Abstract
Autosomal recessive CARD9 deficiency underlies life-threatening, invasive fungal infections in otherwise healthy individuals normally resistant to other infectious agents. In less than 10 years, 58 patients from 39 kindreds have been reported in 14 countries from four continents. The patients are homozygous (n = 49; 31 kindreds) or compound heterozygous (n = 9; 8 kindreds) for 22 different CARD9 mutations. Six mutations are recurrent, probably due to founder effects. Paradoxically, none of the mutant alleles has been experimentally demonstrated to be loss-of-function. CARD9 is expressed principally in myeloid cells, downstream from C-type lectin receptors that can recognize fungal components. Patients with CARD9 deficiency present impaired cytokine and chemokine production by macrophages, dendritic cells, and peripheral blood mononuclear cells and defective killing of some fungi by neutrophils in vitro. Neutrophil recruitment to sites of infection is impaired in vivo. The proportion of Th17 cells is low in most, but not all, patients tested. Up to 52 patients suffering from invasive fungal diseases (IFD) have been reported, with ages at onset of 3.5 to 52 years. Twenty of these patients also displayed superficial fungal infections. Six patients had only mucocutaneous candidiasis or superficial dermatophytosis at their last follow-up visit, at the age of 19 to 50 years. Remarkably, for 50 of the 52 patients with IFD, a single fungus was involved; only two patients had IFDs due to two different fungi. IFD recurred in 44 of 45 patients who responded to treatment, and a different fungal infection occurred in the remaining patient. Ten patients died from IFD, between the ages of 12 and 39 years, whereas another patient died at the age of 91 years, from an unrelated cause. At the most recent scheduled follow-up visit, 81% of the patients were still alive and aged from 6.5 to 75 years. Strikingly, all the causal fungi belonged to the phylum Ascomycota: commensal Candida and saprophytic Trychophyton, Aspergillus, Phialophora, Exophiala, Corynesprora, Aureobasidium, and Ochroconis. Human CARD9 is essential for protective systemic immunity to a subset of fungi from this phylum but seems to be otherwise redundant. Previously healthy patients with unexplained invasive fungal infection, at any age, should be tested for inherited CARD9 deficiency.
Key Points
• Inherited CARD9 deficiency (OMIM #212050) is an AR PID due to mutations that may be present in a homozygous or compound heterozygous state.
• CARD9 is expressed principally in myeloid cells and transduces signals downstream from CLR activation by fungal ligands.
• Endogenous mutant CARD9 levels differ between alleles (from full-length normal protein to an absence of normal protein).
• The functional impacts of CARD9 mutations involve impaired cytokine production in response to fungal ligands, impaired neutrophil killing and/or recruitment to infection sites, and defects of Th17 immunity.
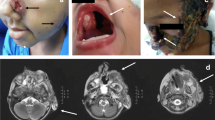
• The key clinical manifestations in patients are fungal infections, including CMC, invasive (in the CNS in particular) Candida infections, extensive/deep dermatophytosis, subcutaneous and invasive phaeohyphomycosis, and extrapulmonary aspergillosis.
• The clinical penetrance of CARD9 deficiency is complete, but penetrance is incomplete for each of the fungi concerned.
• Age at onset is highly heterogeneous, ranging from childhood to adulthood for the same fungal disease.
• All patients with unexplained IFD should be tested for CARD9 mutations. Familial screening and genetic counseling should be proposed.
• The treatment of patients with CARD9 mutations is empirical and based on antifungal therapies and the surgical removal of fungal masses. Patients with persistent/relapsing Candida infections of the CNS could be considered for adjuvant GM-CSF/G-CSF therapy. The potential value of HSCT for CARD9-deficient patients remains unclear.





Similar content being viewed by others
References
Glocker E-O, Hennigs A, Nabavi M, Schäffer A, Woellner C, Salzer U, et al. A homozygous CARD9 mutation in a family with susceptibility to fungal infections. N Engl J Med. 2009;361(18):1727–35.
Lanternier F, Pathan S, Vincent QBQB, Liu L, Cypowyj S, Prando C, et al. Deep dermatophytosis and inherited CARD9 deficiency. N Engl J Med. 2013;369:1704–14.
Lanternier F, Mahdaviani S, Barbati E, Chaussade H, Koumar Y, Levy R, et al. Inherited CARD9 deficiency in otherwise healthy children and adults with meningo-encephalitis and/or colitis caused by Candida. J Allergy Clin Immunol. 2015;135(6):1558–68.
Grumach AS, de Queiroz-Telles F, Migaud M, Lanternier F, Filho NR, Palma SMUU, et al. A homozygous CARD9 mutation in a Brazilian patient with deep dermatophytosis. J Clin Immunol. 2015;35:486–90.
Herbst M, Gazendam R, Reimnitz D, Sawalle-Belohradsky J, Groll A, Schlegel P-GG, et al. Chronic Candida albicans meningitis in a 4-year-old girl with a homozygous mutation in the CARD9 gene (Q295X). Pediatr Infect Dis J. 2015;34:999–1002.
