Abstract
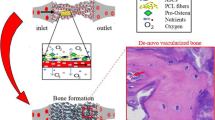
Vascularization is a key factor in the successful integration of tissue engineered (TE) grafts inside the host body. Biological functions of the newly formed tissue depend, in fact, on a reliable and fast spread of the vascular network inside the scaffold. In this study, we propose a technique for evaluating vascularization in TE constructs assembled by a bottom-up approach. The rational, ordered assembly of building blocks (BBs) into a 3D scaffold can improve vessel penetration, and—unlike most current technologies—is compatible with the insertion of different elements that can be designed independently (e.g. structural units, growth factor depots etc.). Poly(ε-caprolactone) scaffolds composed of orderly and randomly assembled sintered microspheres were used to assess the degree of vascularization in a pilot in vivo study. Scaffolds were implanted in a rat subcutaneous pocket model, and retrieved after 7 days. We introduce three quantitative factors as a measure of vascularization: the total percentage of vascularization, the vessels diameter distribution and the vascular penetration depth. These parameters were derived by image analysis of microcomputed tomographic scans of biological specimens perfused with a radiopaque polymer. The outcome of this study suggests that the rational assembly of BBs helps the onset and organization of a fully functional vascular network.








Similar content being viewed by others
References
Velazquez OC. Angiogenesis and vasculogenesis: inducing the growth of new blood vessels and wound healing by stimulation of bone marrow-derived progenitor cell mobilization and homing. J Vasc Surg. 2007;45 Suppl A:A39–47. doi:10.1016/j.jvs.2007.02.068.
Liekens S, De Clercq E, Neyts J. Angiogenesis: regulators and clinical applications. Biochem Pharmacol. 2001;61(3):253–70.
Adair TH, Montani JP. Angiogenesis. Integrated systems physiology: from molecule to function to disease. San Rafael; 2010.
Lamalice L, Le Boeuf F, Huot J. Endothelial cell migration during angiogenesis. Circ Res. 2007;100(6):782–94. doi:10.1161/01.RES.0000259593.07661.1e.
Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nat Med. 2000;6(4):389–95. doi:10.1038/74651.
Levenberg S, Rouwkema J, Macdonald M, Garfein ES, Kohane DS, Darland DC, et al. Engineering vascularized skeletal muscle tissue. Nat Biotechnol. 2005;23(7):879–84. doi:10.1038/nbt1109.
Ring A, Tilkorn D, Ottomann C, Geomelas M, Steinstraesser L, Langer S, et al. Intravital monitoring of microcirculatory and angiogenic response to lactocapromer terpolymer matrix in a wound model. Int Wound J. 2011;8(2):112–7. doi:10.1111/j.1742-481X.2010.00742.x.
Singh S, Wu BM, Dunn JC. Enhancing angiogenesis alleviates hypoxia and improves engraftment of enteric cells in polycaprolactone scaffolds. J Tissue Eng Regen Med. 2013;7(12):925–33. doi:10.1002/term.1484.
Biazar E, Heidari M, Asefnejad A, Montazeri N. The relationship between cellular adhesion and surface roughness in polystyrene modified by microwave plasma radiation. Int J Nanomed. 2011;6:631–9. doi:10.2147/IJN.S17218.
Kuddannaya S, Chuah YJ, Lee MH, Menon NV, Kang Y, Zhang Y. Surface chemical modification of poly(dimethylsiloxane) for the enhanced adhesion and proliferation of mesenchymal stem cells. ACS Appl Mater Interfaces. 2013;5(19):9777–84. doi:10.1021/am402903e.
Auger FA, Gibot L, Lacroix D. The pivotal role of vascularization in tissue engineering. Annu Rev Biomed Eng. 2013;15:177–200. doi:10.1146/annurev-bioeng-071812-152428.
Feng B, Jinkang Z, Zhen W, Jianxi L, Jiang C, Jian L, et al. The effect of pore size on tissue ingrowth and neovascularization in porous bioceramics of controlled architecture in vivo. Biomed Mater. 2011;6(1):015007. doi:10.1088/1748-6041/6/1/015007.
Woodruff MA, Lange C, Reichert J, Berner A, Chen FL, Fratzl P, et al. Bone tissue engineering: from bench to bedside. Mater Today. 2012;15(10):430–5.
Choi SW, Zhang Y, Macewan MR, Xia Y. Neovascularization in biodegradable inverse opal scaffolds with uniform and precisely controlled pore sizes. Adv Healthc Mater. 2013;2(1):145–54. doi:10.1002/adhm.201200106.
Bajaj P, Schweller RM, Khademhosseini A, West JL, Bashir R. 3D biofabrication strategies for tissue engineering and regenerative medicine. Annu Rev Biomed Eng. 2014;16:247–76. doi:10.1146/annurev-bioeng-071813-105155.
Elbert DL. Bottom-up tissue engineering. Curr Opin Biotechnol. 2011;22(5):674–80. doi:10.1016/j.copbio.2011.04.001.
Lantada AD, Morgado PL. Rapid prototyping for biomedical engineering: current capabilities and challenges. Annu Rev Biomed Eng. 2012;14:73–96. doi:10.1146/annurev-bioeng-071811-150112.
Lima MJ, Pirraco RP, Sousa RA, Neves NM, Marques AP, Bhattacharya M, et al. Bottom-up approach to construct microfabricated multi-layer scaffolds for bone tissue engineering. Biomed Microdevices. 2014;16(1):69–78. doi:10.1007/s10544-013-9806-4.
Mironov V, Trusk T, Kasyanov V, Little S, Swaja R, Markwald R. Biofabrication: a 21st century manufacturing paradigm. Biofabrication. 2009;1(2):022001. doi:10.1088/1758-5082/1/2/022001.
