Abstract
Congruence in spirituality between HIV+ adolescent (n = 40)/family (n = 40) dyads and psychological adjustment and quality of life were assessed, using the Spiritual Well-Being Scale of the Functional Assessment of Chronic Illness Therapy, Beck Depression Inventory-II, Beck Anxiety Inventory and Pediatric Quality of Life Inventory at baseline and 3-month post-intervention. Adolescents were 60 % female and 92 % African American. Congruence in spirituality between adolescent/surrogate dyads remained unchanged at 3 months. High congruence existed for “having a reason for living”; rejection of “life lacks meaning/purpose” and “HIV is a punishment from God.” Adolescents were less likely to forgive the harm others caused them than their families.
Similar content being viewed by others
Introduction
Religion plays an integral part in the lives of adolescent patients in the United States (Lippman and McIntosh 2010). In the National Study of Youth and Religion, 84 % of adolescents aged 13–17 expressed a strong belief in God and half reported that their religious faith is important in making major life decisions (Dowling et al. 2004; Smith and Denton 2005). Girls report higher levels of religiosity than boys (Le et al. 2007). Data from the National Longitudinal Study of Adolescent Health demonstrated how the importance of religion in adolescents’ lives is consistently related to better family relations (Regnerus and Burdett 2006). African American adolescents show higher levels of religious involvement than white adolescents (Le et al. 2007; Oser and Gmunder 1991).
Spirituality is one of many ways teens with HIV and their families cope with the burdens of HIV (Krauss et al. 2006; Rotheram-Borus et al. 2006). Spirituality is often a central issue not only for them, but also for their families (Garvie et al. 2012; Lyon et al. 2001, 2011). Surveyed HIV-positive teens rated themselves as religious/spiritual, 68 % (Garvie et al. 2012) and reported regular attendance at religious services, 72 %; and religions/spirituality helped 80 % face their fears.
Religious beliefs can increase spiritual distress. HIV-positive teens were more likely to report “God abandoned me,” than HIV-negative teens (Bernstein et al. 2009, 2012). The belief HIV was a punishment from God was associated with poor medication adherence among HIV-positive teens (Lyon et al. 2011).
Religion may protect youth from risky behaviors (McCree et al. 2003; Rostosky et al. 2003; Sinha et al. 2007), particularly young transgender women (Dowshen et al. 2011) and young African American men who have sex with men (Foster et al. 2011).
For adults with HIV, spirituality is associated with mental and physical health (Cotton et al. 2005, 2009; Finocchario-Kessler et al. 2011; Kudel et al. 2011; Ironson et al. 2006; Udell et al. 2011) and protection from depression (Ciesla and Roberts 2001; Perez et al. 2009). Depression is linked with accelerated disease progression and lower survival time (Leserman 2003). Spiritual struggle may increase distress (Pargament et al. 2001, 2004; Lee et al. 2010), disease progression (Ironson et al. 2002) and even mortality (Pargament et al. 2001, 2004), while positive spiritual beliefs may influence well-being, particularly at the end-of-life (Tarakeshwar et al. 2006).
Few research studies have evaluated spirituality or religion among teens with HIV with their families (Lyon et al. 2011). Rather family studies focus on intergenerational transmission of spirituality (Miller 2005); the adolescent perspective on their spiritual development (Rew et al. 2007); interviews with families (Loser et al. 2008); or exploration of conceptual models of how religion may shape family bonds (Mahoney 2010).
We examined spiritual well-being, operationally defined as faith, meaning and purpose (FACIT-SP: Peterman et al. 2002), among primarily African American adolescents living with HIV and their families. We hypothesized that: (a) adolescent and their family’s spirituality would be positively associated; (b) high spirituality would protect adolescents and families from depression and anxiety; and (c) high spirituality would be associated with higher quality of life (QOL) in HIV-positive adolescents over time.
Methods
Participants and Procedures
Participants were recruited/enrolled between July 1, 2006 and May 31, 2008. Adolescents were between 14 and 21 years old, not in foster care, had a legal guardian (if between ages 14–17) or family member (if age 18 or older). “Family” is defined here as the legal guardian or chosen surrogate decision-maker. Exclusion criteria were severe depression, psychosis, suicidality, homicidality, dementia or developmental delay in either HIV+ adolescents or their families.