Gavino C, Hamel N, Zeng B, Legault C, Guiot M, Chankowsky J, et al. Impaired RASGRF1/ERK-mediated GM-CSF response characterizes CARD9 deficiency in French-Canadians. J Allergy Clin Immunol. 2015;137(4):1178–88.
Drummond RA, Collar AL, Swamydas M, Rodriguez CA, Lim JK, Mendez LM, et al. CARD9-dependent neutrophil recruitment protects against fungal invasion of the central nervous system. PLoS Pathog. 2015;11:1–32.
Rieber N, Gazendam RP, Freeman AF, Hsu AP, Collar AL, Sugui JA, et al. Extrapulmonary Aspergillus infection in patients with CARD9 deficiency. JCI Insight. 2016;1:1–13.
Celmeli F, Oztoprak N, Turkkahraman D, Seyman D, Mutlu E, Frede N, et al. Successful granulocyte colony-stimulating factor treatment of relapsing Candida albicans meningoencephalitis caused by CARD9 deficiency. Pediatr Infect Dis J. 2016;35:428–31.
Alves de Medeiros AK, Lodewick E, Bogaert DJAA, Haerynck F, Van Daele S, Lambrecht B, et al. Chronic and invasive fungal infections in a family with CARD9 deficiency. J Clin Immunol. 2016;36:204–9.
Cetinkaya PG, Ayvaz DC, Karaatmaca B, Gocmen R, Söylemezoğlu F, Bainter W, et al. A young girl with severe cerebral fungal infection due to card 9 deficiency. Clin Immunol. 2018;191:21–6.
Puel A, Cypowyj S, Marodi L, Abel L, Picard C, Casanova J-L. Inborn errors of human IL-17 immunity underlie chronic mucocutaneous candidiasis. Curr Opin Allergy Clin Immunol. 2012;12(6):616–22.
Li J, Vinh DC, Casanova J-L, Puel A. Inborn errors of immunity underlying fungal diseases in otherwise healthy individuals. Curr Opin Microbiol. 2017;40:46–57.
Wang X, Zhang R, Wu W, Song Y, Wan Z, Han W, et al. Impaired specific antifungal immunity in CARD9-deficient patients with phaeohyphomycosis. J. Invest. Dermatol. 2018;138:607–17.
Wang X, Wang W, Lin Z, Wang X, Li T, Yu J, et al. CARD9 mutations linked to subcutaneous phaeohyphomycosis and TH17 cell deficiencies. J Allergy Clin Immunol. 2014;133:905–8.
Drewniak A, Gazendam RP, Tool ATJJ, van Houdt M, Jansen MH, Van Hamme JL, et al. Invasive fungal infection and impaired neutrophil killing in human CARD9 deficiency. Blood. 2013;121:2385–92.
Gavino C, Cotter A, Lichtenstein D, Lejtenyi D, Fortin C, Legault C, et al. CARD9 deficiency and spontaneous central nervous system candidiasis: complete clinical remission with GM-CSF therapy. Clin Infect Dis. 2014;59:81–4.
Jones N, Garcez T, Newman W, Denning D, Jones N, Garcez T, et al. Endogenous Candida endophthalmitis and osteomyelitis associated with CARD9 deficiency. BMJ Case Rep. 2016;2016:2015–7.
Gavino C, Mellinghoff S, Cornely OA, Landekic M, Le C, Langelier M, et al. Novel bi-allelic splice mutations in CARD9 causing adult-onset Candida endophthalmitis. Mycoses. 2017;12:3218–21.
Jachiet M, Lanternier F, Rybojad M, Bagot M, Ibrahim L, Casanova J-L, et al. Posaconazole treatment of extensive skin and nail dermatophytosis due to autosomal recessive deficiency of CARD9. JAMA Dermatology. 2015;151:192–4.
Boudghene Stambouli O, Amrani N, Boudghéne Stambouli K, Bouali F. Dermatophytic disease with deficit in CARD9: a new case with a brain impairment. J Mycol Med. 2017;27:250–3.
Lanternier F, Barbati E, Meinzer U, Liu L, Pedergnana V, Migaud M, et al. Inherited CARD9 deficiency in 2 unrelated patients with invasive exophiala infection. J Infect Dis. 2015;211:1241–50.
Yan XX, Yu CP, Fu XA, Bao FF, Du DH, Wang C, et al. CARD9 mutation linked to Corynespora cassiicola infection in a Chinese patient. Br J Dermatol. 2016;174:176–9.
Bertin J, Guo Y, Wang L, Srinivasula SM, Jacobson MD, Poyet JL, et al. CARD9 is a novel caspase recruitment domain-containing protein that interacts with BCL10/CLAP and activates NF-kB. J Biol Chem. 2000;275:41082–6.
Parkhouse R, Boyle JP, Mayle S, Sawmynaden K, Rittinger K, Monie TP. Interaction between NOD2 and CARD9 involves the NOD2 NACHT and the linker region between the NOD2 CARDs and NACHT domain. FEBS Lett. 2014;588:2830–6.
