Abstract
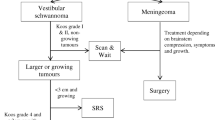
In intraoperative neuromonitoring (IONM), facial nerve motor function (FaNMF) is assessed by facial muscle corticobulbar motor evoked potentials (FMcoMEP). Mostly only amplitude decrease is used as warning criterion. We related a refined criterion for FMcoMEP consisting of a bilateral final-to-baseline motor threshold ratio with standard criteria and postoperative FaNMF. 79 patients (45 females; 48 ± 16 years) undergoing IONM-guided cerebellopontine angle tumor surgery were retrospectively analyzed. An intraoperative final-to-baseline motor threshold increase ≥ 20% ipsi- versus contralaterally (bFBMT20) was correlated to postoperative FaNMF at day 1 (D1), 7 (D7) and 3 months (3 M). An ipsilateral-only final-to-baseline motor threshold increase ≥ 20 mA (iAMT20) and amplitude decrement ≥ 50% (iAR50) served as reference. Tumors included vestibular schwannomas (68%), meningiomas (19%) and others (13%). Mean tumor diameter was 2.7 ± 1.1 cm. Postoperatively, HB-increase ≥ 2 was seen in 27% (D1), 17% (D7), and 6% (3 M) of patients, respectively. FMcoMEP were obtained in 75/79 cases. Pathological bFBMT20, iAMT20 and iAR50 were seen in 17, 17, and 46 cases, respectively. Area under the ROC curve for bFBMT20 (iAMT20) was 0.894 (0.868) at D1; 0.903 (0.822) at D7 and 0.941 (0.959) at 3 M. iAR50 performed worse at all time points. Diagnostic odds ratios were highest for bfBMT20 compared to iAMT20 and iAR50 for D1 (172.5 vs. 8.7 vs. 0.45) and D7 (51.4 vs. 6.1 vs. 0.8). The refined parameter bFBMT20 provides a valuable contribution to the prognostic assessment of FaNMF. Due to its bihemispheric character, it might thus circumvent false-positive events which affect FMcoMEP bilaterally.


Similar content being viewed by others
References
Goldbrunner RH, Schlake HP, Milewski C, Tonn JC, Helms J, Roosen K. Quantitative parameters of intraoperative electromyography predict facial nerve outcomes for vestibular schwannoma surgery. Neurosurgery. 2000;46(5):1140–6 (discussion 1146–1148).
Acioly MA, Liebsch M, de Aguiar PH, Tatagiba M. Facial nerve monitoring during cerebellopontine angle and skull base tumor surgery: a systematic review from description to current success on function prediction. World Neurosurg. 2013;80(6):e271–300. https://doi.org/10.1016/j.wneu.2011.09.026.
Dong CC, Macdonald DB, Akagami R, Westerberg B, Alkhani A, Kanaan I, Hassounah M. Intraoperative facial motor evoked potential monitoring with transcranial electrical stimulation during skull base surgery. Clin Neurophysiol. 2005;116(3):588–96. https://doi.org/10.1016/j.clinph.2004.09.013.
Matthies C, Raslan F, Schweitzer T, Hagen R, Roosen K, Reiners K. Facial motor evoked potentials in cerebellopontine angle surgery: technique, pitfalls and predictive value. Clin Neurol Neurosurg. 2011;113(10):872–9. https://doi.org/10.1016/j.clineuro.2011.06.011.
Macdonald DB, Skinner S, Shils J, Yingling C, American Society of Neurophysiological M. Intraoperative motor evoked potential monitoring—a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol. 2013;124(12):2291–316. https://doi.org/10.1016/j.clinph.2013.07.025.
Acioly MA, Liebsch M, Carvalho CH, Gharabaghi A, Tatagiba M. Transcranial electrocortical stimulation to monitor the facial nerve motor function during cerebellopontine angle surgery. Op Neurosurg. 2010;66:ons354–62. https://doi.org/10.1227/01.neu.0000369654.41677.b7.
Acioly MA, Gharabaghi A, Liebsch M, Carvalho CH, Aguiar PH, Tatagiba M. Quantitative parameters of facial motor evoked potential during vestibular schwannoma surgery predict postoperative facial nerve function. Acta Neurochir. 2011;153(6):1169–79. https://doi.org/10.1007/s00701-011-0995-4.
Akagami R, Dong CCJ, Westerberg BD. Localized transcranial electrical motor evoked potentials for monitoring cranial nerves in cranial base surgery. Op Neurosurg. 2005;57:78–85. https://doi.org/10.1227/01.neu.0000163486.93702.95.
Fukuda M, Oishi M, Takao T, Saito A, Fujii Y. Facial nerve motor-evoked potential monitoring during skull base surgery predicts facial nerve outcome. J Neurol Neurosurg Psychiatry. 2008;79(9):1066–70. https://doi.org/10.1136/jnnp.2007.130500.
