Abstract
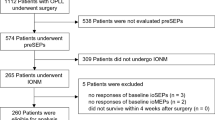
To report the incidence of clinically detectable nerve injuries when utilizing transcranial electrical motor evoked potentials (MEPs) during shoulder arthroplasty. A retrospective review of patients undergoing shoulder arthroplasty with continuous IONM was performed. The criteria for nerve alerts was an 80% amplitude reduction in MEPs. The primary outcome measure was post-operative clinically detectable nerve deficit. An additional retrospective analysis on a subset of cases using an all-or-none (100% amplitude reduction) criterion applied to the deltoid was performed. Two hundred eighty four arthroplasty cases were included. There were no permanent post-operative nerve injuries and two transient nerve injuries (0.7%). MEP alerts occurred in 102 cases (36.2%). Nineteen (6.7%) cases did not have signals return above alert threshold at closure. These cases were significantly associated with post-operative nerve injury (p = 0.03). There were no false negatives, making sensitivity 100% and specificity was 93.9%. In the subset of cases in which an all-or-none criterion was retrospectively applied to just the deltoid, MEP alerts occurred in just 17.9% of cases; specificity improved to 98.0%. We conclude that utilization of the real-time diagnostic MEP data during shoulder arthroplasty aids surgeons in decision making regarding impending peripheral nerve injuries.

Similar content being viewed by others
References
Boardman ND 3rd, Cofield RH. Neurologic complications of shoulder surgery. Clin Orthop Relat Res 1999; 368:44–53.
Lynch NM, Cofield RH, Silbert PL, Hermann RC. Neurologic complications after total shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5(1):53–61.
Nagda SH, Rogers KJ, Sestokas AK, Getz CL, Ramsey ML, Glaser DL, Williams GR Jr. Neer award 2005: peripheral nerve function during shoulder arthroplasty using intraoperative nerve monitoring. J Shoulder Elbow Surg. 2007;16(3 Suppl):S2–S8. https://doi.org/10.1016/j.jse.2006.01.016.
Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78(4):603–16.
Ladermann A, Lubbeke A, Melis B, Stern R, Christofilopoulos P, Bacle G, Walch G. Prevalence of neurologic lesions after total shoulder arthroplasty. J Bone Joint Surg Am. 2011;93(14):1288–93. doi:https://doi.org/10.2106/JBJS.J.00369.
Esmail AN, Getz CL, Schwartz DM, Wierzbowski L, Ramsey ML, Williams GR Jr. Axillary nerve monitoring during arthroscopic shoulder stabilization. Arthroscopy. 2005;21(6):665–71. https://doi.org/10.1016/j.arthro.2005.03.013.
Padberg AM, Bridwell KH. Spinal cord monitoring: current state of the art. Orthop Clin North Am. 1999;30(3):407–33. (viii)
Padberg AM, Russo MH, Lenke LG, Bridwell KH, Komanetsky RM. Validity and reliability of spinal cord monitoring in neuromuscular spinal deformity surgery. J Spinal Disord. 1996;9(2):150–8.
Delaney RA, Freehill MT, Janfaza DR, Vlassakov KV, Higgins LD, Warner JJ. 2014 Neer award paper: neuromonitoring the Latarjet procedure. J Shoulder Elbow Surg. 2014;23(10):1473–80. https://doi.org/10.1016/j.jse.2014.04.003.
Dong CC, Macdonald DB, Akagami R, Westerberg B, Alkhani A, Kanaan I, Hassounah M. Intraoperative facial motor evoked potential monitoring with transcranial electrical stimulation during skull base surgery. Clin Neurophysiol. 2005;116(3):588–96. https://doi.org/10.1016/j.clinph.2004.09.013.
Dong CC, MacDonald DB, Janusz MT. Intraoperative spinal cord monitoring during descending thoracic and thoracoabdominal aneurysm surgery. Ann Thorac Surg. 2002;74(5):S1873–S1876. (discussion S1892–S1878).
MacDonald DB, Al Zayed Z, Khoudeir I, Stigsby B. Monitoring scoliosis surgery with combined multiple pulse transcranial electric motor and cortical somatosensory-evoked potentials from the lower and upper extremities. Spine (Phila Pa 1976). 2003;28(2):194–203. https://doi.org/10.1097/01.BRS.0000041583.59280.24.
Macdonald DB, Skinner S, Shils J, Yingling C, American Society of Neurophysiological Monitoring. Intraoperative motor evoked potential monitoring—a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol. 2013;124 (12):2291–316. https://doi.org/10.1016/j.clinph.2013.07.025.