Hsu Y-MSMS, Zhang Y, You Y, Wang D, Li H, Duramad O, et al. The adaptor protein CARD9 is required for innate immune responses to intracellular pathogens. Nat Immunol. 2007;8:198–205.
Taylor PR, Tsoni SV, Willment JA, Dennehy KM, Rosas M, Findon H, et al. Dectin-1 is required for β-glucan recognition and control of fungal infection. Nat Immunol. 2007;8:31–8.
Robinson MJ, Osorio F, Rosas M, Freitas RP, Schweighoffer E, Groß O, et al. Dectin-2 is a Syk-coupled pattern recognition receptor crucial for Th17 responses to fungal infection. J Exp Med. 2009;206:2037–51.
Le Zhu L, Zhao XQ, Jiang C, You Y, Chen XP, Jiang YY, et al. C-type lectin receptors dectin-3 and dectin-2 form a heterodimeric pattern-recognition receptor for host defense against fungal infection. Immunity. 2013;39:324–34.
Yamasaki S, Ishikawa E, Sakuma M, Hara H, Ogata K, Saito T. Mincle is an ITAM-coupled activating receptor that senses damaged cells. Nat Immunol. 2008;9:1179–88.
Drummond RA, Lionakis MS. Mechanistic insights into the role of C-type lectin receptor/CARD9 signaling in human antifungal immunity. Front Cell Infect Microbiol. 2016;6(36):6–11.
Gross O, Gewies A, Finger K, Schäfer M, Sparwasser T, Peschel C, et al. Card9 controls a non-TLR signalling pathway for innate anti-fungal immunity. Nature. 2006;442:651–6.
Hara H, Ishihara C, Takeuchi A, Imanishi T, Xue L, Morris SW, et al. The adaptor protein CARD9 is essential for the activation of myeloid cells through ITAM-associated and Toll-like receptors. Nat Immunol. 2007;8:619–29.
Drummond RA, Saijo S, Iwakura Y, Brown GD. The role of Syk/CARD9 coupled C-type lectins in antifungal immunity. Eur J Immunol. 2011;41:276–81.
Roth S, Ruland J, Roth SRJ. Caspase recruitment domain-containing protein 9 signaling in innate immunity and inflammation. Trends Immunol. 2013;34:243–50.
Strasser D, Neumann K, Bergmann H, Marakalala MJ, Guler R, Rojowska A, et al. Syk kinase-coupled C-type lectin receptors engage protein kinase C-δ to elicit Card9 adaptor-mediated innate immunity. Immunity. 2012;36:32–42.
Kingeter LM, Lin X. C-type lectin receptor-induced NF-κB activation in innate immune and inflammatory responses. Cell Mol Immunol. 2012;9:105–12.
Ruland J. CARD9 signaling in the innate immune response. Ann N Y Acad Sci. 2008;1143:35–44.
LeibundGut-Landmann S, Groß O, Robinson MJ, Osorio F, Slack EC, Tsoni SVS, et al. Syk- and CARD9-dependent coupling of innate immunity to the induction of T helper cells that produce interleukin 17. Nat Immunol. 2007;8:630–8.
Roth S, Bergmann H, Jaeger M, Netea M. Vav proteins are key regulators of Card9 signaling for innate antifungal immunity. Cell Rep. 2016;17:2572–83.
Jia XM, Tang B, Zhu LL, Liu YH, Zhao XQ, Gorjestani S, et al. CARD9 mediates Dectin-1-induced ERK activation by linking Ras-GRF1 to H-Ras for antifungal immunity. J Exp Med. 2014;211:2307–21.
Willment JA, Marshall AS, Reid DM, Williams DL, Wong SYC, Gordon S, et al. The human β-glucan receptor is widely expressed and functionally equivalent to murine Dectin-1 on primary cells. Eur J Immunol. 2005;35:1539–47.
Sato K, Yang XL, Yudate T, Chung JS, Wu J, Luby-Phelps K, et al. Dectin-2 is a pattern recognition receptor for fungi that couples with the Fc receptor γ chain to induce innate immune responses. J Biol Chem. 2006;281:38854–66.
Wells CA, Salvage-Jones JA, Li X, Hitchens K, Butcher S, Murray RZ, et al. The macrophage-inducible C-type lectin, Mincle, is an essential component of the innate immune response to Candida albicans. J Immunol. 2008;180:7404–13.
Rogers NC, Slack EC, Edwards AD, Nolte MA, Schulz O, Schweighoffer E, et al. Syk-dependent cytokine induction by dectin-1 reveals a novel pattern recognition pathway for C type lectins. Immunity. 2005;22:507–17.
Yokota K, Takashima A, Bergstresser PR, Ariizumi K. Identification of a human homologue of the dendritic cell-associated C-typt lectin-1, dectin-1. Gene. 2001;272:51–60.
Kanazawa N, Tashiro K, Inaba K, Lutz MB, Miyachi Y. Molecular cloning of human Dectin-2. J Invest Dermatol. 2004;122:1522–4.
Balch SG, McKnight AJ, Seldin MF, Gordon S. Cloning of a novel C-type lectin expressed by murine macrophages. J Biol Chem. 1998;273:18656–64.
