Abstract
Beyond promoting hard tissue repairing, bioactive glasses (BGs) have also been proved to be beneficial for wound healing. Nano-scale BGs prepared by sol-gel method were found to have a better performance as they have a larger specific surface area. In this work, bioactive nanoparticles (nBPs) with mean diameter of 12 nm (BP-12) instead of conventional BGs were mixed with gelatin to form an easy-to-use hydrogel as a dressing for skin wound. It was found that the composite of BP-12 and gelatin could form a hydrogel (BP-12/Gel) under 25 °C, which showed pronounced thixotropy at a practically accessible shear rate, therefore become easy to be used for wound cover. In vitro, the composite hydrogel of BP-12 and gelatin had good biocompatibility with the fibroblast cells. In vivo, rapid cutaneous-tissue regeneration and tissue-structure formation within 7 days was observed in the wound-healing experiment performed in rats. This hydrogel is thus a promising easy-to-use wound dressing material.
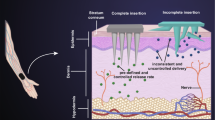
Graphical Abstract











Similar content being viewed by others
References
Balasubramani M, Kumar TR, Babu M. Skin substitutes: a review. Burns. 2001;27:534–44.
Ojeh N, Pastar I, Tomic-Canic M, Stojadinovic O. Stem cells in skin regeneration, wound healing, and their clinical applications. Int J Mol Sci. 2015;16:25476–501.
Reimers K, Liebsch C, Radtke C, Kuhbier JW, Vogt PM. Silks as scaffolds for skin reconstruction. Biotechnol Bioeng. 2015;112:2201–5.
Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, Gottrup F, Gurtner GC, Longaker MT. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009;17:763–71.
Peck MD. Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns. 2011;37:1087–100.
Miguez-Pacheco V, Hench LL, Boccaccini AR. Bioactive glasses beyond bone and teeth: emerging applications in contact with soft tissues. Acta Biomater. 2015;13:1–15.
Pereira RF, Barrias CC, Granja PL, Bartolo PJ. Advanced biofabrication strategies for skin regeneration and repair. Nanomedicine. 2013;8:603–21.
Sun BK, Siprashvili Z, Khavari PA. Advances in skin grafting and treatment of cutaneous wounds. Science. 2014;346:941–5.
Hench LL. Bioceramics. J Am Ceram Soc. 1998;81:1705–28.
Livingston T, Ducheyne P, Garino J. In vivo evaluation of a bioactive scaffold for bone tissue engineering. J Biomed Mater Res. 2002;62:1–13.
Rahaman MN, Day DE, Bal BS, Fu Q, Jung SB, Bonewald LF, Tomsia AP. Bioactive glass in tissue engineering. Acta Biomater. 2011;7:2355–73.
Ostomel TA, Shi Q, Tsung CK, Liang H, Stucky GD. Spherical bioactive glass with enhanced rates of hydroxyapatite deposition and hemostatic activity. Small. 2006;2:1261–5.
Ostomel TA, Shi Q, Stucky GD. Oxide hemostatic activity. J Am Chem Soc. 2006;128:8384–5.
Roether JA, Boccaccini AR, Hench LL, Maquet V, Gautier S, Jerome R. Development and in-vitro characterisation of novel bioresorbable and bioactive composite materials based on polylactide foams and Bioglass (R) for tissue engineering applications. Biomaterials. 2002;23:3871–8.
Day RM, Boccaccini AR, Shurey S, Roether JA, Forbes A, Hench LL, Gabe SM. Assessment of poly(glycolic acid) mesh and bioactive glass for soft tissue engineering scaffolds. Biomaterials. 2004;25:5857–66.
Gorustovich AA, Perio C, Roether JA, Boccaccini AR. Effect of bioactive glasses on angiogenesis: a review of in vitro and in vivo evidence. Tissue Eng B. 2010;16:199–207.
Balakrishnan B, Mohanty M, Fernandez AC, Mohanan PV, Jayakrishnan A. Evaluation of the effect of incorporation of dibutyryl cyclic adenosine monophosphate in an in situ-forming hydrogel wound dressing based on oxidized alginate and gelatin. Biomaterials. 2006;2:1355–61.
Tran NQ, Joung YK, Lih E, Park KD. In Situ forming and rutin-releasing chitosan hydrogels as injectable dressings for dermal wound healing. Biomacromolecules. 2011;12:2872–80.
Le Meins JF, Moldenaers P, Mewis J. Suspensions in polymer melts. 1. Effect of particle size on the shear flow behavior. Ind Eng Chem Res. 2002;41:6297–304.
Montes S, White JL. Rheological models of rubber-carbon black compounds: low interaction viscoelastic models and high interaction thixotropic - plastic - viscoelastic models. J Non-Newton Fluid Mech. 1993;49:277–98.
Letwimolnun W, Vergnes B, Ausias G, Carreau PJ. Stress overshoots of organoclay nanocomposites in transient shear flow. J Non-Newton Fluid Mech. 2007;141:167–79.
Mewis J, Wagner NJ. Thixotropy. Adv Colloid Interface Sci. 2009;147–148:214–27.