A sample of 40 adolescents and 40 family members (Total N = 80) completed the Spiritual Well-Being Scale of the Functional Assessment of Chronic Illness Therapy-Version 4 (FACIT-Sp-EX-4), the Beck Depression Inventory-II, the Beck Anxiety Inventory and the Pediatric Quality of Life Inventory, at baseline and 3-month post-intervention. Data were collected as part of a two-site, two-armed randomized controlled clinical trial, which received Institutional Review Board (IRB) approval at both sites. Informed consent/assent was obtained.
Detailed methods are reported elsewhere (Lyon et al. 2009a, b, 2010). Those relevant to this report are below. Initially demographic and health characteristics were collected from chart review and directly from the participants. Questionnaires were orally administered separately by a trained research assistant who recorded participants responses to control for literacy.
Spiritual Well-being
Spiritual Well-Being Scale of the Functional Assessment of Chronic Illness Therapy-Version 4 (Peterman et al. 2002). The FACIT-Sp-Ex-4 was used to investigate spirituality. It is a 23-item scale which assesses faith (comfort and strength in one’s belief) and meaning/peace (sense of meaning, purpose, and peacefulness in life). The FACIT-Sp-Ex 4 exhibits good internal reliability and convergent validity. Validation samples were outpatients with HIV and cancer.
Psychological Adjustment
Beck Depression Inventory-II (BDI: Beck et al. 1996). Administered individually to both adolescent and the family, the BDI-II is a 21-item self-report measure to assess the presence of symptoms of depression and severity of symptoms reported. It has shown good reliability and high content, construct, and factorial validity and is appropriate for children and adolescents >13 years of age. The Beck Anxiety Index (BAI: Beck and Steer 1993) is a 21-item measure assessing severity of subjective, somatic, and panic-related symptoms of anxiety. The BAI has demonstrated good reliability and validity in individuals aged 17–80. We extended to a younger age range for this study to allow for consistency of data collected by a single measure of anxiety.
Health-Related Quality of Life
The Pediatric Quality of Life Inventory™ 4.0 (PedsQL™ 4.0) (Varni et al. 1999, 2001, 2003; Varni and Limbers 2009) is a 23-item modular instrument designed to measure health-related quality of life (HRQOL) in adolescents. Validity was demonstrated using the known-groups method, correlations with indicators of morbidity and illness burden, and factor analysis. This measure has the strongest norms, validity, and reliability of available health-related QOL measures for adolescents.
Statistical Analysis
Data were analyzed using Stata 10.0 (StataCorp, College Station, Texas 77845 USA). Descriptive statistics including frequencies, means ± standard deviations and 95 % confidence intervals were developed to describe the study dyads. Analyses of Covariance were used to test for differences in post-intervention levels of spirituality, depression, anxiety and QoL, while statistically controlling for baseline levels.
We used weighted κ statistics to assess chance-adjusted item congruence across adolescent/family dyads. For these analyses, 5-point Likert scales were collapsed to 3-point Likert scales to reduce the problem of empty cells. The item, HIV is a punishment from God, was added for this study and is not part of the FACIT-SP-EX-4. This item was used to generate future hypotheses.
Results
Participants
Baseline adolescent and family characteristics are presented in Table 1. Adolescent participant mean age was 16 years, 40 % were male, 93 % were African American, 68 % had perinatal HIV infection, 40 % were asymptomatic, and 30 % had an AIDS diagnosis. Of 40 dyads randomized after baseline assessment, two were excluded from analyses, because they never started the intervention. Analyses were based on 38 dyads (N = 76) who completed the 3-month follow-up. No adverse events occurred, nor were there any missing data.
Spiritual Well-being Among HIV-Infected Adolescents and Their Families
There were statistically significantly higher levels of spirituality in family members than in adolescents at baseline and these differences persisted at the 3-month assessment (Total Mean Scaled Scores (SS) at Baseline: Surrogate = 103.52 (SD = 8.5) versus Adolescent 90.69 (SD = 13.4); 3-month follow-up: Surrogate = 102.02 (SD = 11.1) versus Adolescent 92.82 (SD = 16.1), p = 0.07); (Meaning/Peace subscale Mean SS: Family = 51.6 vs. Adolescent 48.6 (SD = 7.36), p = 0.33); (Faith subscale Mean SS: Family = 44.6 vs. Adolescent 45.0 (SD = 8.17), p = 0.57). We decided to examine the baseline FACIT-SP-EX data collected prior to the intervention, to eliminate an intervention effect found in our earlier study and reported elsewhere, which increased the sense of purpose of adolescents in the HLC group on the FACIT-SP-EX.
