Abstract
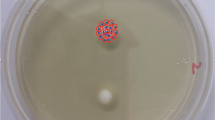
This study aimed to evaluate the effects of cold atmospheric pressure plasma (CAPP) jet on Trichophyton rubrum growth, germination and adherence to nail. The effects of plasma jet on T. rubrum conidia germination and on mycelial growth were evaluated by in vitro assays. An ex vivo nail infection model was used to evaluate the effects on conidia adherence and infection. Biochemical analyses of nail fragments exposed or not to CAPP were performed by attenuated total reflectance–Fourier transform infrared (ATR–FTIR) spectroscopy. Plasma jet exposure for 10 and 15 min completely inhibited mycelial growth after only one exposure. Fifteen minutes of exposure could reduce conidia germination in suspension. Fungal suspensions exposed to plasma jet for 10 and 15 min were not able to infect nail specimens. These results were corroborated by ATR–FTIR analyses of nail fragments. In conclusion, single exposure to CAPP for 15 min was able to inhibit fungal growth, adherence and infection capacity. The results suggest that cold atmospheric plasma jet can be a promising alternative for the treatment of onychomycoses caused by T. rubrum.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.






Similar content being viewed by others
References
Faway É, Lambert de Rouvroit C, Poumay Y. In vitro models of dermatophyte infection to investigate epidermal barrier alterations. Exp Dermatol. 2018;27(8):915–22.
Asz-Sigall D, Tosti A, Arenas R. Tinea unguium: diagnosis and treatment in practice. Mycopathologia. 2017;182(1–2):95–100.
Chabasse D, Pihet M. Onychomycoses due to molds. J Mycol Med. 2014;24(4):261–8.
Gupta AK, Versteeg SG, Shear NH, Piguet V, Tosti A, Piraccini BM. A practical guide to curing onychomycosis: how to maximize cure at the patient, organism, treatment, and environmental level. Am J Clin Dermatol. 2019;20(1):123–33.
Nenoff P, Krüger C, Ginter-Hanselmayer G, Tietz HJ. Mycology—an update. Part 1: dermatomycoses: causative agents, epidemiology and pathogenesis. J Dtsch Dermatol Ges. 2014;12(3):188–209; quiz 10, 188–211; quiz 2.
Rouzaud C, Hay R, Chosidow O, Dupin N, Puel A, Lortholary O, et al. Severe dermatophytosis and acquired or innate immunodeficiency: a review. J Fungi (Basel). 2015;2(1):4.
Dogra S, Narang T. Emerging atypical and unusual presentations of dermatophytosis in India. Clin Dermatol Rev. 2017;1(3):12–8.
Zhan P, Liu W. The changing face of dermatophytic infections worldwide. Mycopathologia. 2017;182(1–2):77–86.
Sei Y. 2011 epidemiological survey of dermatomycoses in Japan. Med Mycol J. 2015;56(4):J129–35.
Silva LB, de Oliveira DB, da Silva BV, de Souza RA, da Silva PR, Ferreira-Paim K, et al. Identification and antifungal susceptibility of fungi isolated from dermatomycoses. J Eur Acad Dermatol Venereol. 2014;28(5):633–40.
Khan Z, Ahmad S, Alfouzan W, Joseph L, Varghese S. Demonstration of adventitious sporulation in Fusarium petroliphilum onychomycosis. Mycopathologia. 2019;184(2):303–8.
Gupta AK, Versteeg SG, Shear NH, Piguet V, Tosti A, Piraccini BM. A practical guide to curing onychomycosis: how to maximize cure at the patient, organism, treatment, and environmental level. Am J Clin Dermatol. 2019;20(1):123–33.
Angora KE, Ira-Bonouman A, Vanga-Bosson AH, Konaté A, Kassi FK, Tuo K, et al. Clinical and mycological characteristics of onychomycosis due to Candida at Institut Pasteur of Côte d’Ivoire. J Mycol Med. 2018;28(1):167–72.
Lipner SR. Pharmacotherapy for onychomycosis: new and emerging treatments. Expert Opin Pharmacother. 2019;20(6):725–35.
Iwanaga T, Ushigami T, Anzawa K, Mochizuki T. Pathogenic dermatophytes survive in nail lesions during oral terbinafine treatment for Tinea unguium. Mycopathologia. 2017;182(7–8):673–9.
Laroussi M. Plasma medicine: a brief introduction. Plasma. 2018;1(1):5.
Schröter S, Wijaikhum A, Gibson AR, West A, Davies HL, Minesi N, et al. Chemical kinetics in an atmospheric pressure helium plasma containing humidity. Phys Chem Chem Phys. 2018;20(37):24263–86.
Nishime TMC, Borges AC, Koga-Ito CY, Machida M, Hein LRO, Kostov KG. Non-thermal atmospheric pressure plasma jet applied to inactivation of different microorganisms. Surf Coat Technol. 2017;312:19–24.
Weltmann K-D, von Woedtke T. Plasma medicine—current state of research and medical application. Plasma Phys Control Fusion. 2017;59(1):14031.
Brun P, Bernabè G, Marchiori C, Scarpa M, Zuin M, Cavazzana R, et al. Antibacterial efficacy and mechanisms of action of low power atmospheric pressure cold plasma: membrane permeability, biofilm penetration and antimicrobial sensitization. J Appl Microbiol. 2018;125(2):398–408.
Borges AC, Nishime TMC, Kostov KG, Lima GDMG, Gontijo AVL, de Carvalho JNMM, et al. Cold atmospheric pressure plasma jet modulates Candida albicans virulence traits. Clin Plasma Med. 2017;7–8:9–15.