Raynor BL, Bright JD, Lenke LG, Rahman RK, Bridwell KH, Riew KD, Buchowski JM, Luhmann SJ, Padberg AM. Significant change or loss of intraoperative monitoring data: a 25-year experience in 12,375 spinal surgeries. Spine (Phila Pa 1976). 2013;38(2):E101–E108. https://doi.org/10.1097/BRS.0b013e31827aafb9.
Raynor BL, Padberg AM, Lenke LG, Bridwell KH, Riew KD, Buchowski JM, Luhmann SJ. Failure of intraoperative monitoring to detect postoperative neurologic deficits: a 25-year experience in 12,375 spinal surgeries. Spine (Phila Pa 1976). 2016. https://doi.org/10.1097/BRS.0000000000001531.
Roh MS, Wilson-Holden TJ, Padberg AM, Park JB, Daniel Riew K. The utility of somatosensory evoked potential monitoring during cervical spine surgery: how often does it prompt intervention and affect outcome? Asian Spine J. 2007;1(1):43–7. https://doi.org/10.4184/asj.2007.1.1.43.
Thuet ED, Winscher JC, Padberg AM, Bridwell KH, Lenke LG, Dobbs MB, Schootman M, Luhmann SJ. Validity and reliability of intraoperative monitoring in pediatric spinal deformity surgery: a 23-year experience of 3436 surgical cases. Spine (Phila Pa 1976). 2010;35(20):1880–6. https://doi.org/10.1097/BRS.0b013e3181e53434.
Warrender WJ, Oppenheimer S, Abboud JA. Nerve monitoring during proximal humeral fracture fixation: what have we learned? Clin Orthop Relat Res. 2011;469(9):2631–7. https://doi.org/10.1007/s11999-010-1760-3.
Wilson-Holden TJ, Padberg AM, Lenke LG, Larson BJ, Bridwell KH, Bassett GS. Efficacy of intraoperative monitoring for pediatric patients with spinal cord pathology undergoing spinal deformity surgery. Spine (Phila Pa 1976). 1999;24(16):1685–92.
Carofino BC, Brogan DM, Kircher MF, Elhassan BT, Spinner RJ, Bishop AT, Shin AY. Iatrogenic nerve injuries during shoulder surgery. J Bone Joint Surg Am. 2013;95(18):1667–74. https://doi.org/10.2106/JBJS.L.00238.
Bhalodia VM, Schwartz DM, Sestokas AK, Bloomgarden G, Arkins T, Tomak P, Gorelick J, Wijesekera S, Beiner J, Goodrich I. Efficacy of intraoperative monitoring of transcranial electrical stimulation-induced motor evoked potentials and spontaneous electromyography activity to identify acute-versus delayed-onset C-5 nerve root palsy during cervical spine surgery: clinical article. J Neurosurg Spine. 2013;19(4):395–402. https://doi.org/10.3171/2013.6.SPINE12355.
Tamkus A, Rice KS, Hoffman G. Transcranial motor evoked potential alarm criteria to predict foot drop injury during lumbosacral surgery. Spine (Phila Pa 1976). 2017. https://doi.org/10.1097/BRS.0000000000002288.
Yue Q, Hale T, Knecht A, Laidacker J. (2017) Intraoperative loss of tibialis anterior transcranial electrical motor evoked potentials predicted postoperative footdrop. World Neurosurg. 97:755.e1–755.e3. https://doi.org/10.1016/j.wneu.2016.10.036.
Block J, Silverstein JW, Ball HT, Mermelstein LE, DeWal HS, Madhok R, Basra SK, Goldstein MJ. Motor evoked potentials for femoral nerve protection in transpsoas lateral access surgery of the spine. Neurodiagn J. 2015;55(1):36–45.
Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94(6):495–501. https://doi.org/10.2106/JBJS.J.01830.
Tamkus AA, Rice KS, Kim HL. Differential rates of false-positive findings in transcranial electric motor evoked potential monitoring when using inhalational anesthesia versus total intravenous anesthesia during spine surgeries. Spine J. 2014;14(8):1440–6. https://doi.org/10.1016/j.spinee.2013.08.037.
Cheung E, Willis M, Walker M, Clark R, Frankle MA. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2011;19(7):439–49.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
This study was conducted under IRB approval from Thomas Jefferson University. Study ID: #11D.442.
Rights and permissions
About this article
Cite this article
Aleem, A.W., Wilent, W.B., Narzikul, A.C. et al. Incidence of peripheral nerve injury during shoulder arthroplasty when motor evoked potentials are monitored. J Clin Monit Comput 32, 897–906 (2018). https://doi.org/10.1007/s10877-017-0080-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-017-0080-5