Matsumoto M, Tanaka T, Kaisho T, Sanjo H, Copeland NG, Gilbert DJ, et al. A novel LPS-inducible C-type lectin is a transcriptional target of NF-IL6 in macrophages. J Immunol. 1999;163:5039–48.
Di Carlo FJ, Fiore JV. On the composition of zymosan. Science. 1958;127:756–6.
McIntosh M, Stone BA, Stanisich VA. Curdlan and other bacterial (1→3)-β-D-glucans. Appl Microbiol Biotechnol. 2005;68:163–73.
Gringhuis SI, den Dunnen J, Litjens M, van der Vlist M, Wevers B, Bruijns SCM, et al. Dectin-1 directs T helper cell differentiation by controlling noncannonical NK-kB activation through Raf-1 and Syk. Nat Immunol. 2009;10:203–13.
Meyts I, Bosch B, Bolze A, Boisson B, Itan Y, Belkadi A, et al. Exome and genome sequencing for inborn errors of immunity. J Allergy Clin Immunol. 2016;138:957–69.
Itan Y, Shang L, Boisson B, Patin E, Bolze A, Moncada-Vélez M, et al. The human gene damage index as a gene-level approach to prioritizing exome variants. Proc Natl Acad Sci. 2015;112:13615–20.
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7:248–9.
Kircher M, Witten DM, Jain P, O’roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46:310–5.
Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc. 2009;4:1073–82.
Itan Y, Shang L, Boisson B, Ciancanelli MJ, Markle JG, Martinez-Barricarte R, et al. The mutation significance cutoff: gene-level thresholds for variant predictions. Nat Methods. 2016;13:109–10.
Gazendam RP, Van Hamme JL, Tool ATJ, Van Houdt M, Verkuijlen PJJH, Herbst M, et al. Two independent killing mechanisms of Candida albicans by human neutrophils: evidence from innate immunity defects. Blood. 2014;124:590–7.
Liang P, Wang X, Wang R, Wan Z, Han W, Li R. CARD9 deficiencies linked to impaired neutrophil functions against Phialophora verrucosa. Mycopathologia. 2015;179:347–57.
Drummond RA, Zahra FT, Natarajan M, Swamydas M, Hsu AP, Wheat LJ, et al. GM-CSF therapy in human CARD9 deficiency. J. Allergy Clin. Immunol. 2018.
Biggs CM, Keles S, Chatila TA. DOCK8 deficiency: insights into pathophysiology, clinical features and management. Clin Immunol. 2017;181:75–82.
Minegishi Y, Saito M, Tsuchiya S, Tsuge I, Takada H, Hara T, et al. Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature. 2007;448:1058–62.
Lionakis MS, Lim JK, Lee C-CR, Murphy PM. Organ-specific innate immune responses in a mouse model of invasive candidiasis. J Innate Immun. 2011;3:180–99.
Saresella M, Roda K, Speciale L, Taramelli D, Mendozzi E, Guerini F. A rapid evaluation of phagocytosis and killing of Candida albicans by CD13q leukocytes. J Immunol Methods. 1997;210:227–34.
Wu W, Zhang R, Wang X, Song Y, Liu Z, Han W, et al. Impairment of immune response against dematiaceous fungi in Card9 knockout mice. Mycopathologia. 2016;181:631–42.
Conti H, Gaffen S. IL-17-mediated immunity to the opportunistic fungal pathogen Candida albicans. J Immunol. 2015;195(3):780–8.
Cypowyj S, Picard C, Maródi L, Casanova JL, Puel A. Immunity to infection in IL-17-deficient mice and humans. Eur J Immunol. 2012;42:2246–54.
Glocker E, Grimbacher B. Chronic mucocutaneous candidiasis and congenital susceptibility to Candida. Curr Opin Allergy Clin Immunol. 2010;10:542–50.
Puel A, Cypowyj S, Bustamante J, Wright JF, Liu L, Lim K, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65–8.
Boisson B, Wang C, Pedergnana V, Wu L, Cypowyj S, Rybojad M, et al. An ACT1 mutation selectively abolishes interleukin-17 responses in humans with chronic mucocutaneous candidiasis. Immunity. 2013;39:676–86.
Ling Y, Cypowyj S, Aytekin C, Galicchio M, Camcioglu Y, Nepesov S, et al. Inherited IL-17RC deficiency in patients with chronic mucocutaneous candidiasis. J Exp Med. 2015;212:619–31.
Cua DJ, Tato CM. Innate IL-17-producing cells: the sentinels of the immune system. Nat. Rev. Immunol. 2010;10:479–98.
Svenson IK, Ashley-Koch AE, Gaskell PC, Riney TJ, Cumming WJ, Kingston HM, et al. Identification and expression analysis of spastin gene mutations in hereditary spastic paraplegia. Am J Hum Genet. 2001;68:1077–85.
Brown GD, Denning DW, Gow NAR, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4:1–9.
Queiroz-Telles F, Fahal AH, Falci DR, Caceres DH, Chiller T, Pasqualotto AC. Neglected endemic mycoses. Lancet Infect Dis. 2017;3099:1–11.