Table 2 shows item congruence ranked from most to least congruent. Two areas of substantial congruence were identified. Except for a single instance of disagreement, all of the dyads (97.3 %) agreed they had “a reason for living”, all (97.3 %) disagreed that “life lacks meaning/purpose.” A κ statistic could not be obtained due to a lack of variance in their responses, that is very high agreement.
There was moderate congruence with the statement “Do you believe your HIV (your child’s HIV) is God’s punishment” (κ = 0.4089; p = 0.0012) with 1 dyad endorsing this and 32 dyads disagreeing. There was fair congruence on only one item “Feeling a sense of harmony” (κ = 0.3285; p = 0.0011) with 25 dyads agreeing with this statement while 2 dyads disagreed.
Showing only slight congruence were: “I have trouble feeling peace of mind”; “I find comfort in faith or spiritual beliefs”; “I find strength in faith or spiritual beliefs”; “Things will be o.k.”; “I feel forgiven”; and “Appreciation for natural beauty”. Of note on “I feel connected to a higher power or God”, 22 dyads were in agreement and no dyads endorsed not at all. Other adolescents endorsed not at all (n = 8) or some what (n = 5), while their family member endorsed quite a bit/very much (n = 13). With respect to “I feel connected to people,” 17 dyads were in agreement and one dyad endorsed not at all, while other adolescents endorsed not at all (n = 4) and or somewhat (n = 9), but their families endorsed quite a bit/very much (n = 13).
Showing poor congruence with adolescents consistently responding in the opposite direction of their family (κ < 0.00), that is in each instance, adolescents were less likely to agree with the statement and their family members more likely to agree with the statement: “I feel peaceful;” “Life is productive;” “I feel a sense of purpose;” “I am able to reach deep into myself;” “My/my child’s illness strengthened my faith or spiritual beliefs;” “I feel loved;” “I feel love for others;” “I am able to forgive others;” “I feel a sense of thankfulness;” “I feel a sense of thankfulness for what others bring;” “I feel hopeful;” “I feel compassion for others”.
An exploratory analysis was conducted of correlates of adolescent responses to “I am able to forgive others for any harm they have ever caused me,” where adolescents reported not at all (n = 11) or somewhat (n = 4), yet family reported quite a bit/very much (n = 15). No evidence was found that adolescent forgiveness was associated with mode of transmission (behavioral vs. perinatal) (Fisher’s exact test, p = 0.488), stage of illness (Fisher’s exact test, p = 0.833) or adherence to Highly Active Antiretroviral Therapy (F test, p = 0.522). However, with respect to adherence, which was measured using a visual analog scale of percentage of time they took their meds in the past month, those endorsing Not at all/A Little Bit (n = 6) for forgiving others had a Mean adherence score of 79 % [Standard Deviation (SD) = 22)]; those endorsing Somewhat (n = 13) had Mean adherence of 83 % (SD = 17); and those endorsing Quite a Bit/Very Much (n = 13) had Mean adherence of 89 % (SD = 18). Although adherence increased with forgiveness of others, this was not statistically significant.
Was Spirituality at Baseline Assessment Protective at 3-month Post-intervention?
In multiple regression analyses, controlling for baseline levels of spirituality at post-intervention 3-month follow-up, higher adolescent spirituality was associated with lower depression (p = 0.002) and lower anxiety (p = 0.013), while stage of illness, represented by CDC classification for HIV (Centers for Disease Control and Prevention 1992), was not associated (p = 0.768). Family spirituality was not associated family depression (p = 0.987) or anxiety (p = 0.535). Gender did not significantly differ in spirituality, depression, or anxiety for either families or adolescents.
