Abstract
This review describes the basic principles of radiometal-theranostics and its dawn based on the development of the positron-emitting 86Y and 86Y-labeled radiopharmaceuticals to quantify biodistribution and dosimetry of 90Y-labeled analogue therapeutics. The nuclear and inorganic development of 86Y (including nuclear and cross section data, irradiation, radiochemical separation and recovery) led to preclinical and clinical evaluation of 86Y-labeled citrate and EDTMP complexes and yielded organ radiation doses in terms of mGy/MBq 90Y. The approach was extended to [86/90Y]Y-DOTA-TOC, yielding again yielded organ radiation doses in terms of mGy/MBq 90Y. The review further discusses the consequences of this early development in terms of further radiometals that were used (68Ga, 177Lu etc.), more chelators that were developed, new biological targets that were addressed (SSTR, PSMA, FAP, etc.) and subsequent generations of radiometal-theranostics that resulted out of that.
Similar content being viewed by others
Introduction
The term "theranostics" overlaps with terms such as "personalized medicine" or "precision oncology" insofar as medical decisions, procedures and/or products are tailored to the individual patient. This includes technologies to produce customized pharmaceutical products that contain individual dosages for one or more active ingredients. Diagnostic tests used to select appropriate therapies are referred to as "companion diagnostics".
In the context of radiopharmacy and molecular imaging, the concept is particularly succinct: the ultimate object is successful therapy with appropriate short-range particle emitters (α or β−), crucially built on therapy-deciding and -accompanying diagnosis with photon emitters.
With the goal of patient-specific treatment, potent radiopharmaceuticals are used in a diagnostic (ideally using positron emitters for quantitative PET/CT) and a therapeutic variant. The diagnostic radiopharmaceutical is used to verify tumor indication and staging for an individual patient. Conversely, it verifies that the radiopharmaceutical at hand is a target-specific and selective molecule: the ideally suited for a specific patient. Precise diagnostic imaging also allows quantitative dosimetric information (expressed in terms of maximum radiation dose to the target tissue and tolerable dose to healthy organs) for the therapeutic variant of the theranostic agent. This is applied with optimal radioactivity of the appropriate radiopharmaceutical in the individual patient. Finally, post-therapeutic imaging with the diagnostic variant of the theranostic is part of the assessment of treatment success for the individual patient.
In the context of radiopharmacy and nuclear medicine, radiopharmaceuticals available in both a diagnostic (usually for PET/CT) and a therapeutic form are the central instruments. The transition from the diagnostic to the therapeutic derivative is made by substituting the diagnostic radionuclide by its therapeutic counterpart—where the oncological target should be identical and the pharmacological properties of the two variants should not differ. In cases where the theranostic pair is from nuclides of different elements (“mismatched pair”, e.g. gallium-68 and lutetium-177) the properties are not identical but very similar so the in vivo behaviour should not differ significantly. Radiotheranostics, by definition, share the same physiology in that they address the same oncologic target. Figure 1 gives an overview over four typical molecular design options from a radiochemical/radiopharmaceutical perspective.
Principal options of the molecular designs of Radiotheranostics. A: direct injection of radionuclide, B: injection of complexed radiometal, C: covalent coupling of a radionuclide to a targeting vector (red), D: radiometal complexed by bifunctional chelator (BFC) which is covalently bound by a linker to the targeting vector and a possible spacer
Option A (Fig. 1A) represents the specificity of individual radioisotopes to already have an oncologically relevant function in its ionic form. This includes, above all, the historically first implementation of the theranostic concept—it dates back more than 80 years. SAUL HERTZ realized the concept of thyroid diagnostics and therapy in the form of a single radionuclide, which offers both diagnostically and therapeutically relevant radiation: 131I [1, 2].
Additional “chemistry” is not required—the physiological function of the isotope in the form of iodide [131I]I− is sufficient. Another example of option A is the use of the calcium mimetics 89Sr or 223Ra for the therapy of bone metastases; here, the cations Sr2+ or Ra2+ already have an effect due to their affinity for the hydroxyapatite structure of the bones too and are applied as chloride salts [89Sr]SrCl2 and [223Ra]RaCl2, respectively [3,4,5]. Diagnostic analogues such as 18F as [18F]F−, 99mTc-bisphosphonates or modern 68 Ga-labeled bisphosphonates are all also effective "bone seekers" [6,7,8,9,10,11].
Option B (Fig. 1B) involves the rather rare clinically realized design of radiometallic-labeled complexes for therapy, where the physiological role is not from the metal but from a property of the ligand. Typical representatives are 186/188Re-HEDP complexes [12, 13].
Options C and D represent a paradigm shift. The transport function for the radioisotope to a concrete oncological target is taken over by a defined targeting vector (proteins such as antibodies, proteins as receptors, messenger analogues, inhibitors, amino acids, but also inorganic species). Now, neither the radioisotope nor the radiometallic ligand complex should have any physiological significance, but on the contrary should be physiologically inert to the greatest possible extent.
Option C applies to radiohalogens, especially 131I. Clinically relevant cases are 131I-MIBG and 131I-labeled tyrosine derivatives for the therapy of glioblastoma and other diseases, respectively [14,15,16,17]. The radioiodine is introduced into the targeting vector in a covalent bond in such a way that the physiological role of guanidine or tyrosine is not diminished significantly. In the ideal concept of radiotheranostics, the substitution of 123I or 124I for the therapeutic isotope 131I is sufficient to generate the potent diagnostic variant. Regardless of the type of iodine isotope, the pharmacokinetics of the theranostic remain absolutely identical.
Option D concerns radiometals. Unlike aliphatic or aromatic halogenation, the radiometal cannot be directly covalently coupled to a targeting vector, but requires a bifunctional chelating moiety. Docking such a relatively large chemical moiety to a small targeting vector can lead to major pharmacological interference (binding affinities, lipohilicity, etc.). Therefore, in terms of medicinal chemistry, optimizations of the chelator, as well as in linker and spacer units, play a major role [18].
In nuclear medicine, the clinical routine of a theranostic application (its logical and logistical processes) can be represented in five stages.
Quantitative diagnostics (PET/CT) with the diagnostic derivative of the theranostic agent
First, disease and disease state are evaluated for an individual patient using an appropriate diagnostic radiopharmaceutical. Conversely, or simultaneously with this, it is verified that the radiopharmaceutical at hand is a target-specific molecule: the ideally suited for that individual patient.
Structural translation of the diagnostic into a therapeutic radiopharmaceutical
This central pillar of theranostics is the task of radiopharmaceutical chemistry. How to replace the positron emitter of the PET/CT form of the theranostic with a beta or alpha emitter without compromising the specificity of the radiopharmaceutical? This task is subdivided into sub-areas: (1) What is the appropriate combination of the diagnostic/therapeutic radionuclide? From this, (2) what are the chemical properties of the chosen theranostic radionuclide and how this must affect (3) the structure of the theranostic in terms of stable radiolabeling. Finally, (4) the appropriate structure must be characterized in vitro and in preclinical studies to demonstrate broad agreement in pharmacological properties with the diagnostic derivative of the theranostic.
Pretherapeutic dosimetry
Diagnostic imaging with the PET/CT form of the theranostic agent can be converted into quantitative dosimetric information in the form of time-activity correlations. In experimentally obtained time-activity correlations of the diagnostic derivative of the theranostic agent for healthy organs and lesions, the emission profile and physical half-life of the therapeutic radionuclide are now substituted. This is used to determine the optimal radioactivity (expressed in terms of maximum radiation dose to the target tissue and tolerable dose to healthy organs) of the appropriate radiotheranostic on the individual patient, cf. Figure 2.
Simplified illustration on the determination of radiation doses based on quantitative uptake kinetics obtained by the diagnostic PET tracer of the theranostic agent. A, B and C describe different pharmacology of the theranostic. The integral (e.g. the grey area for B) gives the cumulative radiation dose D, which is obtained from the kinetics, i.e. the biological and physical half-lives expressed by λbiol and λphys, respectively. S is the S-factor representing transformation energies of a given radionuclides and A is the activity injected
Therapy
The therapeutic derivative of the theranostic is ideally applied at the activity level determined from the pretherapeutic dosimetry. This application can be repeated after appropriate times.
Post-therapeutic monitoring
Usually, the outcome of therapy is followed by quantitative imaging with the diagnostic derivative of the theranostic agent. Ideally, lesion size and SUV values will have decreased compared to pre-therapy.
The 1990s: 86Y/90Y matched isotope pair and prototype of radiometal-based theranostics
Nuclear chemistry and physics know more than 3000 radioactive isotopes—in contrast, the number routinely used in the field of diagnostic as well as therapeutic nuclear medicine is small. This is due to the fact that important selection criteria such as type and energy of the emissions, physical half-life and, above all, availability have to be fulfilled together.
For PET, these would be the short-lived "organic" radionuclides 11C, 13N, 15O, halogens such as 18F, 124I, and radiometals such as 82Rb, 64Cu, 68Ga, 86Y and others. In the field of therapeutics, 131I, 89Sr, 90Y, 153Sm, 177Lu, 161Tb, 186/188Re, 225Ac and others are used. Realistically (i.e., if one does not want to speculate on further "exotic" nuclides whose transformation properties appear promising but whose availability for clinical routine is currently only wishful thinking) very few ideal combinations result from this selection.
