb06572.x
Wolf AR, Eyres RL, Laussen PC et al (1993) Effect of extradural analgesia on stress responses to abdominal surgery in children. Br J Anaesth 70:654–660. doi:10.1093/bja/70.6.654
Moylan S, Collee G, Mackersie A et al (1993) Anaesthetic management in paediatric craniofacial surgery. A review of 126 cases. Pediatr Anesth 3:275–281. doi:10.1111/j.1460-9592.1993.tb00086.x
Nielsen JK, Djurhuus CB, Gravholt CH, Carus AC, Granild-Jensen J, Orskov H, Christiansen JS (2005) Continuous glucose monitoring in interstitial subcutaneous adipose tissue and skeletal muscle reflects excursions in cerebral cortex. Diabetes 54(6):1635–1639. doi:10.2337/diabetes.54.6.1635
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pietrini, D., Di Rocco, C., Di Bartolomeo, R. et al. No-glucose strategy influences posterior cranial fossa tumors' postoperative course: introducing the Glycemic Stress Index. J Neurooncol 93, 361–368 (2009). https://doi.org/10.1007/s11060-008-9784-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9784-1