Spiritual Well-being and Psychological Adjustment at 3-Month Post-intervention
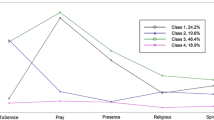
A strong negative relationship existed between scores on the BDI-II and the FACIT-Spirituality (p = 0.002) (Fig. 1), as spirituality scores increased, depression scores decreased. Likewise, there was a strong negative relationship between scores on the BAI and on the FACIT-Spirituality, as spirituality increased, anxious mood decreased for adolescents (Fig. 2). There were not statistically significant associations for families between anxiety and spirituality.
Spiritual Well-being and Quality of Life at 3-Month Post-intervention
Controlling for baseline levels, levels of QOL at 3 months were associated with higher spirituality. This relationship achieved statistical significance for Total Score (p = 0.017) (Fig. 3), Emotional (p = 0.008) (Fig. 4) and Social (p = 0.013) (Fig. 5) subscale scores. There was no such relationship with the school or physical subscale scores.
Discussion
This is the first study to examine congruence in spiritual beliefs between adolescents with HIV and their families. Also unique is the use of a prospective, longitudinal, multi-level design with a valid and reliable measure of spirituality. Among HIV-positive adolescents and their families, there was almost unanimous agreement that life is worth living and that life has meaning and purpose from the outset. However, contrary to our hypotheses, the majority of adolescents’ item responses were not congruent with that of their family member, likely reflecting generational differences. These differences would have been hidden if only the means of the sample were examined, rather than item analysis.
Perhaps the most important difference was that many adolescents find it hard to forgive others harm that was caused them, while the inverse was true for their families. Clinically, this finding may reflect a core spiritual struggle for HIV-positive adolescents, to forgive or not forgive the “other” who was the source of their HIV transmission. Adolescents likely need help working through their anger toward those who transmitted the virus to them, thereby minimizing the significant social isolation families and teens with HIV experience (Abramovitz et al. 2009).
Lack of forgiveness in teens is associated with depression in adolescent psychiatric outpatients (Dew et al. 2008). If anger at the other is turned back on self, a mechanism of depression (Abbas 2002; Leichsenring et al. 2004), adolescents may be less likely to adhere to treatment regimens. Forgiveness of others for the harm done to them is an area not well studied (Gorsuch and Hao 1993; Thompson et al. 2005; Maio et al. 2008), yet may have implications for treatment and medication adherence. Although we found no statistically significant association between forgiveness of others and Highly Active Antiretroviral Treatment (HAART) adherence, likely due to the small sample size, there was a trend suggesting that as forgiveness increased, adherence to HAART increased. This would be consistent with the recent finding that view of God as a benevolent and forgiving versus punishing and judgmental has been found to predict HIV progression in adults (Ironson et al. 2011). Future research should examine whether the construct of forgiveness of others or a forgiving God is an underlying pathway to nonadherence to HAART which in turn influences disease progression.
Also noteworthy, were the low levels of adolescents’ reports of feeing a sense of thankfulness or a sense of thankfulness for what others bring, in contrast to their families. Having a grateful outlook has been found to be highly associated with psychological and physical well-being (Emmons and McCullough 2003). Developing a sense of gratitude is a potential source of resilience and possible target for future interventions, consistent with positive psychology (Froh et al. 2010).
Consistent with studies of adults with HIV/AIDS (Cotton et al. 2006; Le et al. 2007; Sowell et al. 2000) and healthy adolescents (Cotton et al. 2009; Perez et al. 2009; Wong et al. 2006), as hypothesized, spirituality among adolescents with HIV was associated with fewer symptoms of depression and anxiety and enhanced quality of life. The null finding for families is likely related to very high levels of spirituality in families, creating “ceiling effects.”
Contrary to other studies, we did not find that spirituality varied as a function of age, gender, race, or stage of illness (Pargament 2002; Perez et al. 2009). One plausible explanation is that the combination of living with a life-threatening illness and being African American minimized such differences in this sample. Alternatively, selection bias may account for this finding, that is people who were willing to participate in a study which required discussing death and dying were more likely to be spiritual, regardless of demographic differences.
Limitations include all measures were self-reported. Multiple assessment methods of anxiety and depressive symptoms (Kazdin 1994) would have strengthened the outcomes, yet increased participant burden. Participants with severe levels of depression were excluded from the study, decreasing the possibility of finding significant differences due to “floor effects.” We had only one measure of spirituality, the FACIT-Sp-Ex-4 which was designed as a spiritual quality of life measure. We did not examine how the religious community may have provided social support or, to the contrary, isolated participants. Finally, the sample size was small, not allowing for further item analysis and limiting generalizability beyond our urban, primarily African American adolescents.