Radioiodide [*I]I−
Historically, the most important combination is, in fact, only one radionuclide—which offers both diagnostically and therapeutically relevant radiation. Radioiodine 131I is one of the best-known radionuclides that can be used directly in its anionic form as iodide [131I]I−. Like nonradioactive iodide, it is accumulated in the thyroid gland. After administration, radioiodide is rapidly taken up by the thyroid via the sodium iodide symporter (NIS), and excess radioiodide is excreted renally. For administration, they are all formulated as sodium iodide in slightly basic aqueous solutions. They can be taken orally or administered by injection. Scintigraphic images of the thyroid gland allow identification of various diseases and dysfunctions of the organ, such as local foci of hyperthyroidism or hypothyroidism. Because of their long half-life, these iodine isotopes are usually provided by outside vendors for routine clinical use. For example, [131I]NaI is usually supplied in capsule form with radioactivity already calibrated for specific patients. Several radioisotopes of iodine are suitable for molecular imaging and also enable PET (124I) or SPECT (123I, 131I).
However, the spectrum of theranostically significant targeting vectors utilizing radioiodine is limited. A major challenge with radioiodinated compounds is the stability in vivo due to the weak C-I bond. Deiodination can be catalyzed by deiodinases, different enzymes like iodothyronine deiodinase (DIO1-3) for example, or proteolytic cleavage of peptides that contain iodine-substituted tyrosine units [19]. Cavina et al. gave an extensive review discussing the stability of radioiodinated pharmaceuticals depending on their molecular structures [20].
86Y/90Y
In the early 1990s, several laboratories began to consider using a SPECT radionuclide as a surrogate for a therapeutic radionuclide, e.g. 111In (\({t}_{1/2}=2.8 \, {\text{d}}\)), a trivalent metal, as a surrogate for 90Y, another trivalent metal [21, 22]. The use of various other metallic radionuclides has also been discussed [21, 22].
While the β−-emitting therapeutic radionuclide 90Y (\({t}_{1/2}=2.7 \, {\text{d}}\)) had been available for a long time via the 90Sr/90Y generator system and was used for various therapies, there was no possibility of quantifiable imaging with 90Y-labeled therapeutics at that time—the patient remained a “black box”. Therefore, the β+-emitter 86Y had to be first developed for medical use [23,24,25]. This included the evaluation and optimization of radionuclide production [23, 24], radiolabeling and its analytics as well as first pilot in vivo studies to learn about the in vivo quantification via PET [25]. With a half-life of \({t}_{1/2}=14.7 \, {\text{h}}\) and a fraction of 32% positron emission it was suitable to reproduce the pharmacology of analogous 90Y-pharmaceuticals well [26,27,28,29,30,31,32]. Rösch et al. [33] gives a retrospective overview of the various aspects of the radiochemical and nuclear development work including nuclear data, cyclotron irradiation, chemical processing, quality control, etc. of 86Y and 86Y-labeled pharmaceuticals, the methodology established to quantify the molecular imaging of 86Y-labeled compounds in the form of multiple and long-term PET recordings, and finally, application examples that highlighted the ultimate goal of radiotheranostics, namely to determine the radiation dose of the 90Y-labeled compound in mGy or mSv per MBq of 90Y injected, based on the long-term PET measurements with 86Y analogues (Fig. 3). Of historical note, in addition to the methodological aspect, is the specific demonstration of the approach for the case of [90Y]Y-DOTA-TOC [29, 30]. Sandoz initially exercised the [86Y]Y-DOTA-TOC program as a diagnostic arm of [90Y]Y-DOTA-TOC before this entered the clinic. This was then realized first in baboons (Fig. 4) [29, 30] and later in patients (Fig. 5) [31, 34].
The 2000s: 177Lu/68Ga
Biological targets
The most important radiotracer for nuclear medicine oncology imaging is 2-deoxy-2-[18F]fluoro-D-glucose ([18F]FDG). Cancer cells obtain their energy mainly through aerobic glycolysis which is very inefficient. To compensate for this, the glycolysis rate is upregulated as well as the oxidative phosphorylation (Warburg effect). [18F]FDG is a glucose analogue which is likewise phosphorylated by the enzyme hexokinase. The [18F]FDG-6-phosphate on the other hand cannot be metabolized further which results in an accumulation in the cancer cell (metabolic trapping) that can be visualized via PET. Consequently, this makes [18F]FDG an almost universal oncological imaging tool. However, radiopharmaceutical chemistry does not have a therapeutic counterpart of glycolysis metabolism. Therefore, for tumor therapy, alternative oncological targets need to be identified and the appropriate radiopharmaceuticals developed, ideally for both PET/CT imaging and therapeutics. Figure 6 provides a schematic overview of the relevant targets and classes of target vectors for this purpose.
Selected targets for PET imaging in oncology and corresponding radiotracers: 2-deoxy-2-[18F]fluoro-D-glucose ([18F]FDG), O-(2-[18F]fluoroethyl)-L-tyrosine ([18F]FET). GLUT = glucose transporter, AAT = amino acid transporter, GPCR = G protein-coupled receptors, SST = somatostatin, mAb = monoclonal antibody, PSMA = prostate-specific membrane antigen, FAP = fibroblast activation protein, PS = protein synthesis [35]
Other targets are based on the increased metabolism and requirement of substances and building blocks for the high proliferation rate of tumor cells. Radiotracers as analogs of DNA and RNA building blocks are compounds such as 5-[18F]fluorouracil, [11C]thymidine, or 3′-deoxy-3′-[18F]fluorothymidine, which allow determination of the proliferation status of tumor cells by PET imaging.
Another important mechanism for oncological targeting is enhanced amino acid transporter activity by tumor cells. O-(2-[18F]fluoroethyl)-L-tyrosine ([18F]FET) and [11C-methyl]-L-methionine are the most commonly used radiolabeled amino acid analogs. In the context of theranostics, iodinated analogs are another approach.
However, it appeared that the transmembrane receptors represent the most attractive target in radiotheranostics. Typically, the corresponding targeting vectors are radiometal-labeled tracers, which is in particular relevant for their therapeutic application. For diagnostic analogs, also 18F-labeled modifications are being applied.
Radionuclides
The turn of the millennium saw a dramatic change in the theranostic isotopes utilized in the 1990s: The approach to produce carrier free 177Lu and the appearance of the 68Ge/68Ga-radionuclide generator.
Although 90Y was and still is an extremely important therapeutic isotope in theranostics and nuclear medicine in general, 177Lu (\({t}_{1/2}=6.65 \, {\text{d}}\)) became relevant because of the lower energy of the emitted β− particles. The 176Lu(n,γ) production pathway was easily established and gives good yields due to the high cross section, yet the content of 176Lu carrier and the contamination with the long-lived isomer 177mLu appeared to be critical for theranostics targeting e.g. saturable oncological targets such as GPC receptors. The indirect 176Yb(n,γ)177Yb \(\stackrel{{\beta }^{-}}{\to }\) 177Lu production pathway suggested an alternative option [36]. It is now commercially realized at TBq scale and GMP levels [37].
With the start of the new millennium, the Obninsk team provided a 68Ge/68Ga-radionuclide generator providing the positron-emitting trivalent radiometal 68Ga (\({t}_{1/2}=68 \, {\text{min}}\)) in a chemical environment easily to label radiopharmaceuticals by its diluted hydrochloric acid eluent system and its low contamination levels of long-lived parent isotope 68Ge (\({t}_{1/2}=271 \, {\text{d}}\)) [38]. The post-processing chemistry introduced by Zhernosekov et al. [39] and Asti et al. [40] translated this generator to nuclear medicine. This was crucial to the increasing success of 68Ga and its routine applications in PET diagnosis. This has been discussed in several reviews in detail, e.g. by Rösch and Riss [41] as well as Rösch and Baum [42], or different reports and book chapters [43, 44].
The 2000s: 177Lu/68Ga and theranostic octreotides for NET
A look at the surface proteins expressed by tumor cells reveals an astonishing number and variety of potential targets. The metabolism and other cellular functions of tumor cells appear to be completely unregulated. As a result, the expression of surface proteins is dramatically increased on tumor cells, which can easily reach a million-fold overexpression compared to normal cells. Moreover, several tumor entities (over)express (specific) transmembrane proteins that are hardly or only very restrictedly expressed in healthy tissues. Transmembrane receptors are large protein structures located in the cell membrane. These receptors have three main domains: the transmembrane, extracellular, and intracellular domains. The extracellular domain is the part of the cell surface that is recognized by specific ligands. In contrast, the intracellular domain is the part that generates a signal inside the cell by activating (effector) proteins or enzymes.
One prominent family is the G protein-coupled receptors (GPCRs), in which the intracellular domain is coupled to the so-called G protein, which is responsible for further signal transduction in the cell. Some GPCRs undergo endocytosis after ligand binding, which is a major advantage because it effectively traps the radiotracer inside the tumor cell.
Clearly, these surface structures are generally potential targets for tumor diagnosis and therapy. The most important transmembrane receptor class of the last decade in nuclear medicine is the human somatostatin receptor (hSSTR) family. Out of the five subtypes, hSSTR2 is the most important subtype, and to a much lesser extent hSSTR1, 3, and 5. hSSTRs are highly overexpressed in neuroendocrine tumors and some other human tumor types. Expression of hSSTR2 on tumor cells can reach 2.5-million-fold overexpression. Physiological expression of hSSTR2 in healthy tissues is very limited and is mainly found in the spleen. Therefore, hSSTR2 offers ideal properties as a target for tumor imaging (and therapy). In addition, the hSSTR family undergoes endocytosis after ligand binding, resulting in very efficient trapping of the ligand in the addressed cell.
