Abstract
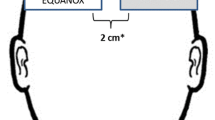
We assessed the accuracy of Masimo O3™ regional cerebral oxygen saturation (rSO2) readings by comparing them with reference values and evaluated the relationship between rSO2 and somatic tissue oxygen saturation (StO2) in children undergoing cardiac surgery. After anesthesia induction, pediatric sensors were applied to the forehead and foot sole, and rSO2 and StO2 values were monitored continuously. Before cardiopulmonary bypass (CPB), FIO2 was set to 0.2, 0.5, and 0.8 serially every 15 min. After CPB, FIO2 was reversed. The reference values (SavO2) were calculated by combining arterial (SaO2) and central venous oxygen saturation (SvO2) readings from the arterial and central lines, respectively (0.7 \(\times\) SvO2 + 0.3 \(\times\) SaO2). In total, 265 pairs of rSO2/StO2 and SavO2 from 49 patients were analyzed. The bias, standard deviation (SD), standard error (SE), and root mean squared error (RMSE) of rSO2 were 2.6%, 4.5%, 0.3%, and 4.3%, respectively. The limits of agreement ranged from -6.3% to 11.6%. Trend accuracy analysis yielded a relative mean error of -1.4%, with an SD of 4.3%, SE of 0.2%, and RMSE of 3.9%. According to multiple linear regression analysis, the application of CPB, FIO2, Hb level, and tip location of the central venous catheter influenced the bias (all P < 0.05). Furthermore, the correlation between rSO2 and StO2 was weak (r = 0.254). rSO2 readings by the Masimo O3™ device and pediatric sensor had good absolute and trending accuracies with respect to the calculated reference values in children undergoing cardiac surgery. rSO2 and StO2 cannot be used interchangeably.
Clinical trial registration http://clinicaltrials.gov (number: NCT04208906).




Similar content being viewed by others
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Yao FS, Tseng CC, Ho CY, Levin SK, Illner P. Cerebral oxygen desaturation is associated with early postoperative neuropsychological dysfunction in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18(5):552–8.
Slater JP, Guarino T, Stack J, et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg. 2009;87(1):36–44 (discussion 44-35).
Redford D, Paidy S, Kashif F. Absolute and trend accuracy of a new regional oximeter in healthy volunteers during controlled hypoxia. Anesth Analg. 2014;119(6):1315–9.
DiNardo JA. Cerebral oximetry in children: so NIRS yet so far. Anesth Analg. 2019;128(4):605–6.
Tortoriello TA, Stayer SA, Mott AR, et al. A noninvasive estimation of mixed venous oxygen saturation using near-infrared spectroscopy by cerebral oximetry in pediatric cardiac surgery patients. Paediatr Anaesth. 2005;15(6):495–503.
Ginther R, Sebastian VA, Huang R, et al. Cerebral near-infrared spectroscopy during cardiopulmonary bypass predicts superior vena cava oxygen saturation. J Thorac Cardiovasc Surg. 2011;142(2):359–65.
Benni PB, MacLeod D, Ikeda K, Lin HM. A validation method for near-infrared spectroscopy based tissue oximeters for cerebral and somatic tissue oxygen saturation measurements. J Clin Monit Comput. 2018;32(2):269–84.
Wu C, Honarmand AR, Schnell S, et al. Age-related changes of normal cerebral and cardiac blood flow in children and adults aged 7 months to 61 years. J Am Heart Assoc. 2016;5(1):e002657.
Weiss M, Dullenkopf A, Kolarova A, Schulz G, Frey B, Baenziger O. Near-infrared spectroscopic cerebral oxygenation reading in neonates and infants is associated with central venous oxygen saturation. Paediatr Anaesth. 2005;15(2):102–9.
Nagdyman N, Ewert P, Peters B, Miera O, Fleck T, Berger F. Comparison of different near-infrared spectroscopic cerebral oxygenation indices with central venous and jugular venous oxygenation saturation in children. Paediatr Anaesth. 2008;18(2):160–6.
Moreno GE, Pilán ML, Manara C, et al. Regional venous oxygen saturation versus mixed venous saturation after paediatric cardiac surgery. Acta Anaesthesiol Scand. 2013;57(3):373–9.
la Cour A, Greisen G, Hyttel-Sørensen S. In vivo validation of cerebral near-infrared spectroscopy: a review. Neurophotonics. 2018;5(4):040901.
Schell RM, Cole DJ. Cerebral monitoring: jugular venous oximetry. Anesth Analg. 2000;90(3):559–66.
Lynch JM, Buckley EM, Schwab PJ, et al. Noninvasive optical quantification of cerebral venous oxygen saturation in humans. Acad Radiol. 2014;21(2):162–7.
Watzman HM, Kurth CD, Montenegro LM, Rome J, Steven JM, Nicolson SC. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology. 2000;93(4):947–53.
Ikeda K, MacLeod DB, Grocott HP, Moretti EW, Ames W, Vacchiano C. The accuracy of a near-infrared spectroscopy cerebral oximetry device and its potential value for estimating jugular venous oxygen saturation. Anesth Analg. 2014;119(6):1381–92.
Weiss M, Dullenkopf A, Kolarova A, Schulz G, Frey B, Baenziger O. Near-infrared spectroscopic cerebral oxygenation reading in neonates and infants is associated with central venous oxygen saturation. Pediatr Anesth. 2005;15(2):102–9.
Kreeger RN, Ramamoorthy C, Nicolson SC, et al. Evaluation of pediatric near-infrared cerebral oximeter for cardiac disease. Ann Thorac Surg. 2012;94(5):1527–33.
la Cour A, Greisen G, Hyttel-Sorensen S. In vivo validation of cerebral near-infrared spectroscopy: a review. Neurophotonics. 2018;5(4):040901.
Nasr VG, Bergersen LT, Lin HM, et al. Validation of a Second-Generation Near-Infrared Spectroscopy Monitor in Children With Congenital Heart Disease. Anesth Analg. 2019;128(4):661–8.
Michel-Macías C, Morales-Barquet DA, Martínez-García A, Ibarra-Ríos D. Findings From Somatic and Cerebral Near-Infrared Spectroscopy and Echocardiographic Monitoring During Ductus Arteriosus Ligation: Description of Two Cases and Review of Literature. Front Pediatr. 2020;8:523.
Ortmann LA, Fontenot EE, Seib PM, Eble BK, Brown R, Bhutta AT. Use of near-infrared spectroscopy for estimation of renal oxygenation in children with heart disease. Pediatr Cardiol. 2011;32(6):748–53.
Funding
None.
Author information
Authors and Affiliations
Contributions
J-HL: This author helped in the study design, patient recruitment, data collection, data analysis, and writing of the manuscript. ISS: This author helped in the patient recruitment, data analysis, and data collection, and writing of the manuscript. PK: This author helped in the study design, patient recruitment, and data collection. S-HJ: This author helped in the patient recruitment, data analysis, and data collection. Y-EJ: This author helped in the study design, and data collection. E-HK: This author helped in the patient recruitment, data analysis, and data collection. H-SK: This author helped in the study design, data collection and data analysis. J-TK: This author helped in the study design, patient recruitment, data collection, data analysis, and writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (H1911-099-1081; date of approval: 3rd January, 2020).
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, JH., Song, IS., Kang, P. et al. Validation of the Masimo O3™ regional oximetry device in pediatric patients undergoing cardiac surgery. J Clin Monit Comput 36, 1703–1709 (2022). https://doi.org/10.1007/s10877-022-00815-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-022-00815-3