Despite these limitations, significant strengths include a prospective randomized controlled clinical trial with intention to treat design and a dyadic analysis of adolescent/family responses to a standardized spirituality measure. Retention was excellent. We interviewed participants individually in private and included instruction that should lessen the tendency toward “socially desirable” responding. The longitudinal design of this study permitted an examination of spirituality over time.
Conclusion
The Centers for Disease Control and Prevention (CDC) have recognized the importance of partnering with communities of faith in addressing the HIV epidemic, as religious institutions may be in a unique position to intervene with youth on an individual and community level (CDC 2006). Efforts are now underway to build capacity to develop and disseminate a religiously appropriate tool kit with African American churches (Berkley-Patton et al. 2012). Integrating spiritual practice into HIV services may diminish behaviors associated with the transmission of HIV to others, while improving the quality of life and physical health of HIV-infected youth, particularly among African American sexual minority youth (Foster et al. 2011). Regular screening of youth with HIV for spiritual or religious needs and identifying sources of religious or spiritual support should be a routine part of care, consistent with JACHO and palliative care guidelines (Puchalski et al. 2009).
Abbreviations
- FACE:
-
Family-centered advance care planning
- QOL:
-
Quality of life
- HIV:
-
Human immunodeficiency virus
- FACIT-Sp-Ex:
-
Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being, Expanded Version
- IRB:
-
Institutional Review Board
- HLC:
-
Healthy living control
- BDI-II:
-
Beck Depression Inventory-II
- BAI:
-
Beck Anxiety Index
- PedsQL™ 4.0:
-
Pediatric Quality of Life Inventory™ 4.0
- HAART:
-
Highly active antiretroviral therapy
- JCAHO:
-
Joint Commission on Accreditation of Healthcare Organizations
References
Abbas, A. (2002). Intensive short-term dynamic psychotherapy in a private psychiatric office, clinical and cost effectiveness. American Journal Psychotherapy, 56, 225–232.
Abramovitz, S., Koenig, L. J., Chandwani, S., Orban, L., Stein, R., Lagrange, R., et al. (2009). Characterizing social support: Global and specific social support experiences of HIV-infected youth. AIDS Patient Care and STDS, 23, 323–330.
Beck, A. T., & Steer, R. A. (1993). Beck anxiety inventory manual. San Antonio: The Psychological Corporation, Harcourt Brace & Company.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory manual (2nd ed.). San Antonio: The Psychological Corporation, Harcourt Brace & Company.
Berkley-Patton, J., Thompson, C. B., Martinez, D. A., Hawes, S. M., Moore, E., Williams, E., et al. (2012). Examining church capacity to develop and disseminate a religiously appropriate HIV tool kit with African American churches. Journal of Urban Health. 4(7). pii: a006783. doi:10.1101/cshperspect.a006783.
Bernstein, K., D’Angelo, L., & Lyon, M. E. (2012). An exploratory study of HIV+ adolescents’ spirituality: Will you pray with me? Journal of Religion and Health. (Epub 2012 January 19). doi:10.1007/s10943-012-9565-1.
Bernstein, K., Lyon, M. E., & D’Angelo, L. J. (2009). Spirituality and religion in adolescents with and without HIV/AIDS. Journal of Adolescent Health, 44, S25.
Centers for Disease Control and Prevention. (1992). 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR, 41, 1–17.
Centers for Disease Control and Prevention. (2006). CDC executive summary: CDC consultation on faith and HIV prevention.
Ciesla, J., & Roberts, J. (2001). Meta-analysis of the relationship between HIV infection and risk of depressive disorders. American Journal of Psychiatry, 158, 725–730.
Cotton, S., Kudel, I., Roberts, Y. H., Pallerla, H., Tsevat, J., Succop, P., et al. (2009). Spiritual well-being and mental health outcomes in adolescents with or without inflammatory bowel disease. Journal of Adolescent Health, 44, 485–492.
Cotton, S., Larkin, E., Hoopes, A., et al. (2005). Impact of adolescent spirituality on depressive symptoms and health behaviors. Journal of Adolescent Health, 36, 529.