The native ligand, somatostatin, is a peptide hormone of 14 or 28 amino acids (two isoforms). Somatostatin has a plasma half-life of only 2 min and is therefore unsuitable for molecular imaging. The truncated derivative octreotide, a much smaller cyclic peptide, has been developed as a somatostatin analog for the treatment of acromegaly and for the treatment of neuroendocrine tumors. In an initial approach, octreotide was conjugated to DTPA as a chelating system for radiolabeling with indium-111. 111In-labeled DTPA-octreotide is available as Octreoscan© for SPECT imaging [45, 46]. Further developments led to the corresponding derivative, [DOTAo-D-Phe1-Tyr3]-octreotide (DOTA-TOC), with the chelating agent DOTA for radiolabeling with various radiometals and a strongly enhanced affinity for hSSTR2 [47,48,49,50]. The theranostic pair 86Y/90Y was used for research and development as described in the previous chapter. [29,30,31, 34] Later on, for clinical routine application the theranostic pair was changed to 68Ga/177Lu due to the better availability of these radionuclides. Together with another variant, DOTA-TATE, DOTA-TOC is the major precursor for radiolabeled somatostatin analogs [51]. [68Ga]Ga-DOTA-TOC/TATE are the most commonly used tracers in routine clinical practice for PET imaging of hSSTR2-positive tumors and metastases (cf. Figure 7).
PET imaging with [68Ga]Ga-DOTA-TATE in patients suffering from neuroendocrine cancer [35]
Lessons to learn for the design of theranostic monomers
The key component is the system oncological target/specific targeting vector. The chelator is covalently attached either directly to the targeting vector (amid coupling is the preferred method usually utilizing a -COOH group at the chelator and an amine at the targeting vector).
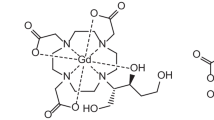
A first lesson to learn was that for therapeutic application macrocyclic chelators are much better suited because of the thermodynamic and kinetic stability of the chelates, cf. 111In-labeled DTPA-octreotide for SPECT imaging vs. 90Y-, 177Lu or 225Ac-labeled DOTA-TOC/-TATE therapeutics [51]. Pioneering work by H. Mäcke and others revealed, that the chelate is influencing the pharmacology of the theranostic compound [52, 53]. Accordingly, careful tailoring of the chelator and the radiometal belong to the challenges in radiopharmaceutical chemistry. Figure 8 depicts some of the non-macrocyclic and cyclic chelators and some bifunctional derivatives introduced around the turn of the millennium.
The proof-of-principle peptidic radiometal theranostics: 90Y-, 177Lu-, 225Ac-labeled DOTA-TOC/-TATE to treat neuroendocrine tumors: 90Y-DOTA-TOC therapies of neuroendocrine started in the last years of the last millennium, and systematic experiences were obtained in the 2000s [47, 48, 54,55,56]. Figure 9 gives a representative illustration of such applications. Obviously, the theranostic concept became a great success, and many patients benefited from this treatment. However, only decades later, this was validated by a systematic and successful clinical phase III study [57].
90Y-DOTA-TOC therapies of neuroendocrine cancer; PRRT = peptide receptor radiation therapy. [68Ga]Ga-DOTA-TOC PET images prior (left) treatment and after / between successive applications of first [90Y]Y-DOTA-TOC followed by two cycles of [177Lu]Lu-DOTA-TOC (Courtesy by R. P. Baum) [58]
The 2010s: more oncological vectors
In addition to the key/lock systems SSTR/octreotide derivatives for neuroendocrine tumors and PSMA/PSMA inhibitors for prostate cancer (PCa), there are other examples that have been validated for the diagnosis of other cancers in nuclear medicine. The chemical design is exactly the one of option D in Fig. 1. The key component is the system oncological target / specific targeting vector, while the chelator remains a common chelate.
PSMA/PSMA inhibitor
The prostate-specific membrane antigen (PSMA) has been identified as a suitable target for prostate cancer diagnosis and therapy. The corresponding binding motif is a PSMA inhibitor. Over time the very small peptidomimetic structure of Glu-urea-Lys (KuE) has established itself as the by far most commonly used PSMA-targeting vector. Several radiolabeled derivatives have been developed for molecular imaging with 18F, 68Ga and other radionuclides. The most successful and clinically used diagnostic ligand is the 68Ga-labeled ligand from DKFZ Heidelberg, which uses an HBED chelate: PSMA-11 ((EuK)-Ahx-HBED-CC, see Fig. 11A) [59, 60]. A comparative study with [18F]fluoromethylcholine showed a much higher contrast which enabled the visualization of small metastases despite low PSA levels [61]. Figure 10 shows PET imaging of prostate cancer with [68Ga]Ga-PSMA-11.
[68Ga]Ga-PSMA-11 PET imaging in patients suffering from prostate cancer [58]. a Maximum Intensity Projection (MIP) of a PET/CT at 1 h p.i. b Fusion PET/CT image. The primary prostate cancer tumor (12) as well as the lymph node metastases (11) can be visualized with a very high contrast (Courtesy of Afshar-Oromieh, DKFZ, Heidelberg, Germany) [35]
Figure 11 shows three of the most common KuE-based radiopharmaceuticals routinely used for the diagnosis of prostate cancer by PET/CT.
PSMA-617 (Fig. 11 B) has a DOTA chelator which enables theranostic application in contrast to PSMA-11 which can only be labeled with 68Ga for diagnostic PET. Unlike with [177Lu]Lu-DOTA-TATE, where over 15 years have passed between the first application and the approval [51], the approval process [177Lu]Lu-PSMA-617 is going a lot faster. Between the original unleashing in 2015 by Benesova et al. [62] and the start of the phase III clinical VISION trial in 2018 only 3 years and only 7 years until its recent approval passed [63]. Several big studies were published quickly in the early years which helped to accelerate the process [64, 65].
Besides that, efforts were made to establish 18F-labeled PSMA-inhibitors where [18F]F-DCFPyL was investigated heavily which lead to two phase III studies that resulted in a recent FDA approval [66, 67]. [18F]F-PSMA-1007 (Fig. 11 C) has also increasingly found its way into clinical routine over the last few years [68,69,70].
Hydroxyapatite in bone metastases/Bisphosphonates
Malignant tumors of the prostate, breast and other organs often lead to the formation of painful bone metastases in advanced stages. The disease is related to the activity of osteoblasts and osteoclasts, which are the active components of bone growth. The inorganic bone matrix itself consists mainly of calcium hydroxyapatite. Conventional drugs and diagnostic and therapeutic radiopharmaceuticals all share a high binding affinity to the inorganic matrix and/or the enzymes that regulate bone growth. Drugs for the treatment of osteoporosis are often used as bisphosphonate components. Bisphosphonates resemble pyrophosphate but are metabolically stable due to the replacement of the central oxygen atom with a carbon atom. In addition, this carbon atom allows the attachment of two functional groups. By using a hydroxy group as a substituent, the affinity for hydroxyapatite can be increased.
Utilizing bisphosphonates as a targeting vector, a series of theranostic tracers were developed with high binding potency to bone metastases. The first generation of bisphosphonates were the DOTA-conjugated precursors BPAMD, BPAPD and BPPED that were investigated as 68Ga-labeled derivatives in PET diagnosis [7,8,9]. Further the precursor were labeled with the therapeutic nuclides 177Lu- and 225Ac and have been successfully applied in patient studies [11, 71,72,73]. Figure 12 shows the structure of BPAMD and its PET- and ERT-application in vivo.
BPAMD, a DOTA-conjugated first-generation bisphosphonate labeled with 68Ga or 177Lu and its use in theranostics of disseminated bone metastases [35]
CAFs / FAP inhibitors
In contrast to specific molecular tumor targets such as the somatostatin receptor in neuroendocrine tumors and the prostate-specific membrane antigen in prostate cancer, the tumor microenvironment has recently been identified as a suitable target for cancer diagnosis and therapy. Cancer is a heterogeneous disease that arises in an extremely complex microenvironment. Malignant tumors are composed not only of cancer cells but also of a large majority of endogenous host stromal cells (e.g., fibroblasts, vascular and immune cells) and extracellular matrix (ECM) components, collectively referred to as the tumor microenvironment (TME) [74]. The stromal cells within the tumor (tumor stroma) comprise the majority of the total tumor mass (up to 90%) and are connected by a desmoplastic reaction [75]. Among all cells within the TME matrix, fibroblasts are considered dominant cells whose biological functions play a strong role in all stages of cancer progression and metastasis. Cancer-associated fibroblasts (CAFs) are thought to have potent tumor-modulating effects and are found in most solid tumors. In general, CAFs account for up to 80% of all fibroblasts in TME. CAFs are identified by the expression of several specific biomarkers on their surface, such as SMA (Smooth Muscle Actin), S100A4 or FSP-1 (Fibroblast-Specific Protein 1), PDGFR/ (Platelet-Derived Growth Factor Receptors), and FAP (Fibroblast Activation Protein). Fibroblast Activation Protein alpha (FAPα or FAP), also known as Seprase, is a type II membrane-bound serine protease associated with fibrosis, tissue repair, inflammation, and ECM degradation. FAP contains two types of enzymatic activity: dipeptidyl peptidase and endopeptidase. Endopeptidase enables FAP to mediate proteolytic processing of collagen I cleaved by matrix metalloproteinase, leading to prevention of morphogenesis, tissue remodeling and repair [76,77,78].
FAP appears to be a promising target in oncology because it is not expressed in normal fibroblasts and in the stroma of benign epithelial tumors, whereas it is significantly increased in the stromal compartments of various malignant tumors. The challenge for radiopharmaceutical chemistry is to develop molecular targeting vectors with high affinity for FAP and high selectivity towards related proteases. Recently, molecular antibodies, small peptides, and inhibitors have been transformed into molecular imaging probes, with inhibitors utilizing the (4-quinolinoyl)-glycyl-2-cyanopyrrolidine scaffold representing the most exciting class [79, 80]. The inhibitor structure UAMC1110 showed nanomolar affinity and the best selectivity towards the concurring enzymes prolyl endopeptidase (PREP) and dipeptidyl peptidases DPPIV, DPPVIII and DPPIX [80].