Lee PP, Lau YL. Cellular and molecular defects underlying invasive fungal infections—revelations from endemic mycoses. Front Immunol. 2017;8:735.
Sari S, Dalgic B, Muehlenbachs A, Deleon-Carnes M, Goldsmith CS, Ekinci O, et al. Prototheca zopfii colitis in inherited CARD9 deficiency. JID. 2018;XX.
Torres JM, Martinez-barricarte R, García-gómez S, Mazariegos MS, Itan Y, Boisson B, et al. Inherited BCL10 deficiency impairs hematopoietic and nonhematopoietic immunity. J Clin Invest. 2014;124:5239–48.
Jabara HH, Ohsumi T, Chou J, Massaad MJ, Benson H, Megarbane A, et al. A homozygous mucosa-associated lymphoid tissue 1 (MALT1) mutation in a family with combined immunodeficiency. J Allergy Clin Immunol. 2013;132:151–8.
McKinnon ML, Rozmus J, Fung SY, Hirschfeld AF, Del Bel KL, Thomas L, et al. Combined immunodeficiency associated with homozygous MALT1 mutations. J Allergy Clin Immunol. 2014;133:1458–1462.e7.
Köhler JR, Casadevall A, Perfect J. The spectrum of fungi that infects humans. Cold Spring Harb. Perspect. Med. 2015;5:a019273.
Bennett RJ, Turgeon BG. Fungal sex: the Ascomycota. Microbiol. Spectr. 2016;4:1–28.
Gow NAR, Latge J, Munro CA. The fungal cell wall: structure, biosynthesis, and function. Microbiol Spectr. 2017;5:1–25.
Hoving JC, Kolls JK. New advances in understanding the host immune response to pneumocystis. Curr Opin Microbiol. 2017;40:65–71.
Casanova JL, Abel L. Human genetics of infectious diseases: unique insights into immunological redundancy. Semin Immunol. 2018;36:1–12.
McManus BA, Coleman DC. Molecular epidemiology, phylogeny and evolution of Candida albicans. Infect Genet Evol. 2014;21:166–78.
Cauchie M, Desmet S, Lagrou K. Candida and its dual lifestyle as a commensal and a pathogen. Res Microbiol. 2016:1–9.
Lionakis MS, Netea MG. Candida and host determinants of susceptibility to invasive candidiasis. PLoS Pathog. 2013;9(1):1–5.
Papon N, Courdavault V, Clastre M, Bennett RJ. Emerging and emerged pathogenic Candida species: beyond the Candida albicans paradigm. PLoS Pathog. 2013;9(9):e1003550.
Zhan P, Liu W. The changing face of dermatophytic infections worldwide. Mycopathologia. 2017;182:77–86.
Havlickova B, Czaika VA, Fredrich M. Epidemiological trends in skin mycosis worldwide. Mycosis. 2008;51:2–15.
Rouzaud C, Hay R, Chosidow O, Dupin N, Puel A, Lortholary O, et al. Severe dermatophytosis and acquired or innate immunodeficiency: a review. J Fungi. 2015;2:4.
Chowdhary A, Perfect J, de Hoog GS. Black molds and melanized yeasts pathogenic to humans. Cold Spring Harb Perspect Med. 2015;5:a019570.
Chan GF, Puad MSA, Chin CF, Rashid NAA. Emergence of Aureobasidium pullulans as human fungal pathogen and molecular assay for future medical diagnosis. Folia Microbiol. 2011;56:459–67.
Dixon LJ, Schlub RL, Pernezny K, Datnoff LE. Host specialization and phylogenetic diversity of Corynespora cassiicola. Phytopathology. 2009;99:1015–27.
Samerpitak K, Duarte APM, Attili-Angelis D, Pagnocca FC, Heinrichs G, Rijs AJMM, et al. A new species of the oligotrophic genus Ochroconis (Sympoventuriaceae). Mycol Prog. 2015;14:1–10.
Brandt ME, Warnock DW. Epidemiology, clinical manifestations, and therapy of infections caused by dematiaceous fungi. J Chemother. 2003;15:36–47.
Seyedmousavi S, Netea MG, Mouton JW, Melchers WJG, Verweij PE, de Hoog GS. Black yeasts and their filamentous relatives: principles of pathogenesis and host defense. Clin Microbiol Rev. 2014;27:527–42.
Revanker S, Sutton D. Melanized fungi in human disease. Clin Microbiol Rev. 2010;23(4):884–928.
Paulussen C, Hallsworth JE, Álvarez-Pérez S, Nierman WC, Hamill PG, Blain D, et al. Ecology of aspergillosis: insights into the pathogenic potency of Aspergillus fumigatus and some other Aspergillus species. Microb Biotechnol. 2017;10:296–322.
Latgé J. Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev. 1999;12:310–50.
Dinauer MC. Primary immunedeficiencies with defects in neutrophil function. Hematology. 2016;2016:43–50.
Lee JH, Kim JS, Park YH. Diagnosis and treatment of postpartum Candida endophthalmitis. J Obstet Gynaecol Res. 2012;38:1220–2.