Cotton, S., Puchalski, C. M., Sherman, S. N., Mrus, J. M., Peterman, A. H., Feinberg, J., et al. (2006). Spirituality and religion in patients with HIV/AIDS. Journal of General Internal Medicine, 21(Suppl 5), S5–S13.
Dew, R. E., Daniel, S. S., Goldstone, D. B., & Koenig, H. G. (2008). Religion, spirituality, and depression in adolescent psychiatric outpatients. Nervous Mental Diseases, 196, 247–251.
Dowling, E. M., Gestsdottir, S., Anderson, P. M., von Eye, A., Almerigi, J., & Lerner, R. M. (2004). Structural relations among spirituality, religiosity, and thriving in adolescence. Applied Developmental Science, 8, 7–16.
Dowshen, N., Forke, C. M., Johnson, A. K., Kuhns, L. M., Rubin, D., & Garofalo, R. (2011). Religiosity as a protective factor against HIV risk among young transgender women. Journal of Adolescent Health, 48, 410–414.
Emmons, R. A., & McCullough, M. E. (2003). Counting blessings versus burdens: An experimental investigation of gratitude and subjective well being in daily life. Journal of Personality and Social Psychology, 84, 377–389.
Finocchario-Kessler, S., Catley, D., Berkley-Patton, J., Gerkovich, M., Williams, K., Banderas, J., et al. (2011). Baseline predictors of ninety percent or higher antiretroviral therapy adherence in a diverse urban sample: The role of patient autonomy and fatalistic religious beliefs. AIDS Patient Care and STDS, 25, 103–111.
Foster, M. L., Arnold, E., Rebchook, G., & Kegeles, S. M. (2011). ‘It’s my inner strength’: Spirituality, religion and HIV in the lives of young African American men who have sex with men. Culture, Health & Sexuality, 13, 1103–1117.
Froh, J. J., Emmons, R. A., Card, N. A., Bono, G., & Wilson, J. A. (2010). Gratitude and the reduced costs of materialism in adolescents. Journal of Happiness Studies, 12, 289–302.
Garvie, P. A., He, J., Wang, J., D’Angelo, L. J., & Lyon, M. E. (2012). An exploratory survey of end-of-life attitudes, beliefs and experiences of adolescents with HIV/AIDS and their families. Journal of Pain and Symptom Management, 44(3), 373–385.e29. (Epub 2012 Jul 7).
Gorsuch, R. L., & Hao, J. Y. (1993). Forgiveness: An exploratory factor analysis and its relationship to religious variables. Review of Religious Research, 34, 333–347.
Ironson, G., Solomon, G. G., Balbin, E. G., O’Cleirigh, C., George, A., Kumar, M., et al. (2002). The Ironson-Woods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Annals of Behavioral Medicine, 24, 34–48.
Ironson, G., Stuetzle, R., & Fletcher, M. A. (2006). An increase in religiousness/spirituality occurs after HIV diagnosis and predicts slower disease progression over 4 years in people with HIV. Journal of General Internal Medicine, 21(Suppl 5), S62–S68.
Ironson, G., Stuetzle, R., Kronson, D., Balbin, E., Kremer, H., George, A., et al. (2011). View of God as benevolent and forgiving or punishing and judgmental predicts HIV disease progression. Journal of Behavioral Medicine, 34, 414–425.
Kazdin, A. E. (1994). Informant variability in the assessment of childhood depression. In W. M. Reynolds & H. F. Johnson (Eds.), Handbook of depression in children and adolescents: Issues in clinical child psychology (pp. 249–271). New York: Plenum Press.
Krauss, B. J., Godfrey, C., O’Day, J., Freidin, E., & Kaplan, R. (2006). Learning to live with an epidemic: Reducing stigma and increasing safe and sensitive socializing with persons with HIV. In M. Lyon & J. D’Angelo (Eds.), Teenagers HIV and AIDS: Insights from youths living with the virus (pp. 83–103). London: Praeger Press.
Kudel, I., Cotton, S., Szaflarski, M., Holmes, W. C., & Tsevat, J. (2011). Spirituality and religiosity in patients with HIV: A test and expansion of a model. Annals of Behavioral Medicine, 41, 92–103.