Radiopharmaceutical chemists at the German Cancer Research Center in Heidelberg pioneered the translation of this inhibitor into effective diagnostic radiopharmaceuticals by coupling chelators to the amine of the quinoline moiety of the inhibitor and introducing a series of linker and spacer motifs [81, 82]. At the University in Mainz (Germany) a linker based on squaric acid (SA), which links several bifunctional chelators (DATA5m, DOTA, etc.) to the inhibitor was used [83, 84]. Currently, 68Ga-labeled derivatives such as FAPI-04, FAPI-46, DATA5m.SA.FAPi and DOTA.SA.FAPi (cf. Figure 13) are being investigated in vivo.
These first generation of FAPi-radiotracers show promising value in the diagnosis of many different tumor types and provide new information, also in comparison with established oncologic tracers such as [18F]FDG [85, 86]. Figure 14 shows an exemplary PET image of of a thyroid cancer patient visualized with [68Ga]Ga-DOTA.SA.FAPi.
Outlook: more oncological vectors and new radioisotopes
Radioisotopes
In radiotherapy, it is the desired action of particle-induced ionization of α or β− emitters on tumor DNA. It requires the identification of the most successful radionuclide candidates which offer adequate nuclear parameters, specific activities and effective production routes including yield, purity, and cost. Routine clinical availability is the key issue. As of today, the number of such therapeutic isotopes is relatively low, yet important carrier-free β− emitters such as 90Y and 177Lu are available even at a GMP level. Availability of 225Ac, in contrast, is limited.
However, there is a substantial risk that the supply chain of those radionuclides cannot satisfy the demand of e.g. radiolabeled PSMA inhibitors. The growing number of registered theranostic radiopharmaceuticals and their dramatically growing demand even for the well-established radionuclides ask for upscaling production capacities. Interestingly, the use of nuclear reactors dedicated to nuclear energy also for isotope production is a fascinating avenue. In parallel, alternative production routes such as the potential of photonuclear reactions are being investigated-asking for dedicated facilities. Finally, research and development towards new radionuclides must continue-with 161Tb representing an important example (cf. Figure 15). Other candidates are still pending routine commercial availability on larger activities such as 211At or 212Pb.
New oncological targets and new design of targeting vectors
The dominant systems of target/targeting vectors are Somatostatin receptors (NET patients)/octreotides and PSMA (prostate cancer patients)/PSMA inhibitors-both quantified in successful clinical phase III trials and being registered drugs. In addition, in the last decade new systems have been translated from bench to bedside such as the TME / FAP inhibitors or peptides as mentioned, as well as the inorganic vectors for the system Hydroxyapatite (bone metastases) / bisphosphonates. Yet there are many more examples, just to mention bombesine-based targeting vectors targeting Gastrin-releasing protein receptor (GRPR) also known as bombesin type-2 receptor for use in prostate cancer [87, 88], the chemokine receptor CXCR4 ligands [89] and RGD-containing cyclic peptides targeting αvβ3 and other integrines [90,91,92] for different types of cancer, new SSTR antagonists for NET [93,94,95] etc. This is an ongoing progress.
However, there are also some new developments in radiopharmaceutical chemistry. One example to mention is the creation of homo- and hetero-multimers. The principal designs are illustrated in Fig. 16 with a bifunctional chelator as the central unit which has at least two functional groups for the coupling with the linker and the targeting vector. Furthermore, additional spacer units may be required.
The effect of multivalency on affinity, avidity and selectivity of receptor-ligand interactions is known for several decades [96, 97]. Based on this, multimeric designs found its way into radiopharmaceuticals in the 2000s mainly targeting the integrin αvβ3 with RGD-containing cyclic peptides such as c[RGDfK] as targeting vectors [98,99,100] but also with aptamers targeting MUC1 [101]. A 64Cu-labeled RGD-tetramer (64Cu-DOTA-E{E[c(RDGfK)]2}2) showed first promising results indicating a prolonged tumor retention time while tumor uptake and blood clearance were rapid [100].
Notni et al. developed a new bifunctional chelator TRAP (triazacyclononance-triphosphinate) which showed superior 68Ga-labeling properties compared to DOTA and NOTA (milder reaction conditions, broader pH range during labeling, higher specific activities while retaining high complex stability) and simultaneously allowed the conjugation of three targeting vectors [102]. A following study with 68Ga-TRAP(RGD)3 (“68Ga-Avebtrin”, Fig. 17) could demonstrate the superiority of the RGD trimer compared to RGD monomers [103].
Structure of TRAP(RGD)3 which can be labeled with 68Ga [103]
The concept was expanded to tetraazacyclododecane scaffold which resulted in the chelator DOTPI [104]. This allowed for the synthesis of tetramers and the radiolabeling with a broader range of radiometals such as 177Lu which enables therapeutic applications. As a proof-of-concept DOTPI was conjugated with the PSMA-targeting vector KuE via CuI-catalyzed alkyne-aide cycloaddition (CuAAC, Huisgen-reaction) and copper-free strain-promoted alkyne-aide cycloaddition (SPAAC) with DBCO (dibenzyocyclooctyne) and investigated [105].
The chelator sarcophagine (Sar) is especially suited to form stable and kinetically inert complexes with CuII. Figure 18A shows the PSMA dimer SarbisPSMA which was labeled with 64Cu. In vivo-investigation in comparison to the monomer SarPSMA showed far superior tumor uptake, tumor-to-background ratio and longer tumor retention of the dimer [106].
Besides PSMA also Gastrin-releasing peptide receptors (GRPRs) are interesting targets and strongly expressed in several types of cancer such as prostate cancer which can be targeted with bombesin (BBN)-derived peptides. Here, also several attempts were made to investigate homodimeric bombesin radiotracers [88, 108, 109].
Recently the dimeric concept was translated to FAP inhibitor-based radiopharmaceuticals since the first-generation of FAPIs like FAPI-04 and FAPI-46 and other monomers (cf. Figure 13) suffer from short tumor retention time limiting its translation towards therapy using radionuclides with longer half-lives such as 177Lu or 225Ac. Figure 18B shows the structure of DOTAGA.(SA.FAPi)2 which was labeled with 68Ga and 177Lu [107]. In comparison with [177Lu]Lu-DOTA.SA.FAPi, [177Lu]Lu-DOTAGA.(SA.FAPi)2 showed higher tumor uptake, faster clearance and longer tumor retention time. Even after 7 days p.i. the tumor lesions could still be visualized via whole-body scintigraphy [110]. The slighty higher uptakes in colon and kidneys were tolerated well by the patients.
Other groups also published FAPi dimers such as [177Lu]Lu-BiOncoFAP [111] and [68Ga]Ga-DOTA-2P(FAPI)2 [112] recently and showed similar results in murine in vivo studies regarding the biodistribution and pharmacokinetics.
Heterodimers also appeared in recent years having a similar molecular design than the homodimers but with two different targeting vectors. Most of the combinations try to simultaneously target GRPRs and integrins with a bombesin derivative and a cyclic RGD peptide [113,114,115]. PSMA-BBN [116, 117] and recently the first PSMA-FAP heterodimer [118] have also been published. Some PCa patients are PSMA-negative so they do not overexpress PSMA. This means that cannot be visualized via a monomeric PSMA radiotracer. A heterodimer could therefore be interesting to improve the rate of successful diagnosis or therapy. It has also been reported that the enzymes are both overexpressed in different malignant tumors at the same time [119, 120].
Besides that, a combination of one of an established oncological targeting vector and a human serume albumin (HSA) binding moiety emerged in radiopharmaceuticals. In most cases 4-(p-iodophenyl)butyric acid oder Evans Blue (EB) are used as a HSA binding moiety [121]. These moietites bind reversibly to albumin which results in a prolonged circulation in the blood and therefore a delayed renal clearance. This results in a prolonged tumor retention also which is why a higher accumulated radiation dose can be deposited in the tumor region. This approach has been investigated for SSTR and PSMA in humans. This could be confirmed e.g. with 177Lu-EB-TATE and 177Lu-EB-PSMA-617 with a 7.9- and 5.7-fold higher dose to the tumor compared to the monomeric derivatives, respectively [121,122,123]. But the drawbacks were also observed since the radiation dose is increased in healthy tissue as well which can result in overall lower tumor-to-background ratios. Much higher uptake was also observed in the kidneys (3.2- and sixfold) and especially the bone marrow (18.2- and sixfold) which can be critical. Even when lower initial activities are needed to treat a patient (particularly interesting for 225Ac) the uptake in healthy tissue increases roughly in the same order of magnitude than in the tumor [121,122,123].
Conclusion
Since the 1990s huge progress was made in radiometal-based theranostics in every field concerning radiopharmaceuticals. This includes new methods to produce radionuclides (improved production routes of established radionuclides as well as making new radionuclides available for routine use), improved labeling chemistry (acyclic vs. macrocyclic chelators), new oncologic targets (SSTR, PSMA, FAP, …) combined with new targeting vectors (TOC/TATE, PSMA and FAP inhibitors, …), sophisticated linker and spacer chemistry. The development in this field still is ongoing with new molecular designs (dimers and multimers with multiple targeting vectors) and most importantly the ever-increasing interaction of diagnosis and therapy.