Oksi J, Finnilä T, Hohenthal U, Rantakokko-Jalava K. Candida dubliniensis spondylodiscitis in an immunocompetent patient. Case report and review of the literature. Med Mycol Case Rep. 2014;3:4–7.
Moon HH, Kim JH, Moon BG, Kim JS. Cervical spondylodiscitis caused by Candida albicans in non-immunocompromised patient. J Korean Neurosurg Soc. 2008;43:45–7.
Miller DJ, Mejicano GC. Vertebral osteomyelitis due to Candida species: case report and literature review. Clin Infect Dis. 2001;53706:523–30.
Antinori S, Milazzo L, Sollima S, Galli M, Corbellino M. Candidemia and invasive candidiasis in adults: a narrative review. Eur J Intern Med. 2016;34:21–8.
Seçkin D, Arikan S, Haberal M. Deep dermatophytosis caused by Trichophyton rubrum with concomitant disseminated nocardiosis in a renal transplant recipient. J Am Acad Dermatol. 2004;51:S173–6.
Dan P, Rawi R, Hanna S, Reuven B. Invasive cutaneous Trichophyton shoenleinii infection in an immunosuppressed patient. Int J Dermatol. 2011;50:1266–9.
Inaoki M, Nishijima C, Miyake M, Asaka T, Hasegawa Y, Anzawa K, et al. Case of dermatophyte abscess caused by Trichophyton rubrum: a case report and review of the literature. Mycoses. 2015;58:318–23.
Marconi VC, Kradin R, Marty FM, Hospenthal DR, Kotton CN. Disseminated dermatophytosis in a patient with hereditary hemochromatosis and hepatic cirrhosis: case report and review of the literature. Med Mycol. 2010;48:518–27.
Hadida E, Schousboe A. Dermatophytic disease aspects. Alger Med. 1959;63:303–36.
Gong JQ, Liu XQ, Xu HB, Zeng XS, Chen W, Li XF. Deep dermatophytosis caused by Trichophyton rubrum: report of two cases. Mycoses. 2007;50:102–8.
Kim S-H, Jo IH, Kang J, Joo SY, Choi J-H. Dermatophyte abscesses caused by Trichophyton rubrum in a patient without pre-existing superficial dermatophytosis: a case report. BMC Infect Dis. 2016;16:298–302.
Zeng JS, Sutton DA, Fothergill AW, Rinaldi MG, Harrak MJ, De Hoog GS. Spectrum of clinically relevant Exophiala species in the United States. J Clin Microbiol. 2007;45:3713–20.
Revankar SG, Sutton DA, Rinaldi MG. Primary central nervous system phaeohyphomycosis: a review of 101 cases. Clin Infect Dis. 2004;38:206–16.
Gao LJ, Yu J, Wang DL, Li RY. Recalcitrant primary subcutaneous Phaeohyphomycosis due to Phialophora verrucosa. Mycopathologia. 2013;175:165–70.
Panda A, Das H, Deb M, Khanal B, Kumar S. Aureobasidium pullulans keratitis. Clin Exp Ophthalmol. 2006;34:260–4.
Koppang HS, Olsen I, Stuge U, Sandven P. Aureobasidium infection of the jaw. J Oral Pathol Med. 1991;20:191–5.
Chen WT, Tu ME, Sun PL. Superficial Phaeohyphomycosis caused by Aureobasidium melanogenum mimicking tinea nigra in an immunocompetent patient and review of published reports. Mycopathologia. 2016;181:555–60.
Lv GX, Ge YP, Shen YN, Li M, Zhang X, Chen H, et al. Phaeohyphomycosis caused by a plant pathogen, Corynespora cassiicola. Med Mycol. 2011;49:657–61.
Mahgoub E. Corynespora cassiicola, a new agent of maduromycetoma. J Trop Med Hyg. 1969;72:218–21.
Yamada H, Takahashi N, Hori N, Asano Y, Mochizuki K, Ohkusu K, et al. Rare case of fungal keratitis caused by Corynespora cassiicola. J Infect Chemother. 2013;19:1167–9.
Huang HK, Liu CE, Liou JH, Hsiue HC, Hsiao CH, Hsueh PR. Subcutaneous infection caused by Corynespora cassiicola, a plant pathogen. J Inf Secur. 2010;60:188–90.
Segal B. Aspergillosis. N Engl J Med. 2009;360(18):1870–84.
Whibley N, Jaycox JR, Reid D, Garg AV, Taylor JA, Clancy CJ, et al. Delinking CARD9 and IL-17: CARD9 protects against Candida tropicalis infection through a TNF-a-dependent, IL-17-independent mechanism. J Immunol. 2015;195:3781–92.
Bishu S, Hernández-Santos N, Simpson-Abelson MR, Huppler AR, Conti HR, Ghilardi N, et al. The adaptor CARD9 is required for adaptive but not innate immunity to oral mucosal Candida albicans infections. Infect Immun. 2014;82:1173–80.
Jhingran A, Mar KB, Kumasaka DK, Knoblaugh SE, Ngo LY, Segal BH, et al. Tracing conidial fate and measuring host cell antifungal activity using a reporter of microbial viability in the lung. Cell Rep. 2012;2:1762–73.
