Abstract
Real-time measurement of propofol in the breath may be used for routine clinical monitoring. However, this requires unequivocal identification of the expiratory phase of the respiratory propofol signal as only expiratory propofol reflects propofol blood concentrations. Determination of CO2 breath concentrations is the current gold standard for the identification of expiratory gas but usually requires additional equipment. Human breath also contains isoprene, a volatile organic compound with low inspiratory breath concentration and an expiratory concentration plateau. We investigated whether breath isoprene could be used similarly to CO2 to identify the expiratory fraction of the propofol breath signal. We investigated real-time breath data obtained from 40 study subjects during routine anesthesia. Propofol, isoprene, and CO2 breath concentrations were determined by a combined ion molecule reaction/electron impact mass spectrometry system. The expiratory propofol signal was identified according to breath CO2 and isoprene concentrations and presented as median of intervals of 30 s duration. Bland–Altman analysis was applied to detect differences (bias) in the expiratory propofol signal extracted by the two identification methods. We investigated propofol signals in a total of 3,590 observation intervals of 30 s duration in the 40 study subjects. In 51.4 % of the intervals (1,844/3,590) both methods extracted the same results for expiratory propofol signal. Overall bias between the two data extraction methods was −0.12 ppb. The lower and the upper limits of the 95 % CI were −0.69 and 0.45 ppb. Determination of isoprene breath concentrations allows the identification of the expiratory propofol signal during real-time breath monitoring.



Similar content being viewed by others
References
Hornuss C, Praun S, Villinger J, Dornauer A, Moehnle P, Dolch M, Weninger E, Chouker A, Feil C, Briegel J, Thiel M, Schelling G. Real-time monitoring of propofol in expired air in humans undergoing total intravenous anesthesia. Anesthesiology. 2007;106(4):665–74.
Perl T, Carstens E, Hirn A, Quintel M, Vautz W, Nolte J, Junger M. Determination of serum propofol concentrations by breath analysis using ion mobility spectrometry. Br J Anaesth. 2009;103(6):822–7. doi:10.1093/bja/aep312.
Takita A, Masui K, Kazama T. On-line monitoring of end-tidal propofol concentration in anesthetized patients. Anesthesiology. 2007;106(4):659–64.
Grossherr M, Hengstenberg A, Meier T, Dibbelt L, Gerlach K, Gehring H. Discontinuous monitoring of propofol concentrations in expired alveolar gas and in arterial and venous plasma during artificial ventilation. Anesthesiology. 2006;104(4):786–90.
Miekisch W, Fuchs P, Kamysek S, Neumann C, Schubert JK. Assessment of propofol concentrations in human breath and blood by means of HS-SPME-GC-MS. Clin Chim Acta. 2008;395(1–2):32–7.
Hornuss C, Wiepcke D, Praun S, Dolch ME, Apfel CC, Schelling G. Time course of expiratory propofol after bolus injection as measured by ion molecule reaction mass spectrometry. Anal Bioanal Chem. 2012;403(2):555–61. doi:10.1007/s00216-012-5856-3.
Boshier PR, Cushnir JR, Mistry V, Knaggs A, Spanel P, Smith D, Hanna GB. On-line, real time monitoring of exhaled trace gases by SIFT-MS in the perioperative setting: a feasibility study. Analyst. 2011;136(16):3233–7. doi:10.1039/c1an15356k.
Hornuss C, Zagler A, Dolch ME, Wiepcke D, Praun S, Boulesteix AL, Weis F, Apfel CC, Schelling G. Breath isoprene concentrations in persons undergoing general anesthesia and in healthy volunteers. J Breath Res. 2012;6(4):046004. doi:10.1088/1752-7155/6/4/046004.
Spanel P, Smith D. Progress in SIFT-MS: breath analysis and other applications. Mass Spectrom Rev. 2011;30(2):236–67. doi:10.1002/mas.20303.
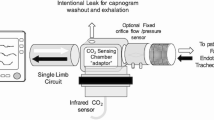
Dolch M, Frey L, Hornuss C, Schmoelz M, Praun S, Villinger J, Schelling G. Molecular breath-gas analysis by online mass spectrometry in mechanically ventilated patients: a new software-based method of CO2-controlled alveolar gas monitoring. J Breath Res. 2009;2:10.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346(8982):1085–7.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–60.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17(4):571–82. doi:10.1080/10543400701329422.
Miekisch W, Kischkel S, Sawacki A, Liebau T, Mieth M, Schubert JK. Impact of sampling procedures on the results of breath analysis. J Breath Res. 2008;2(2):026007. doi:10.1088/1752-7155/2/2/026007.
Anderson JC, Hlastala MP. Breath tests and airway gas exchange. Pulm Pharmacol Ther. 2007;20(2):112–7. doi:10.1016/j.pupt.2005.12.002.
Grossherr M, Hengstenberg A, Dibbelt L, Igl BW, Noel R, Knesebeck A, Schmucker P, Gehring H. Blood gas partition coefficient and pulmonary extraction ratio for propofol in goats and pigs. Xenobiotica. 2009;39(10):782–7. doi:10.1080/00498250903056109.
King J, Kupferthaler A, Unterkofler K, Koc H, Teschl S, Teschl G, Miekisch W, Schubert J, Hinterhuber H, Amann A. Isoprene and acetone concentration profiles during exercise on an ergometer. J Breath Res. 2009;3(2):027006. doi:10.1088/1752-7155/3/2/027006.
Schwoebel H, Schubert R, Sklorz M, Kischkel S, Zimmermann R, Schubert JK, Miekisch W. Phase-resolved real-time breath analysis during exercise by means of smart processing of PTR-MS data. Anal Bioanal Chem. 2011;401(7):2079–91. doi:10.1007/s00216-011-5173-2.
Kushch I, Arendacka B, Stolc S, Mochalski P, Filipiak W, Schwarz K, Schwentner L, Schmid A, Dzien A, Lechleitner M, Witkovsky V, Miekisch W, Schubert J, Unterkofler K, Amann A. Breath isoprene–aspects of normal physiology related to age, gender and cholesterol profile as determined in a proton transfer reaction mass spectrometry study. Clin Chem Lab Med. 2008;46(7):1011–8. doi:10.1515/CCLM.2008.181.
Smith D, Spanel P, Enderby B, Lenney W, Turner C, Davies SJ. Isoprene levels in the exhaled breath of 200 healthy pupils within the age range 7-18 years studied using SIFT-MS. J Breath Res. 2010;4(1):017101. doi:10.1088/1752-7155/4/1/017101.
Acknowledgments
This work was funded by departmental funds of the Department of Anaesthesiology at the Ludwig-Maximilians-University, Munich, Germany (Klinikum der Universität München). Additionally, V&F medical development supported the study by providing an ion molecule reaction mass spectrometry system during the study period. Siegfried Praun, Ph.D. is a scientist employed by V&F medical development. Cyrill Hornuss, M.D. received an unrestricted research grant from V&F. V&F reimbursed the travel expenses of Cyrill Hornuss and Michael Dolch, M.D. for meeting presentations related to this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hornuss, C., Dolch, M.E., Janitza, S. et al. Determination of breath isoprene allows the identification of the expiratory fraction of the propofol breath signal during real-time propofol breath monitoring. J Clin Monit Comput 27, 509–516 (2013). https://doi.org/10.1007/s10877-013-9452-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9452-7