References
Hertz S, Roberts A (1946) Radioactive iodine in the study of thyroid physiology. VII. The use of radioactive iodine therapy in hyperthyroidism. JAMA 132:81–86
Fahey FH, Grant FD, Thrall JH (2017) Saul Hertz, MD, and the birth of radionuclide therapy. EJNMMI Phys 4:15. https://doi.org/10.1186/s40658-017-0182-7
Soerdjbalie-Maikoe V, Pelger RC, Lycklama NGA, Arndt JW, Zwinderman AH, Papapoulos SE, Hamdy NA (2002) Strontium-89 (Metastron) and the bisphosphonate olpadronate reduce the incidence of spinal cord compression in patients with hormone-refractory prostate cancer metastatic to the skeleton. Eur J Nucl Med 29:494–498. https://doi.org/10.1007/s00259-001-0728-7
Nilsson S, Franzén L, Parker C, Tyrrell C, Blom R, Tennvall J, Lennernäs B, Petersson U, Johannessen DC, Sokal M, Pigott K, Yachnin J, Garkavij M, Strang P, Harmenberg J, Bolstad B, Bruland ØS (2007) Bone-targeted radium-223 in symptomatic, hormone-refractory prostate cancer: a randomised, multicentre, placebo-controlled phase II study. Lancet Oncol 8:587–594. https://doi.org/10.1016/S1470-2045(07)70147-X
Sartor O, Hoskin P, Coleman RE, Nilsson S, Vogelzang NJ, Petrenciuc O, Staudacher K, Thuresson M, Parker C (2016) Chemotherapy following radium-223 dichloride treatment in ALSYMPCA. Prostate 76:905–916. https://doi.org/10.1002/pros.23180
Delaloye B, Delaloye-Bischof A, Dudczak R, Koppenhagen K, Mata F, Penafiel A, Maul FD, Pasquier J (1985) Clinical comparison of 99mTc-HMDP and 99mTc-MDP. Eur J Nucl Med 11:182–185
Fellner M, Baum RP, Kubíček V, Hermann P, Lukeš I, Prasad V, Rösch F (2010) PET/CT imaging of osteoblastic bone metastases with 68Ga- bisphosphonates: first human study. Eur J Nucl Med Mol Imaging 37:834. https://doi.org/10.1007/s00259-009-1355-y
Fellner M, Biesalski B, Bausbacher N, Kubícek V, Hermann P, Rösch F, Thews O (2012) 68Ga-BPAMD: PET-imaging of bone metastases with a generator based positron emitter. Nucl Med Biol 39:993–999. https://doi.org/10.1016/j.nucmedbio.2012.04.007
Meckel M, Fellner M, Thieme N, Bergmann R, Kubicek V, Rösch F (2013) In vivo comparison of DOTA based 68Ga-labelled bisphosphonates for bone imaging in non-tumour models. Nucl Med Biol 40:823–830. https://doi.org/10.1016/j.nucmedbio.2013.04.012
Meckel M, Bergmann R, Miederer M, Roesch F (2017) Bone targeting compounds for radiotherapy and imaging: *Me(III)-DOTA conjugates of bisphosphonic acid, pamidronic acid and zoledronic acid. EJNMMI Radiopharm Chem 1:1–14. https://doi.org/10.1186/s41181-016-0017-1
Pfannkuchen N, Meckel M, Bergmann R, Bachmann M, Bal C, Sathekge M, Mohnike W, Baum RP, Rösch F (2017) Novel radiolabeled bisphosphonates for PET diagnosis and endoradiotherapy of bone metastases. Pharmaceuticals. https://doi.org/10.3390/ph10020045
Quirijnen JM, Han SH, Zonnenberg BA, de Klerk JM, van het Schip AD, van Dijk A, ten Kroode HF, Blijham GH, van Rijk PP (1996) Efficacy of rhenium-186-etidronate in prostate cancer patients with metastatic bone pain. J Nucl Med 37:1511–1515
Ter Heine R, Lange R, Breukels O, Bloemendal HJ, Rummenie RG, Wakker AM, de Graaf H, Beekman FJ, van der Westerlaken MML, Malingré MM, Wielders JPM, van den Berg L, Hendrikse NH, de Klerk JMH (2014) Bench to bedside development of GMP grade Rhenium-188-HEDP, a radiopharmaceutical for targeted treatment of painful bone metastases. Int J Pharm 465:317–324. https://doi.org/10.1016/j.ijpharm.2014.01.034
Troncone L, Rufini V (1997) 131I-MIBG therapy of neural crest tumours (review). Anticancer Res 17:1823–1831
Hoefnagel CA, De Kraker J, Valdés Olmos RA, Voûte PA (1994) 131I-MIBG as a first-line treatment in high-risk neuroblastoma patients. Nucl Med Commun 15:712–717. https://doi.org/10.1097/00006231-199409000-00008
Górska-Chrzastek M, Grzelak P, Bieńkiewicz M, Tybor K, Zakrzewska E, Mikołajczak R, Stefańczyk L, Kuśmierek J (2004) Assessment of clinical usefulness of 131I alpha-methyl-tyrosine and fused SPECT/MRI imaging for diagnostics of recurrent cerebral gliomas. Nucl Med Rev Cent East Eur 7:135–141
Prante O, Deichen JT, Hocke C, Kuwert T (2004) Characterization of uptake of 3-[131I]iodo-α-methyl-L-tyrosine in human monocyte-macrophages. Nucl Med Biol 31:365–372. https://doi.org/10.1016/j.nucmedbio.2003.10.006
Bartholomä MD (2012) Recent developments in the design of bifunctional chelators for metal-based radiopharmaceuticals used in positron emission tomography. Inorganica Chim Acta 389:36–51. https://doi.org/10.1016/j.ica.2012.01.061
Farhana A, Ganie SA (2010) Iodine, iodine metabolism and iodine deficiency disorders revisited. Indian J Endocrinol Metab 1:13–17
Cavina L, van der Born D, Klaren PHM, Feiters MC, Boerman OC, Rutjes FPJT (2017) Design of radioiodinated pharmaceuticals: structural features affecting metabolic stability towards in vivo deiodination. Eur J Org Chem 2017:3387–3414. https://doi.org/10.1002/ejoc.201601638
Gansow OA (1991) Newer approaches to the radiolabeling of monoclonal antibodies by use of metal chelates. Int J Radiat Appl Instrumentation Part B Nucl Med Biol 18:369–381. https://doi.org/10.1016/0883-2897(91)90063-Q
Press OW, Shan D, Howell-Clark J, Eary J, Appelbaum FR, Matthews D, King DJ, Haines AMR, Hamann P, Hinman L, Shochat D, Bernstein ID (1996) Comparative metabolism and retention of iodine-125, yttrium-90, and indium-111 radioimmunoconjugates by cancer cells. Cancer Res 56:2123–2129
Rösch F, Qaim SM, Stöcklin G (1993) Nuclear data relevant to the production of the positron emitting radioisotope 86Y via the 86Sr(p, n)- and natRb(3He, xn)-processes. Radiochim Acta 61:1–8. https://doi.org/10.1524/ract.1993.61.1.1
Rösch F, Qaim SM, Stöcklin G (1993) Production of the positron emitting radioisotope 86Y for nuclear medical application. Appl Radiat Isot 44:677–681. https://doi.org/10.1016/0969-8043(93)90131-S
Rösch F, Neumaier B, Stöcklin G, Qaim SM, Herzog H, Müller-Gärtner HW (1994) [86Y]Citrate and [86Y]EDTMP: preparation, chemical characterization and in vivo quantitation of their pharmacological data with PET. J Label Compd Radiopharm 35:546–548
Herzog H, Rosch F, Stocklin G, Lueders C, Qaim SM, Feinendegen LE (1993) Measurement of pharmacokinetics of yttrium-86 radiopharmaceuticals with PET and radiation dose calculation of analogous yttrium-90 radiotherapeutics. J Nucl Med 34:2222–2226
Brockmann J, Rösch F, Herzog H, Stolz B, Bruns C, Stöcklin G (1995) In vivo uptake kinetics and dosimetric calculations of 86Y-DTPA-octreotide with PET as a model for potential endotherapeutic octreotides labeled with 90Y. J Label Compd Radiopharm 37:519–521
Rösch F, Herzog H, Plag C, Neumaier B, Braun U, Müller-Gärtner HW, Stöcklin G (1996) Radiation doses of yttrium-90 citrate and yttrium-90 EDTMP as determined via analogous yttrium-86 complexes and positron emission tomography. Eur J Nucl Med 23:958–966. https://doi.org/10.1007/bf01084371
Brockmann J, Rösch F, Herzog H, Mühlensiepen H, Köhle M, Stolz B, Marbach P, Müller-Gärtner HW (1997) Complexation, in vivo-stability, blood clearance and excretion kinetics of 86Y-DOTA-Tyr3-octreotide in baboons. J Label Compd Radiopharm 39:468–470
Rösch F, Herzog H, Stolz B, Brockmann J, Köhle M, Mühlensiepen H (1999) Uptake kinetics of the somatostatin receptor using positron emission tomography in non-human primates and calculation of radiation doses of the 90Y-labelled analogue. Eur J Nucl Med 26:358–366
Förster GJ, Engelbach M, Brockmann J, Reber H, Buchholz HG, Mäcke HR, Rösch F, Herzog H, Bartenstein P (2001) Preliminary data on biodistribution and dosimetry for therapy planning of somatostatin receptor positive tumours: comparison of 86Y-DOTATOC and 111In-DTPA-octreotide. Eur J Nucl Med 28:1743–1750. https://doi.org/10.1007/s002590100628
Buchholz HG, Herzog H, Förster GJ, Reber H, Nickel O, Rösch F, Bartenstein P (2003) PET imaging with yttrium-86: comparison of phantom measurements acquired with different PET scanners before and after applying background subtraction. Eur J Nucl Med Mol Imaging 30:716–720. https://doi.org/10.1007/s00259-002-1112-y