Guigo N, Sbirrazzuoli N, Vyazovkin S. Gelation on heating of supercooled gelatin solutions. Macromol Rapid Commun. 2012;33:698–702.
Crescenzi V, Francescangeli A, Taglienti A. New gelatin-based hydrogels via enzymatic networking. Biomacromolecules. 2002;3:1384–91.
Wang Y, Guo M, Genga Z, Xua H, Wang X, Guo X. Simple approach to generate fluorescent quantum dots/gelatin composite with thermo-responsive and reversible sol-gel transition. Soft Mater. 2015;13:177–82.
Vlierberghe SV, Schacht E, Dubruel P. Reversible gelatin-based hydrogels: fine tuning of material properties. Eur Polym J. 2011;47:1039–47.
Lei B, Shin KH, Noh DY, Jo IH, Koh YH, Choi WY, Kim HE. Nanofibrous gelatin-silica hybrid scaffolds mimicking the native extracellular matrix (ECM) using thermally induced phase separation. J Mater Chem. 2012;22:14133–40.
Kim HW, Song JH, Kim HE. Nanofiber generation of gelatin-hydroxyapatite biomimetics for guided tissue regeneration. Adv Funct Mater. 2005;15:1988–94.
Jenkins HP, Clarke JS. Gelatin sponge, a new hemostatic substance-studies on absorbability. Arch Surg. 1945;51:253–61.
Hu G, Xiao L, Tong P, Bi D, Wang H, Ma H, Zhu G, Liu H. Antibacterial hemostatic dressings with nanoporous bioglass containing silver. Int J Nanomed. 2012;7:2613–20.
Lin C, Mao C, Zhang J, Li Y, Chen X. Healing effect of bioactive glass ointment on full-thickness skin wounds. Biomed Mater. 2012;7:045017.
Curtis AR, West NX, Su B. Synthesis of nanobioglass and formation of apatite rods to occlude exposed dentine tubules and eliminate hypersensitivity. Acta Biomater. 2010;6:3740–6.
Lin S, Ionescu C, Pike KJ, Smith ME, Jones JR. Nanostructure evolution and calcium distribution in sol-gel derived bioactive glass. J Mater Chem. 2009;19:1276–82.
Hong Z, Liu A, Chen L, Chen X, Jing X. Mono-dispersed bioactive glass nanospheres: preparation and effects on biomechanics of mammalian cells. J Non-Cryst Solids. 2009;355:368–72.
Wang C, Xie Y, Li A, Shen H, Wu D, Qiu D. Bioactive nanoparticle through post-modification of colloidal silica. ACS Appl Mater Interfaces. 2014;6:4935–9.
Wang C, Shen H, Tian Y, Xie Y, Li A, Ji L, Niu Z, Wu D, Qiu D. Bioactive nanoparticle-gelatin composite scaffold with mechanical performance comparable to cancellous bones. ACS Appl Mater Interfaces. 2014;6:13061–8.
Jiao G, He X, Li X, Qiu J, Xu H, Zhang N, Liu S. Limitations of MTT and CCK-8 assay for evaluation of graphene cytotoxicity. RSC Adv. 2015;5:53240–4.
Pereira R, Carvalho A, Vaz DC, Gil MH, Mendes A, Bártolo P. Development of novel alginate based hydrogel films for wound healing applications. Int J Biol Macromol. 2013;52:221–30.
Dias AM, Braga MEM, Seabra IJ, Ferreira P, Gil MH, de Sousa HC. Development of natural-based wound dressings impregnated with bioactive compounds and using supercritical carbon dioxide. Int J Pharm. 2011;408:9–19.
Yannas IV, Burke JF. Design of an artificial skin. I. Basic design principles. J Biomed Mater Res. 1980;14:65–81.
Abdelrahman T, Newton H. Wound dressings: principles and practice. Surgery. 2011;29:491–5.
Burke JF, Yannas IV, Quinby WC Jr, Bondoc CC, Jung WK. Successful use of a physiologically acceptable artificial skin in the treatment of extensive burn injury. Ann Surg. 1981;194:413–28.
Kumbar SG, Nukavarapu SP, James R, Nair LS, Laurencin CT. Electrospun poly(lactic acid-co-glycolic acid) scaffolds for skin tissue engineering. Biomaterials. 2008;29:4100–7.
Eaglstein WH. Moist wound healing with occlusive dressings: a clinical focus. Dermatol Surg. 2011;27:175–81.
Greaves NS, Iqbal SA, Baguneid M, Bayat A. The role of skin substitutes in the management of chronic cutaneous wounds. Wound Rep Reg. 2013;21:194–210.
Geoffrey CG, Sabine W, Yann B, Michael TL. Wound repair and regeneration. Nature. 2008;453:314–21.
Jones JR. Review of bioactive glass: from Hench to hybrids. Acta Biomater. 2013;9:4457–86.
Acknowledgements
This work was supported by MOST (Project No. 2012CB933200, 2013DFG52300) and NSFC (Project No. 21474122, 51173193, 81202931).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Wang, C., Zhu, F., Cui, Y. et al. An easy-to-use wound dressing gelatin-bioactive nanoparticle gel and its preliminary in vivo study. J Mater Sci: Mater Med 28, 10 (2017). https://doi.org/10.1007/s10856-016-5823-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5823-1