Jhingran A, Kasahara S, Shepardson KM, Junecko BAFF, Heung LJ, Kumasaka DK, et al. Compartment-specific and sequential role of MyD88 and CARD9 in chemokine induction and innate defense during respiratory fungal infection. PLoS Pathog. 2015;11:1–22.
Hung CY, Castro-Lopez N, Cole GT. Card9- and MyD88-mediated gamma interferon and nitric oxide production is essential for resistance to subcutaneous Coccidioides posadasii infection. Infect Immun. 2016;84:1166–75.
Yamamoto H, Nakamura Y, Sato K, Takahashi Y, Nomura T, Miyasaka T, et al. Defect of CARD9 leads to impaired accumulation of gamma interferon-producing memory phenotype T cells in lungs and increased susceptibility to pulmonary infection with cryptococcus neoformans. Infect Immun. 2014;82:1606–15.
Casanova J-L, Abel L. The human model: a genetic dissection of immunity to infection in natural conditions. Nat Rev Immunol. 2004;4:55–66.
Quintana-Murci L, Alcaïs A, Abel L, Casanova JL. Immunology in natura: clinical, epidemiological and evolutionary genetics of infectious diseases. Nat Immunol. 2007;8:1165–71.
Dorhoi A, Desel C, Yeremeev V, Pradl L, Brinkmann V, Mollenkopf HJ, et al. The adaptor molecule CARD9 is essential for tuberculosis control. J Exp Med. 2010;207:777–92.
Wu W, Hsu Y-MSMS, Bi L, Songyang Z, Lin X. CARD9 facilitates microbe-elicited production of reactive oxygen species by regulating the LyGDI-Rac1 complex. Nat Immunol. 2009;10:1208–14.
Uematsu T, Iizasa E, Kobayashi N, Yoshida H, Hara H. Loss of CARD9-mediated innate activation attenuates severe influenza pneumonia without compromising host viral immunity. Sci Rep. 2015;5:1–11.
Bitar D, Lortholary O, Le Strat Y, Nicolau J, Coignard B, Tattevin P, et al. Population-based analysis of invasive fungal infections. Emerg Infect Dis. 2014;20:1149–55.
Limper AH, Adenis A, Le T, Harrison TS. Fungal infections 1 fungal infections in HIV/AIDS. Lancet Infect Dis. 2017;3099:1–10.
Kontoyiannis DP, Marr KA, Park BJ, Alexander BD, Anaissie EJ, Walsh TJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) database. Clin Infect Dis. 2010;50:1091–100.
Pappas PG, Alexander BD, Andes DR, Hadley S, Kauffman CA, Freifeld A, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis. 2010;50:1101–11.
Lanternier F, Cypowyj S, Picard C, Bustamante J, Lortholary O, Casanova J-L, et al. Primary immunodeficiencies underlying fungal infections. Curr Opin Pediatr. 2013;25:736–47.
Grimm MJ, Vethanayagam RR, Almyroudis NG, Lewandowski D, Rall N, Blackwell TS, et al. Role of NADPH oxidase in host defense against aspergillosis. Med Mycol. 2011;49:S144–9.
Donadieu J, Beaupain B, Fenneteau O, Bellanné-Chantelot C. Congenital neutropenia in the era of genomics: classification, diagnosis, and natural history. Br J Haematol. 2017:1–18.
Toubiana J, Okada S, Hiller J, Oleastro M, Gomez ML, Bousfiha A, et al. Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood. 2016;127:3154–65.
Leven EA, Maffucci P, Ochs HD, Scholl PR, Buckley RH, Fuleihan RL, et al. Hyper IgM syndrome: a report from the USIDNET registry. J Clin Immunol. 2016;36:490–501.
Zhang Q, Jing H, Su HC. Recent advances in DOCK8 immunodeficiency syndrome. J Clin Immunol. 2016;36:441–9.
Spinner MA, Sanchez LA, Hsu AP, Shaw PA, Zerbe CS, Calvo KR, et al. GATA2 deficiency: a protean disorder of hematopoiesis, lymphatics, and immunity. Blood. 2014;123:809–21.
Chandesris MO, Melki I, Natividad A, Puel A, Fieschi C, Yun L, et al. Autosomal dominant STAT3 deficiency and hyper-IgE syndrome: molecular, cellular, and clinical features from a french national survey. Medicine (Baltimore). 2012;91:1–19.
Bustamante J, Boisson-Dupuis S, Abel L, Casanova JL. Mendelian susceptibility to mycobacterial disease: genetic, immunological, and clinical features of inborn errors of IFN-g immunity. Semin Immunol. 2014;26:454–70.
Fischer A. Severe combined immunodeficiencies (SCID). Clin Exp Immunol. 2000;122:143–9.
Picard C, Casanova JL, Puel A. Infectious diseases in patients with IRAK-4, MyD88, NEMO, or IκBα deficiency. Clin Microbiol Rev. 2011;24:490–7.