Le, T. N., Tov, W., & Taylor, J. (2007). Religiousness and depressive symptoms in five ethnic adolescent groups. International Journal for the Psychology of Religion, 17, 209–232.
Lee, C. C., Czaja, S. J., & Schulz, R. (2010). The moderating influence of demographic characteristics, social support, and religious coping on the effectiveness of a multicomponent psychosocial caregiver intervention in three racial ethnic groups. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 65B, 185–194.
Leichsenring, F., Rabung, S., & Leibing, E. (2004). The efficacy of short-term psychodynamic psychotherapy in specific psychiatric disorders. A meta-analysis. Archives of General Psychiatry, 61, 1208–1216.
Leserman, J. (2003). HIV disease progression: Depression, stress and possible mechanisms. Biological Psychiatry, 54, 295–306.
Lippman, L. H., & McIntosh, H. (2010). The demographics of spirituality and religiosity among youth: International and U. S. Patterns. Child Trends Research Brief. September 2010; Pub#2010-21 www.childtrends.org.
Loser, R. W., Klein, S. R., Hill, E. J., & Dollahite, D. C. (2008). Religion and the daily lives of LDS families: An ecological perspective. Family and Consumer Sciences Research Journal, 37, 52–70.
Lyon, M. E., Garvie, P. A., Briggs, L., He, J., D’Angelo, L., & McCarter, R. (2009a). Development, feasibility and acceptability of the family-centered (FACE) advance care planning intervention for adolescents with HIV. Journal of Palliative Medicine, 12, 363–372.
Lyon, M. E., Garvie, P. A., Briggs, L., He, J., Malow, R., D’Angelo, L. J., et al. (2010). Is it safe? Talking to teens with HIV/AIDS about death and dying: A 3-month evaluation of FAmily CEntered (FACE) advance care planning—anxiety, depression quality of life. HIV/AIDS—Research Palliative Care, 2, 1–11.
Lyon, M. E., Garvie, P. A., Kao, E., Briggs, L., He, J., Malow, R., et al. (2011). Spirituality in HIV infected adolescents and their families: FAmily Centered (FACE) advance care planning and medication adherence. Journal of Adolescent Health, 48, 633–636.
Lyon, M. E., Garvie, P. A., McCarter, R., Briggs, L., He, J., & D’Angelo, L. (2009b). Who will speak for me? Improving end-of-life decision-making for adolescents with HIV and their families. Pediatrics, 123, e1–e8.
Lyon, M. E., Townsend-Akpan, C., & Thompson, A. (2001). Spirituality and end-of-life care for an adolescent with AIDS. AIDS Patient Care and STDs, 15, 555–560.
Mahoney, A. (2010). Religion in families, 1999–2009: A relational spirituality framework. Journal of Marriage and Family, 72, 805–827.
Maio, G. R., Thomas, G., & Fincham, F. D. (2008). Unraveling the role of forgiveness in family relationships. Journal of Personality and Social Psychology, 94, 307–319.
McCree, D. H., Wingood, G. M., DiClemente, R. D., Harrington, S., & Harrington, K. F. (2003). Religiosity and risky sexual behavior in African-American adolescent females. Journal of Adolescent Health, 33, 2–8.
Miller, B. A. (2005). Intergenerational transmission of religiousness and spirituality. In W. R. Miller & H. D. Delaney (Eds.), Judeo-Christian perspectives on psychology: Human nature, motivation and change (pp. 227–244). Washington, DC: American Psychological Association.
Oser, F., & Gmunder, P. (1991). Religious judgment: A developmental perspective. Birmingham: AL Religious Education Press.
Pargament, K. I. (2002). The bitter and the sweet: An evaluation of the costs and benefits of religiousness. Psychological Inquiry, 13, 168–181.
Pargament, K. I., Koenig, H. G., Tarakeshwar, N., & Hahn, J. (2001). Religious struggle as a predictor of mortality among medically ill elderly patients. Archives of Internal Medicine, 161, 1881–1885.
Pargament, K. I., Koenig, H. G., Tarakeshwar, N., & Hahn, J. (2004). Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. Journal of Health Psychology, 9, 713–730.
Perez, J. E., Little, T. D., & Henrich, C. C. (2009). Spirituality and depressive symptoms in a school-based sample of adolescents: A longitudinal examination of mediated and moderated effects. Journal of Adolescent Health, 44, 380–386.