Liu BY, Tian YJ, Liu W, Liu SL, Qiao H, Zhang JT, Jia GJ. Intraoperative facial motor evoked potentials monitoring with transcranial electrical stimulation for preservation of facial nerve function in patients with large acoustic neuroma. Chin Med J. 2007;120(4):323–5.
Sarnthein J, Hejrati N, Neidert MC, Huber AM, Krayenbuhl N. Facial nerve motor evoked potentials during skull base surgery to monitor facial nerve function using the threshold-level method. Neurosurg Focus. 2013;34(3):E7. https://doi.org/10.3171/2012.12.FOCUS12386.
Bozinov O, Grotzer MA, Sarnthein J. Intraoperative monitoring of facial nerve motor-evoked potentials in children. World Neurosurg. 2015;84(3):786–94. https://doi.org/10.1016/j.wneu.2015.05.008.
Krammer MJ, Wolf S, Schul DB, Gerstner W, Lumenta CB. Significance of intraoperative motor function monitoring using transcranial electrical motor evoked potentials (MEP) in patients with spinal and cranial lesions near the motor pathways. Br J Neurosurg. 2009;23(1):48–55. https://doi.org/10.1080/02688690802563349.
Szelényi A, Hattingen E, Weidauer S, Seifert V, Ziemann U. Intraoperative motor evoked potential alteration in intracranial tumor surgery and its relation to signal alteration in postoperative magnetic resonance imaging. Neurosurgery. 2010;67(2):302–13. https://doi.org/10.1227/01.neu.0000371973.46234.46.
Abboud T, Schaper M, Duhrsen L, Schwarz C, Schmidt NO, Westphal M, Martens T. A novel threshold criterion in transcranial motor evoked potentials during surgery for gliomas close to the motor pathway. J Neurosurg. 2016;125(4):795–802. https://doi.org/10.3171/2015.8.JNS151439.
Samii M, Matthies C. Management of 1000 vestibular Schwannomas (Acoustic Neuromas): the facial nerve-preservation and restitution of function. Neurosurgery. 1997;40(4):684–95. https://doi.org/10.1097/00006123-199704000-00006.
House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93(2):146–7. https://doi.org/10.1177/019459988509300202.
Deletis V, Fernandez-Conejero I, Ulkatan S, Costantino P. Methodology for intraoperatively eliciting motor evoked potentials in the vocal muscles by electrical stimulation of the corticobulbar tract. Clin Neurophysiol. 2009;120(2):336–41. https://doi.org/10.1016/j.clinph.2008.11.013.
Huang X, Xu J, Xu M, Chen M, Ji K, Ren J, Zhong P. Functional outcome and complications after the microsurgical removal of giant vestibular schwannomas via the retrosigmoid approach: a retrospective review of 16-year experience in a single hospital. BMC Neurol. 2017;17(1):18. https://doi.org/10.1186/s12883-017-0805-6.
Deletis V, Urriza J, Ulkatan S, Fernandez-Conejero I, Lesser J, Misita D. The feasibility of recording blink reflexes under general anesthesia. Muscle Nerve. 2009;39(5):642–6. https://doi.org/10.1002/mus.21257.
Müri RM. Cortical control of facial expression. J Comp Neurol. 2016;524(8):1578–85. https://doi.org/10.1002/cne.23908.
Sarnthein J, Bozinov O, Melone AG, Bertalanffy H. Motor-evoked potentials (MEP) during brainstem surgery to preserve corticospinal function. Acta Neurochir (Wien). 2011;153(9):1753–9. https://doi.org/10.1007/s00701-011-1065-7.
Neuloh G, Bogucki J, Schramm J. Intraoperative preservation of corticospinal function in the brainstem. J Neurol Neurosurg Psychiatry. 2009;80(4):417–22. https://doi.org/10.1136/jnnp.2008.157792.
Kodama K, Javadi M, Seifert V, Szelenyi A. Conjunct SEP and MEP monitoring in resection of infratentorial lesions: lessons learned in a cohort of 210 patients. J Neurosurg. 2014;121(6):1453–61. https://doi.org/10.3171/2014.7.Jns131821.
Skinner SA, Holdefer RN. IONM evidence: putting the work and insight of Tellez et al. in context. Clin Neurophysiol. 2016;127(2):1015–7. https://doi.org/10.1016/j.clinph.2015.09.130.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JT received consultant fees from Brainlab, Germany. AS received consultant fees from Inomed, Germany. The consultant fees were not specific for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Greve, T., Wang, L., Thon, N. et al. Prognostic value of a bilateral motor threshold criterion for facial corticobulbar MEP monitoring during cerebellopontine angle tumor resection. J Clin Monit Comput 34, 1331–1341 (2020). https://doi.org/10.1007/s10877-019-00434-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00434-5