Borges AC, Lima GMG, Nishime TMC, Gontijo AVL, Kostov KG, Koga-Ito CY. Amplitude-modulated cold atmospheric pressure plasma jet for treatment of oral candidiasis: in vivo study. PLoS One. 2018;13(6):e0199832.
Heinlin J, Maisch T, Zimmermann JL, Shimizu T, Holzmann T, Simon M, et al. Contact-free inactivation of Trichophyton rubrum and Microsporum canis by cold atmospheric plasma treatment. Future Microbiol. 2013;8(9):1097–106.
Scholtz V, Soušková H, Hubka V, Švarcová M, Julák J. Inactivation of human pathogenic dermatophytes by non-thermal plasma. J Microbiol Methods. 2015;119:53–8.
Shapourzadeh A, Rahimi-Verki N, Atyabi SM, Shams-Ghahfarokhi M, Jahanshiri Z, Irani S, et al. Inhibitory effects of cold atmospheric plasma on the growth, ergosterol biosynthesis, and keratinase activity in Trichophyton rubrum. Arch Biochem Biophys. 2016;608:27–33.
Pereira FO, Mendes JM, Lima IO, Mota KS, Oliveira WA, Lima EEO. Antifungal activity of geraniol and citronellol, two monoterpenes alcohols, against Trichophyton rubrum involves inhibition of ergosterol biosynthesis. Pharm Biol. 2015;53(2):228–34.
Klämpfl TG, Isbary G, Shimizu T, Li YF, Zimmermann JL, Stolz W, et al. Cold atmospheric air plasma sterilization against spores and other microorganisms of clinical interest. Appl Environ Microbiol. 2012;78(15):5077–82.
Youssef AB, Kallel A, Azaiz Z, Jemel S, Bada N, Chouchen A, et al. Onychomycosis: which fungal species are involved? Experience of the laboratory of parasitology–mycology of the rabta hospital of Tunis. J Mycol Med. 2018;28(4):651–4.
Tachibana H, Kumagai N, Tatsumi Y. Fungicidal activity in the presence of keratin as an important factor contributing to in vivo efficacy: a comparison of efinaconazole, tavaborole, and ciclopirox. J Fungi (Basel). 2017;3(4):58.
Lin X, Alspaugh JA, Liu H, Harris S. Fungal morphogenesis. Cold Spring Harb Perspect Med. 2014;5(2):a019679.
Tainwala R, Sharma Y. Pathogenesis of dermatophytoses. Indian J Dermatol. 2011;56(3):259–61.
Gupta BS, Jelle B, Gao T. Application of ATR–FTIR spectroscopy to compare the cell materials of wood decay fungi with wood mould fungi. Int J Spectrosc. 2015;2015:7.
De Bruyne S, Speeckaert R, Boelens J, Hayette MP, Speeckaert M, Delanghe J. Infrared spectroscopy as a novel tool to diagnose onychomycosis. Br J Dermatol. 2019;180(3):637–46.
Sowa MG, Wang J, Schultz CP, Ahmed MK, Mantsch HH. Infrared spectroscopic investigation of in vivo and ex vivo human nails. Vib Spectrosc. 1995;10(1):49–56.
Farhan KM, Sastry TP, Mandal AB. Comparative study on secondary structural changes in diabetic and non-diabetic human finger nail specimen by using FTIR spectra. Clin Chim Acta. 2011;412(3–4):386–9.
Bitencourt TA, Macedo C, Franco ME, Assis AF, Komoto TT, Stehling EG, et al. Transcription profile of Trichophyton rubrum conidia grown on keratin reveals the induction of an adhesin-like protein gene with a tandem repeat pattern. BMC Genom. 2016;17:249.
Szeghalmi A, Kaminskyj S, Gough KM. A synchrotron FTIR microspectroscopy investigation of fungal hyphae grown under optimal and stressed conditions. Anal Bioanal Chem. 2007;387(5):1779–89.
Costa-Orlandi CB, Sardi JC, Santos CT, Fusco-Almeida AM, Mendes-Giannini MJ. In vitro characterization of Trichophyton rubrum and T. mentagrophytes biofilms. Biofouling. 2014;30(6):719–27.
Scholtz V, Soušková H, Švarcová M, Kríha V, Živná H, Julák J. Inactivation of dermatophyte infection by nonthermal plasma on animal model. Med Mycol. 2017;55(4):422–8.
Acknowledgements
Authors are greatful to São Paulo Research Foundation (FAPESP) for the financial support: Grants #2016/07196-6 (CY Koga-Ito); #2015/21989-6 (KG Kostov) and fellowship #2014/02354-7 (AC Borges).
Author information
Authors and Affiliations
Contributions
ACB and TMCN performed experiments, analyzed data and wrote the paper. GDMGL analyzed data. SDMR performed experiments and analyzed data. KGK designed the study and wrote the paper. GPT carried out FTIR analyses and revised the paper. BRCDM performed FTIR analyses. JPBM conducted SEM analyses. CYK designed the study and wrote the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Handling Editor: Vishnu Chaturvedi.
Rights and permissions
About this article
Cite this article
Borges, A.C., Nishime, T.M.C., de Moura Rovetta, S. et al. Cold Atmospheric Pressure Plasma Jet Reduces Trichophyton rubrum Adherence and Infection Capacity. Mycopathologia 184, 585–595 (2019). https://doi.org/10.1007/s11046-019-00375-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-019-00375-2