Rösch F, Herzog H, Qaim SM (2017) The beginning and development of the theranostic approach in nuclear medicine, as exemplified by the radionuclide pair 86Y and 90Y. Pharmaceuticals 10:1–28. https://doi.org/10.3390/ph10020056
Stolz B, Bruns C, Albert R, Rösch F, Smith-Jones P, Raulf F, Hoyer D, Weckbecker G (1999) Somatostatin receptor-targeted radiotherapy-preclinical proof of concept. Octreotide Next Decad 1:2114
Ross TL, Rösch F (2022) 12 life sciences: nuclear medicine diagnosis. In: Rösch F (ed) Nuclear- and radiochemistry volume 2: modern applications, 2nd edn. Walter De Gruyter GmbH & Co.KG, Berlin, pp 471–560
Lebedev NA, Novgorodov AF, Misiak R, Brockmann J, Rösch F (2000) Radiochemical separation of no-carrier-added 177Lu as produced via the 176Yb(n, γ)177Yb→177Lu process. Appl Radiat Isot 53:421–425. https://doi.org/10.1016/S0969-8043(99)00284-5
Barkhausen C (2011) Production of non carrier added (n.c.a.) 177Lu for radiopharmaceutical applications. Dissertation (TU Munich)
Razbash AA, Sevastianov YG, Krasnov NN, Leonov AI, Pavlekin VE Germanium-68 row of products. In: Proceedings of the 5th international conference on isotopes (5ICI). Brussels, Belgium, Medimond, Bologna, p 147
Zhernosekov KP, Filosofov DV, Baum RP, Aschoff P, Bihl H, Razbash AA, Jahn M, Jennewein M, Rösch F (2007) Processing of generator-produced 68Ga for medical application. J Nucl Med 48:1741–1748. https://doi.org/10.2967/jnumed.107.040378
Asti M, De Pietri G, Fraternali A, Grassi E, Sghedoni R, Fioroni F, Roesch F, Versari A, Salvo D (2008) Validation of 68Ge/68Ga generator processing by chemical purification for routine clinical application of 68Ga-DOTATOC. Nucl Med Biol 35:721–724. https://doi.org/10.1016/j.nucmedbio.2008.04.006
Roesch F, Riss PJ (2010) The renaissance of the 68Ge/68Ga radionuclide generator initiates new developments in 68Ga radiopharmaceutical chemistry. Curr Top Med Chem 10:1633–1668. https://doi.org/10.2174/156802610793176738
Rösch F, Baum RP (2011) Generator-based PET radiopharmaceuticals for molecular imaging of tumours: on the way to THERANOSTICS. Dalt Trans 40:6104–6111. https://doi.org/10.1039/c0dt01504k
Roesch F, Filosofov D V. (2010) Production, radiochemical processing and quality evaluation of Ge-68. In: IAEA-TEC-DOC radioisotopes and radiopharmaceuticals, Series 2: Production of Long Lived Parent Radionuclides for Generators: 68Ge, 82Sr, 90Sr and <s. Vienna
Roesch F (2012) Ge-68/Ga-68 generators: past, present, and future. In: Baum RP, Roesch F (eds) Recent results in cancer research 194. Springer, Berlin, pp 3–16
Bakker WH, Albert R, Bruns C, Breeman WAP, Hofland LJ, Marbach P, Pless J, Pralet D, Stolz B, Koper JW, Lamberts SWJ, Visser TJ, Krenning EP (1991) [111In-DTPA-D-Phe1]-octreotide, a potential radiopharmaceutical for imaging of somatostatin receptor-positive tumors: synthesis, radiolabeling and in vitro validation. Life Sci 49:1583–1591. https://doi.org/10.1016/0024-3205(91)90052-D
Krenning EP, Kwekkeboom DJ, Bakker WH, Breeman WAP, Kooij PPM, Oei HY, van Hagen M, Postema PTE, de Jong M, Reubi JC, Visser TJ, Reijs AEM, Hofland LJ, Koper JW, Lamberts SWJ (1993) Somatostatin receptor scintigraphy with [111In-DTPA-d-Phe1]- and [123I-Tyr3]-octreotide: the Rotterdam experience with more than 1000 patients. Eur J Nucl Med 20:716–731. https://doi.org/10.1007/BF00181765
Otte A, Jermann E, Behe M, Goetze M, Bucher HC, Roser HW, Heppeler A, Mueller-Brand J, Maecke HR (1997) DOTATOC: a powerful new tool for receptor-mediated radionuclide therapy. Eur J Nucl Med 24:792–795. https://doi.org/10.1007/BF00879669
Stolz B, Weckbecker G, Smith-Jones PM, Albert R, Raulf F, Bruns C (1998) The somatostatin receptor-targeted radiotherapeutic [90Y-DOTA-dPhe1, Tyr3]octreotide (90Y-SMT 487) eradicates experimental rat pancreatic CA 20948 tumours. Eur J Nucl Med 25:668–674. https://doi.org/10.1007/s002590050268
Reubi JC, Schär J-C, Waser B, Wenger S, Heppeler A, Schmitt JS, Mäcke HR (2000) Affinity profiles for human somatostatin receptor subtypes SST1–SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med 27:273–282. https://doi.org/10.1007/s002590050034
Hofmann M, Maecke H, Börner A, Weckesser E, Schöffski P, Oei M, Schumacher J, Henze M, Heppeler A, Meyer G, Knapp W (2001) Biokinetics and imaging with the somatostatin receptor PET radioligand 68Ga-DOTATOC: preliminary data. Eur J Nucl Med 28:1751–1757. https://doi.org/10.1007/s002590100639
Kwekkeboom DJ, Bakker WH, Kooij PP, Konijnenberg MW, Srinivasan A, Erion JL, Schmidt MA, Bugaj JL, de Jong M, Krenning EP (2001) [177Lu-DOTA0, Tyr3]octreotate: comparison with [111In-DTPA0]octreotide in patients. Eur J Nucl Med 28:1319–1325. https://doi.org/10.1007/s002590100574
Heppeler A, Froidevaux S, Mäcke HR, Jermann E, Béhé M, Powell P, Hennig M (1999) Radiometal-labelled macrocyclic chelator-derivatised somatostatin analogue with superb tumor-targeting properties and potential for receptor-mediated internal radiotherapy. Chem A Eur J 5:1974–1981
Fani M, Del Pozzo L, Abiraj K, Mansi R, Tamma ML, Cescato R, Waser B, Weber WA, Reubi JC, Maecke HR (2011) PET of somatostatin receptor-positive tumors using 64Cu- and 68Ga-somatostatin antagonists: the chelate makes the difference. J Nucl Med 52:1110–1118. https://doi.org/10.2967/jnumed.111.087999
Paganelli G, Zoboli S, Cremonesi M, Bodei L, Ferrari M, Grana C, Bartolomei M, Orsi F, De Cicco C, Mäcke HR, Chinol M, De Braud F (2001) Receptor-mediated radiotherapy with 90Y-DOTA-D-Phe1-Tyr3-octreotide. Eur J Nucl Med 28:426–434. https://doi.org/10.1007/s002590100490
Bodei L, Cremonesi M, Zoboli S, Grana C, Bartolomei M, Rocca P, Caracciolo M, Mäcke HR, Chinol M, Paganelli G (2003) Receptor-mediated radionuclide therapy with 90Y-DOTATOC in association with amino acid infusion: a phase I study. Eur J Nucl Med Mol Imaging 30:207–216. https://doi.org/10.1007/s00259-002-1023-y
Waldherr C, Pless M, Maecke HR, Haldemann A (2001) Original article in the treatment of neuroendocrine tumours: a clinical phase II study. Ann Oncol 12:941–945
Strosberg J, El-Haddad G, Wolin E et al (2017) Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med 376:125–135. https://doi.org/10.1056/nejmoa1607427
Cutler CS (2022) 13 life sciences: therapy. In: Rösch F (ed) Nuclear- and radiochemistry volume 2: modern applications, 2nd edn. Walter De Gruyter GmbH & Co.KG, Berlin, pp 561–612
Eder M, Schäfer M, Bauder-Wüst U, Hull WE, Wängler C, Mier W, Haberkorn U, Eisenhut M (2012) 68Ga-complex lipophilicity and the targeting property of a urea-based PSMA inhibitor for PET imaging. Bioconjug Chem 23:688–697. https://doi.org/10.1021/bc200279b
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, Graner FP, Kübler H, Haberhorn U, Eisenhut M, Wester HJ, Gschwend JE, Schwaiger M (2015) Evaluation of hybrid 68Ga-PSMA ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med 56:668–674. https://doi.org/10.2967/jnumed.115.154153
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, Holland-Letz T, Hadaschik BA, Giesel FL, Debus J, Haberkorn U (2014) Comparison of PET imaging with a 68Ga-labelled PSMA ligand and 18F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging 41:11–20. https://doi.org/10.1007/s00259-013-2525-5
Benešová M, Bauder-Wüst U, Schäfer M, Klika KD, Mier W, Haberkorn U, Kopka K, Eder M (2016) Linker modification strategies to control the prostate-specific membrane antigen (PSMA)-targeting and pharmacokinetic properties of DOTA-conjugated PSMA inhibitors. J Med Chem 59:1761–1775. https://doi.org/10.1021/acs.jmedchem.5b01210
Hope TA (2020) From compassionate use to phase 3 trial: the impact of germany’s PSMA-617 literature. J Nucl Med 61:255S-256S
Rahbar K, Ahmadzadehfar H, Kratochwil C et al (2017) German multicenter study investigating 177Lu-PSMA-617 radioligand therapy in advanced prostate cancer patients. J Nucl Med 58:85–90. https://doi.org/10.2967/jnumed.116.183194
Hofman MS, Violet J, Hicks RJ, Ferdinandus J, Thang SP, Akhurst T, Iravani A, Kong G, Ravi Kumar A, Murphy DG, Eu P, Jackson P, Scalzo M, Williams SG, Sandhu S (2018) [177Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol 19:825–833. https://doi.org/10.1016/S1470-2045(18)30198-0