Peterman, A. H., Fitchett, G., Brady, M., Hernandez, L., & Cella, D. (2002). Measuring spiritual well-being in people with cancer: The Functional Assessment of chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp). Annals of Behavioral Medicine, 24, 49–58.
Puchalski, C., Ferrell, B., Virani, R., Otis-Green, S., Baird, P., Bull, J., et al. (2009). Improving the quality of spiritual care as a dimension of palliative care: The report of the consensus conference. Journal of Palliative Medicine, 12(10), 885–904.
Regnerus, M. D., & Burdett, A. (2006). Religious change and adolescent family dynamics. The Sociological Quarterly, 47, 175–194.
Rew, L., Wong, J., Torres, R., & Howell, E. (2007). Older adolescents’ perceptions of the social context, impact, and development of their spiritual/religious beliefs and practices. Issues in Comprehensive Pediatric Nursing, 30, 55–68.
Rostosky, S. S., Regnerus, M. D., & Wright, M. L. (2003). Coital debut: The role of religiosity and sex attitudes in ADD Health Survey. The Journal of Sex Research, 40, 358–367.
Rotheram-Borus, M. J., Stein, J. A., & Lester, P. (2006). Adolescent adjustment over six years in HIV-affected families. Journal of Adolescent Health, 39, 174–182.
Sinha, J. W., Cnaan, R. A., & Gelles, R. J. (2007). Adolescent risk behaviors and religion: Findings from a national study. Journal of Adolescence, 30, 231–249.
Smith, C., & Denton, M. L. (2005). Soul searching: The religious and spiritual lives of American teenagers. New York: Oxford University Press.
Sowell, R., Moneyham, L., Hennessy, M., Guilory, J., Demi, A., & Seals, B. (2000). Spiritual activities as a resistance resource for women with human immunodeficiency virus. Annual Review of Nursing Research, 49(2), 73–82.
Tarakeshwar, N., Vanderwerker, L. C., Paulk, E., Pearce, M. J., Kasl, S. V., & Prigerson, H. G. (2006). Religious coping is associated with the quality of life of patients with advanced cancer. Journal of Palliative Medicine, 9, 646–657.
Thompson, L. Y., Snyder, C. R., Hoffman, L., Michael, S. T., Rasmussen, H. N., Billings, L. S., et al. (2005). Dispositional forgiveness of self, others, and situations. Journal of Personality, 73, 313–360.
Udell, W., Donenberg, G., & Emerson, E. (2011). The impact of mental health problems and religiosity on African-American girls’ HIV risk. Cultural Diversity and Ethnic Minority Psychology, 17, 217–224.
Varni, J. W., Burwinkle, T. M., Seid, M., & Skarr, D. (2003). The PedsQL™ 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambulatory Pediatrics, 3, 329–341. Available at http://www.pedsql.org.
Varni, J. W., & Limbers, C. A. (2009). The Pediatric Quality of Life Inventory: Measuring pediatric health-related quality of life from the perspective of children and their parents. Pediatric Clinics of North America, 56, 843–863.
Varni, J. W., Seid, M., & Kurtin, P. S. (2001). PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Medical Care, 39, 800–812.
Varni, J. W., Seid, M., & Rode, C. A. (1999). The PEDSQL: Measurement model for the pediatric quality of life inventory. Medical Care, 37, 126–139.
Wong, Y. J., Rew, L., & Slaikeu, K. D. (2006). A systematic review of recent research on adolescent religiosity/spirituality and mental health. Issues Mental Health Nursing, 27, 161–183.
Acknowledgments
The study was funded by grant 5R34MH072541-03 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. We thank our families for their participation.
Conflict of interest
The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was completed while Dr. Garvie was a faculty member at SJCRH. Collaboration on this project is continued as a voluntary consultant.
This trial has been registered at www.clinicaltrials.gov Identifier #NCT00723476.
Rights and permissions
About this article
Cite this article
Lyon, M.E., Garvie, P., He, J. et al. Spiritual Well-Being Among HIV-Infected Adolescents and Their Families. J Relig Health 53, 637–653 (2014). https://doi.org/10.1007/s10943-012-9657-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-012-9657-y