Firinu D, Massidda O, Lorrai MM, Serusi L, Peralta M, Barca MP, et al. Successful treatment of chronic mucocutaneous candidiasis caused by azole-resistant Candida albicans with posaconazole. Clin Dev Immunol. 2011;2011:4.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Executive summary: clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:409–17.
Pires CAA, da Cruz NFS, Lobato AM, de Sousa PO, Carneiro FRO, Mendes AMD. Clinical, epidemiological, and therapeutic profile of dermatophytosis. An Bras Dermatol. 2014;89:259–64.
Gupta A, Cooper E. Update in antifungal therapy of dermatophytosis. Mycopathologia. 2008;166:353–67.
Oberlin KE, Nichols AJ, Rosa R, Dejman A, Mattiazzi A, Guerra G, et al. Phaeohyphomycosis due to Exophiala infections in solid organ transplant recipients: case report and literature review. Transpl Infect Dis. 2017:e12723.
Chowdhary A, Meis JF, Guarro J, de Hoog GS, Kathuria S, Arendrup MC, et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of systemic phaeohyphomycosis: diseases caused by black fungi. Clin Microbiol Infect. 2014;20:47–75.
Patterson TF, Thompson GR, Denning DW, Fishman JA, Hadley S, Herbrecht R, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;63:e1–60.
Filipovich AH. Hematopoietic cell transplantation for correction of primary immunodeficiencies. Bone Marrow Transplant. 2008;42:S49–52.
Seger RA. Modern management of chronic granulomatous disease. Br J Haematol. 2008;140:255–66.
Soncini E, Slatter MA, Jones LBKR, Hughes S, Hodges S, Flood TJ, et al. Unrelated donor and HLA-identical sibling haematopoietic stem cell transplantation cure chronic granulomatous disease with good long-term outcome and growth. Br J Haematol. 2009;145:73–83.
Parta M, Kelly C, Kwatemaa N, Theobald N, Hilligoss D, Qin J, et al. Allogeneic reduced-intensity hematopoietic stem cell transplantation for chronic granulomatous disease: a single-center prospective trial. J Clin Immunol. 2017;37:548–58.
Decook LJ, Thoma M, Huneke T, Johnson ND, Wiegand RA, Patnaik MM, et al. Impact of lymphocyte and monocyte recovery on the outcomes of allogeneic hematopoietic SCT with fludarabine and melphalan conditioning. Bone Marrow Transplant. 2013;48:708–14.
Maeurer M, Magalhaes I, Andersson J, Ljungman P, Sandholm E, Ulhin M, et al. Allogeneic hematopoietic cell transplantation for GATA2 deficiency in a patient with disseminated human papillomavirus disease. Transplantation. 2014;98:e94–5.
Cuellar-Rodriguez J, Gea-Banacloche J, Freeman AF, Hsu AP, Zerbe CS, Calvo KR, et al. Successful allogeneic hematopoietic stem cell transplantation for GATA2 deficiency. Blood. 2017;118:3715–21.
Miceli MH, Churay T, Braun T, Kauffman CA, Couriel DR. Risk factors and outcomes of invasive fungal infections in allogeneic hematopoietic cell transplant recipients. Mycopathologia. 2017;182:495–504.
Casanova J. Human genetic basis of interindividual variability in the course of infection. PNAS. 2015;112:E7118–27.
Casanova J. Severe infectious diseases of childhood as monogenic inborn errors of immunity. PNAS. 2015;1:E7128–37.
Acknowledgments
We thank all members of the Laboratory of Human Genetics of Infectious Diseases from the Necker and Rockefeller branches and, in particular, Yelena Nemirovskaya and Cécile Patissier for administrative work, Peng Zhang and Yuval Itan for helpful discussions, and Mélanie Migaud for technical work. We also warmly thank Dr. Fanny Lanternier and Prof. Olivier Lotholary, and Prof. Davood Mansouri (Masih Daneshvari Hospital, Tehran, Iran) for his collaboration and follow-up of patients.
Funding
This work was supported by Institut National de la Santé et de la Recherche Médicale (INSERM), Paris Descartes University, Assistance publique - Hôpitaux de Paris (AP-HP), the Rockefeller University, the St. Giles Foundation, and grants from Agence Nationale pour la Recherche (ANR) (grant HGDIFD no. ANR-14-CE15-0006-01, grant EURO-CMC no. ANR-14-RARE-0005-02) and from the National Institutes of Health (NIH) (R01-AI-127564). This study also received funding from the ANR as part of the “Investments for the Future” program (grant number ANR-10-IAHU-01) and Laboratoire d’Excellence “Integrative Biology of Emerging Infectious Diseases” (grant no. ANR-10-LABX-62-IBEID). AP was supported an AP-HP interface contract. EC was supported by the Belgian Fond National de la Recherche Scientifique (F.N.R.S).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Corvilain, E., Casanova, JL. & Puel, A. Inherited CARD9 Deficiency: Invasive Disease Caused by Ascomycete Fungi in Previously Healthy Children and Adults. J Clin Immunol 38, 656–693 (2018). https://doi.org/10.1007/s10875-018-0539-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-018-0539-2