Pienta KJ, Gorin MA, Rowe SP, Carroll PR, Pouliot F, Probst S, Saperstein L, Preston MA, Alva AS, Patnaik A, Durack JC, Stambler N, Lin T, Jensen J, Wong V, Siegel BA, Morris MJ (2021) A phase 2/3 prospective multicenter study of the diagnostic accuracy of prostate specific membrane antigen PET/CT with 18F-DCFPyL in prostate cancer patients (OSPREY). J Urol 206:52–61. https://doi.org/10.1097/JU.0000000000001698
Morris MJ, Rowe SP, Gorin MA et al (2021) Diagnostic performance of 18F-DCFPyL-PET/CT in men with biochemically recurrent prostate cancer: results from the CONDOR Phase III, multicenter study. Clin Cancer Res 27:3674–3682. https://doi.org/10.1158/1078-0432.CCR-20-4573
Giesel FL, Cardinale J, Schäfer M, Neels O, Benešová M, Mier W, Haberkorn U, Kopka K, Kratochwil C (2016) 18F-Labelled PSMA-1007 shows similarity in structure, biodistribution and tumour uptake to the theragnostic compound PSMA-617. Eur J Nucl Med Mol Imaging 43:1929–1930. https://doi.org/10.1007/s00259-016-3447-9
Giesel FL, Hadaschik B, Cardinale J, Radtke J, Vinsensia M, Lehnert W, Kesch C, Tolstov Y, Singer S, Grabe N, Duensing S, Schäfer M, Neels OC, Mier W, Haberkorn U, Kopka K, Kratochwil C (2017) F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging 44:678–688. https://doi.org/10.1007/s00259-016-3573-4
Giesel FL, Kesch C, Yun M, Cardinale J, Haberkorn U, Kopka K, Kratochwil C, Hadaschik BA (2017) 18F-PSMA-1007 PET/CT detects micrometastases in a patient with biochemically recurrent prostate cancer. Clin Genitourin Cancer 15:e497–e499. https://doi.org/10.1016/j.clgc.2016.12.029
Pfannkuchen N, Bausbacher N, Pektor S, Miederer M, Roesch F (2018) In vivo evaluation of [225Ac] Ac-DOTAZOL for α-therapy of bone metastases. Curr Radiopharm 11:223–230
Kreppel B, Gaertner FC, Ahmadzadehfar H, Khawar A, Roesch F, Kürpig S, Meisenheimer M, Essler M, Bundschuh RA (2020) Lu-DOTA-zoledronate therapy-first application in a patient with primary osseous metastatic bronchial carcinoma. Nuklearmedizin 59:281–283. https://doi.org/10.1055/a-1151-4592
Yadav MP, Ballal S, Meckel M, Roesch F, Bal C (2020) [177Lu]Lu-DOTA-ZOL bone pain palliation in patients with skeletal metastases from various cancers: efficacy and safety results. EJNMMI Res. https://doi.org/10.1186/s13550-020-00709-y
Ramamonjisoa N, Ackerstaff E (2017) Characterization of the tumor microenvironment and tumor-stroma interaction by non-invasive preclinical imaging. Front Oncol 7:28–37
Garin-Chesa P, Old LJ, Rettig WJ (1990) Cell surface glycoprotein of reactive stromal fibroblasts as a potential antibody target in human epithelial cancers. Proc Natl Acad Sci U S A 87:7235–7239. https://doi.org/10.1073/pnas.87.18.7235
Hamson EJ, Keane FM, Tholen S, Schilling O, Gorrell MD (2014) Understanding fibroblast activation protein (FAP): substrates, activities, expression and targeting for cancer therapy. Proteomics Clin Appl 8:454–463. https://doi.org/10.1002/prca.201300095
Puré E (2009) The road to integrative cancer therapies: emergence of a tumor-associated fibroblast protease as a potential therapeutic target in cancer. Expert Opin Ther Targets 13:967–973. https://doi.org/10.1517/14728220903103841
Imlimthan S, Moon ES, Rathke H, Afshar-Oromieh A, Rösch F, Rominger A, Gourni E (2021) New frontiers in cancer imaging and therapy based on radiolabeled fibroblast activation protein inhibitors: a rational review and current progress. Pharmaceuticals 14:1023
Jansen K, De Winter H, Heirbaut L, Cheng JD, Joossens J, Lambeir AM, De Meester I, Augustyns K, Van Der Veken P (2013) Selective inhibitors of fibroblast activation protein (FAP) with a (4-Quinolinoyl)-glycyl-2-cyanopyrrolidine Scaffold. ACS Med Chem Lett 4:491–496. https://doi.org/10.1021/ml300410d
Jansen K, Heirbaut L, Verkerk R, Cheng JD, Joossens J, Cos P, Maes L, Lambeir AM, De Meester I, Augustyns K, Van Der Veken P (2014) Extended structure-activity relationship and pharmacokinetic investigation of (4-quinolinoyl)glycyl-2-cyanopyrrolidine inhibitors of fibroblast activation protein (FAP). J Med Chem 57:3053–3074. https://doi.org/10.1021/jm500031w
Loktev A, Lindner T, Mier W, Debus J, Altmann A, Jäger D, Giesel F, Kratochwil C, Barthe P, Roumestand C, Haberkorn U (2018) A tumor-imaging method targeting cancer-associated fibroblasts. J Nucl Med 59:1423–1429. https://doi.org/10.2967/jnumed.118.210435
Loktev A, Lindner T, Burger EM, Altmann A, Giesel F, Kratochwil C, Debus J, Marmé F, Jäger D, Mier W, Haberkorn U (2019) Development of fibroblast activation protein-targeted radiotracers with improved tumor retention. J Nucl Med 60:1421–1429. https://doi.org/10.2967/jnumed.118.224469
Moon ES, Elvas F, Vliegen G, De Lombaerde S, Vangestel C, De Bruycker S, Bracke A, Eppard E, Greifenstein L, Klasen B, Kramer V, Staelens S, De Meester I, Van der Veken P, Rösch F (2020) Targeting fibroblast activation protein (FAP): next generation PET radiotracers using squaramide coupled bifunctional DOTA and DATA5m chelators. EJNMMI Radiopharm Chem. https://doi.org/10.1186/s41181-020-00102-z
Moon ES, Van Rymenant Y, Battan S, De Loose J, Bracke A, Van der Veken P, De Messter I, Rosch F (2021) In vitro evaluation of the squaramide-conjugated fibroblast activation protein inhibitor-based agents AAZTA5.SA.FAPi and DOTA.SA.FAPi. Molecules 26:3482
Ballal S, Yadav MP, Moon ES, Kramer VS, Roesch F, Kumari S, Tripathi M, ArunRaj ST, Sarswat S, Bal C (2021) Biodistribution, pharmacokinetics, dosimetry of [68Ga]Ga-DOTA.SA.FAPi, and the head-to-head comparison with [18F]F-FDG PET/CT in patients with various cancers. Eur J Nucl Med Mol Imaging 48:1915–1931. https://doi.org/10.1007/s00259-020-05132-y
Kratochwil C, Flechsig P, Lindner T, Abderrahim L, Altmann A, Mier W, Adeberg S, Rathke H, Röhrich M, Winter H, Plinkert PK, Marme F, Lang M, Kauczor HU, Jäger D, Debus J, Haberkorn U, Giesel FL (2019) 68Ga-FAPI PET/CT: Tracer uptake in 28 different kinds of cancer. J Nucl Med 60:801–805. https://doi.org/10.2967/jnumed.119.227967
Baratto L, Jadvar H, Iagaru A (2018) Prostate cancer theranostics targeting gastrin-releasing peptide receptors. Mol Imaging Biol 20:501–509. https://doi.org/10.1007/s11307-017-1151-1
Liolios C, Buchmuller B, Bauder-Wüst U, Schäfer M, Leotta K, Haberkorn U, Eder M, Kopka K (2018) Monomeric and dimeric 68Ga-labeled bombesin analogues for positron emission tomography (PET) imaging of tumors expressing gastrin-releasing peptide receptors (GRPrs). J Med Chem 61:2062–2074. https://doi.org/10.1021/acs.jmedchem.7b01856
Woodard LE, Nimmagadda S (2011) CXCR4-based imaging agents. J Nucl Med 52:1665–1669
Steiger K, Quigley NG, Groll T, Richter F, Zierke MA, Beer AJ, Weichert W, Schwaiger M, Kossatz S, Notni J (2021) There is a world beyond αvβ3-integrin: multimeric ligands for imaging of the integrin subtypes αvβ6, αvβ8, αvβ3, and α5β1 by positron emission to. EJNMMI Res. https://doi.org/10.1186/s13550-021-00842-2
Klubo-Gwiezdzinska J, Chen X (2020) Targeting integrins with radiolabeled RGD analogues for radiotheranostics of metastatic radioactive iodine nonresponsive thyroid cancer: new avenues in personalized medicine. Thyroid 30:476–478
Haubner R, Maschauer S, Prante O (2014) PET radiopharmaceuticals for imaging integrin expression: tracers in clinical studies and recent developments. Biomed Res Int. https://doi.org/10.1155/2014/871609
Baum RP, Zhang J, Schuchardt C, Müller D, Mäcke H (2021) First-in-human study of novel SSTR antagonist 177Lu-DOTA-LM3 for peptide receptor radionuclide therapy in patients with metastatic neuroendocrine neoplasms: dosimetry, safety and efficacy. J Nucl Med. https://doi.org/10.2967/jnumed.120.258889
Borgna F, Barritt P, Grundler PV, Talip Z, Cohrs S, Zeevaart JR, Köster U, Schibli R, van der Meulen NP, Müller C (2021) Simultaneous visualization of 161Tb-and 177Lu-Labeled somatostatin analogues using dual-isotope SPECT imaging. Pharmaceutics 13:1–13. https://doi.org/10.3390/pharmaceutics13040536
Borgna F, Haller S, Rodriguez JMM, Ginj M, Grundler PV, Zeevaart JR, Köster U, Schibli R, van der Meulen NP, Müller C (2022) Combination of terbium-161 with somatostatin receptor antagonists—a potential paradigm shift for the treatment of neuroendocrine neoplasms. Eur J Nucl Med Mol Imaging 49:1113–1126. https://doi.org/10.1007/s00259-021-05564-0
Hornick CL, Karush F (1972) Antibody affinity-III the role of multivalence. Immunochemistry 9:325–330. https://doi.org/10.1016/0019-2791(72)90096-1
Ehrlich PH (1979) The effect of multivalency on the specificity of protein and cell interactions. J Theor Biol 81:123–127. https://doi.org/10.1016/0022-5193(79)90085-7
Liu S, Edwards DS, Ziegler MC, Harris AR, Hemingway SJ, Barrett JA (2001) 99mTc-labeling of a hydrazinonicotinamide-conjugated vitronectin receptor antagonist useful for imaging tumors. Bioconjug Chem 12:624–629. https://doi.org/10.1021/bc010012p
Chen X, Liu S, Hou Y, Tohme M, Park R, Bading JR, Conti PS (2004) MicroPET imaging of breast cancer αv-integrin expression with 64Cu-labeled dimeric RGD peptides. Mol Imaging Biol 6:350–359. https://doi.org/10.1016/j.mibio.2004.06.004
Wu Y, Zhang X, Xiong Z, Cheng Z, Fisher DR, Liu S, Gambhir SS, Chen X (2005) microPET imaging of glioma integrin αvβ3 expression using 64Cu-labeled tetrameric RGD peptide. J Nucl Med 46:1707–1718
Borbas KE, Ferreira CSM, Perkins A, Bruce JI, Missailidis S (2007) Design and synthesis of mono- and multimeric targeted radiopharmaceuticals based on novel cyclen ligands coupled to anti-MUC1 aptamers for the diagnostic imaging and targeted radiotherapy of cancer. Bioconjug Chem 18:1205–1212
Notni J, Hermann P, Havlíčková J, Kotek J, Kubíček V, Plutnar J, Loktionova N, Riss PJ, Rösch F, Lukeš I (2010) A triazacyclononane-based bifunctional phosphinate ligand for the preparation of multimeric 68Ga tracers for positron emission tomography. Chem A Eur J 16:7174–7185. https://doi.org/10.1002/chem.200903281
Notni J, Pohle K, Wester HJ (2013) Be spoilt for choice with radiolabelled RGD peptides: preclinical evaluation of 68Ga-TRAP(RGD)3. Nucl Med Biol 40:33–41. https://doi.org/10.1016/j.nucmedbio.2012.08.006
Šimeček J, Hermann P, Havlíčková J, Herdtweck E, Kapp TG, Engelbogen N, Kessler H, Wester H-J, Notni J (2013) A cyclen-based tetraphosphinate chelator for the preparation of radiolabeled tetrameric bioconjugates. Chemistry 19:7748–7757. https://doi.org/10.1002/chem.201300338
Wurzer A, Vágner A, Horváth D, Fellegi F, Wester HJ, Kálmán FK, Notni J (2018) Synthesis of symmetrical tetrameric conjugates of the radiolanthanide chelator DOTPI for application in endoradiotherapy by means of click chemistry. Front Chem 6:1–11. https://doi.org/10.3389/fchem.2018.00107
Zia NA, Cullinane C, Van Zuylekom JK, Waldeck K, McInnes LE, Buncic G, Haskali MB, Roselt PD, Hicks RJ, Donnelly PS (2019) A bivalent inhibitor of prostate specific membrane antigen radiolabeled with copper-64 with high tumor uptake and retention. Angew Chemie Int Ed 58:14991–14994. https://doi.org/10.1002/anie.201908964
Moon ES, Ballal S, Yadav MP, Bal C, Van RY (2021) Fibroblast Activation Protein (FAP) targeting homodimeric FAP inhibitor radiotheranostics : a step to improve tumor uptake and retention time. Am J Nucl Med Mol Imaging 11:476–491
Fournier P, Dumulon-perreault V, Ait-mohand S, Langlois R, Bénard F, Lecomte R, Guérin B (2012) Comparative study of 64Cu/NOTA-[D-Tyr, beta Ala11, Thi13, Nle14] BBN(6–14) monomer and dimers for prostate cancer PET imaging. EJNMMI Res 2:8
Yu Z, Carlucci G, Ananias HJK, Dierckx RAJO, Liu S, Helfrich W, Wang F, De Jong IJ, Elsinga PH (2013) Evaluation of a technetium-99m labeled bombesin homodimer for GRPR imaging in prostate cancer. Amino Acids 44:543–553. https://doi.org/10.1007/s00726-012-1369-9
Ballal S, Yadav MP, Moon ES, Kramer VS, Roesch F, Kumari S, Bal C (2021) First-in-human results on the biodistribution, pharmacokinetics, and dosimetry of [177Lu]Lu-DOTA.SA.FAPi and [177Lu]Lu-DOTAGA.(SA.FAPi)2. Pharmaceuticals 14:555
Galbiati A, Zana A, Bocci M, Millul J, Elsayed A, Mock J, Neri D, Cazzamalli S (2022) A novel dimeric FAP-targeting small molecule-radio conjugate with high and prolonged tumour uptake. J Nucl Med. https://doi.org/10.2967/jnumed.122.264036
Zhao L, Niu B, Fang J, Pang Y, Li S, Xie C, Sun L, Zhang X, Guo Z, Lin Q, Chen H (2022) Synthesis, preclinical evaluation, and a pilot clinical PET imaging study of 68Ga-Labeled FAPI dimer. J Nucl Med 63:862–868. https://doi.org/10.2967/jnumed.121.263016
Liu Z, Li ZB, Cao Q, Liu S, Wang F, Chen X (2009) Small-animal PET of tumors with 64Cu-labeled RGD-bombesin heterodimer. J Nucl Med 50:1168–1177. https://doi.org/10.2967/jnumed.108.061739
Jackson AB, Nanda PK, Rold TL, Sieckman GL, Szczodroski AF, Hoffman TJ, Chen X, Smith CJ (2012) 64Cu-NO2A-RGD-Glu-6-Ahx-BBN(7–14)NH 2: a heterodimeric targeting vector for positron emission tomography imaging of prostate cancer. Nucl Med Biol 39:377–387. https://doi.org/10.1016/j.nucmedbio.2011.10.004
Stott Reynolds TJ, Schehr R, Liu D, Xu J, Miao Y, Hoffman TJ, Rold TL, Lewis MR, Smith CJ (2015) Characterization and evaluation of DOTA-conjugated Bombesin/RGD-antagonists for prostate cancer tumor imaging and therapy. Nucl Med Biol 42:99–108. https://doi.org/10.1016/j.nucmedbio.2014.10.002
Bandari RP, Jiang Z, Reynolds TS, Bernskoetter NE, Szczodroski AF, Bassuner KJ, Kirkpatrick DL, Rold TL, Sieckman GL, Hoffman TJ, Connors JP, Smith CJ (2014) Synthesis and biological evaluation of copper-64 radiolabeled [DUPA-6-Ahx-(NODAGA)-5-Ava-BBN(7–14)NH2], a novel bivalent targeting vector having affinity for two distinct biomarkers (GRPr/PSMA) of prostate cancer. Nucl Med Biol 41:355–363
Liolios C, Schäfer M, Haberkorn U, Eder M, Kopka K (2016) Novel bispecific PSMA/GRPR targeting radioligands with optimized pharmacokinetics for improved PET imaging of prostate cancer. Bioconjug Chem 27:737–751. https://doi.org/10.1021/acs.bioconjchem.5b00687
Hu K, Li L, Huang Y, Ye S, Zhong J, Yan Q, Zhong Y, Fu L, Feng P, Li H (2022) Radiosynthesis and preclinical evaluation of bispecific PSMA/FAP heterodimers for tumor imaging. Pharmaceuticals 15:1–14. https://doi.org/10.3390/ph15030383
de Galiza BF, Queiroz MA, Nunes RF, Costa LB, Zaniboni EC, Marin JFG, Cerri GG, Buchpiguel CA (2020) Nonprostatic diseases on PSMA PET imaging: a spectrum of benign and malignant findings. Cancer Imaging 20:23. https://doi.org/10.1186/s40644-020-00300-7
Liu F, Qi L, Liu B, Liu J, Zhang H, Che D, Cao J, Shen J, Geng J, Bi Y, Ye L, Pan B, Yu Y (2015) Fibroblast activation protein overexpression and clinical implications in solid tumors: a meta-analysis. PLoS ONE 10:1–18. https://doi.org/10.1371/journal.pone.0116683
Lau J, Jacobson O, Niu G, Lin KS, Bénard F, Chen X (2019) Bench to bedside: albumin binders for improved cancer radioligand therapies. Bioconjug Chem 30:487–502. https://doi.org/10.1021/acs.bioconjchem.8b00919
Wang Z, Tian R, Niu G, Ma Y, Lang L, Szajek LP, Kiesewetter DO, Jacobson O, Chen X (2018) Single low-dose injection of evans blue modified PSMA-617 radioligand therapy eliminates prostate-specific membrane antigen positive tumors. Bioconjug Chem 29:3213–3221. https://doi.org/10.1021/acs.bioconjchem.8b00556
Tian R, Jacobson O, Niu G, Kiesewetter DO, Wang Z, Zhu G, Ma Y, Liu G, Chen X (2018) Evans blue attachment enhances somatostatin receptor subtype-2 imaging and radiotherapy. Theranostics 8:735–745. https://doi.org/10.7150/thno.23491
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
*The Hevesy Medal and a certificate was presented Professor RÖSCH at the at the HMA-2022 Ceremony during the 19th Radiochemical Conference (RadChem-2022) in Mariánské Lázně, Czechia, May 15–20, 2022. This article summarizes the lecture given at the conference.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roesch, F., Martin, M. Radiometal-theranostics: the first 20 years*. J Radioanal Nucl Chem 332, 1557–1576 (2023). https://doi.org/10.1007/s10967-022-08624-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10967-022-08624-3