Nichol JW, Khademhosseini A. Modular tissue engineering: engineering biological tissues from the bottom up. Soft Matter. 2009;5(7):1312–9. doi:10.1039/b814285h.
Ferrara N. Molecular and biological properties of vascular endothelial growth factor. J Mol Med. 1999;77(7):527–43.
Muller YA, Heiring C, Misselwitz R, Welfle K, Welfle H. The cystine knot promotes folding and not thermodynamic stability in vascular endothelial growth factor. J Biol Chem. 2002;277(45):43410–6. doi:10.1074/jbc.M206438200.
Guldberg RE, Duvall CL, Peister A, Oest ME, Lin AS, Palmer AW, et al. 3D imaging of tissue integration with porous biomaterials. Biomaterials. 2008;29(28):3757–61. doi:10.1016/j.biomaterials.2008.06.018.
Schmidt C, Bezuidenhout D, Beck M, Van der Merwe E, Zilla P, Davies N. Rapid three-dimensional quantification of VEGF-induced scaffold neovascularisation by microcomputed tomography. Biomaterials. 2009;30(30):5959–68. doi:10.1016/j.biomaterials.2009.07.044.
Vasquez SX, Gao F, Su F, Grijalva V, Pope J, Martin B, et al. Optimization of microCT imaging and blood vessel diameter quantitation of preclinical specimen vasculature with radiopaque polymer injection medium. PLoS One. 2011;6(4):e19099. doi:10.1371/journal.pone.0019099.
Luciani A, Coccoli V, Orsi S, Ambrosio L, Netti PA. PCL microspheres based functional scaffolds by bottom-up approach with predefined microstructural properties and release profiles. Biomaterials. 2008;29(36):4800–7. doi:10.1016/j.biomaterials.2008.09.007.
Luciani A, Guarino V, Ambrosio L, Netti PA. Solvent and melting induced microspheres sintering techniques: a comparative study of morphology and mechanical properties. J Mater Sci Mater Med. 2011;22(9):2019–28. doi:10.1007/s10856-011-4390-8.
Bordes C, Freville V, Ruffin E, Marote P, Gauvrit JY, Briancon S, et al. Determination of poly(epsilon-caprolactone) solubility parameters: application to solvent substitution in a microencapsulation process. Int J Pharm. 2010;383(1–2):236–43. doi:10.1016/j.ijpharm.2009.09.023.
Oh SH, Lee JH. Hydrophilization of synthetic biodegradable polymer scaffolds for improved cell/tissue compatibility. Biomed Mater. 2013;8(1):014101.
Yeo A, Wong WJ, Khoo HH, Teoh SH. Surface modification of PCL-TCP scaffolds improve interfacial mechanical interlock and enhance early bone formation: an in vitro and in vivo characterization. J Biomed Mater Res A. 2010;92(1):311–21. doi:10.1002/jbm.a.32366.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60. doi:10.3758/Brm.41.4.1149.
Song C, Wang P, Makse HA. A phase diagram for jammed matter. Nature. 2008;453(7195):629–32. doi:10.1038/nature06981.
Eshraghi S, Das S. Mechanical and microstructural properties of polycaprolactone scaffolds with one-dimensional, two-dimensional, and three-dimensional orthogonally oriented porous architectures produced by selective laser sintering. Acta Biomater. 2010;6(7):2467–76. doi:10.1016/j.actbio.2010.02.002.
Jaklenec A, Hinckfuss A, Bilgen B, Ciombor DM, Aaron R, Mathiowitz E. Sequential release of bioactive IGF-I and TGF-beta 1 from PLGA microsphere-based scaffolds. Biomaterials. 2008;29:1518–25.
Borden M, Attawia M, Khan Y, Laurencin CT. Tissue engineered microsphere-based matrices for bone repair: design and evaluation. Biomaterials. 2002;23:551–9.
Jiang T, Nukavarapu SP, Deng M, Jabbarzadeh E, Kofron MD, Doty SB, Abdel-Fattah WI. Laurencin CT Chitosan-poly(lactide-co-glycolide) microsphere-based scaffolds for bone tissue engineering: in vitro degradation and in vivo bone regeneration studies. Acta Biomat. 2010;6:3457–70.
Bhamidipati M, Sridharan B, Scurto AM, Detamore MS. Subcritical CO2 sintering of microspheres of different polymeric materials to fabricate scaffolds for tissue engineering. Mater Sci Eng C Mater Biol Appl. 2013;33(8):4892–9.
Tarafder S, Balla VK, Davies NM, Bandyopadhyay A, Bose S. Microwave Sintered 3D Printed Tricalcium Phosphate Scaffolds for Bone Tissue Engineering. J Tissue Eng Regen Med. 2013;7(8):631–64.
Tiainen A, Lyngstadaas SP, Ellingsen JE, Haugen HJ. Ultra-porous titanium oxide scaffold with high compressive strength. J Mater Sci Mater Med. 2010;21(10):2783–92.
Wong HM, Chu PK, Leung FKL, Cheung KMC. Keith Luk DK, Yeung KWK. Engineered polycaprolactone–magnesium hybrid biodegradable porous scaffold for bone tissue engineering. Prog Nat Sci. 2014;24(5):561–7.
Chang KY, Hung LH, Chu IM, Ko CS, Lee YD. The application of type II collagen and chondroitin sulfate grafted PCL porous scaffold in cartilage tissue engineering. J Biomed Mater Res A. 2010;92(2):712–23.
Ekaputra AK, Prestwich GD, Cool SM, Hutmacher DW. Combining electrospun scaffolds with electrosprayed hydrogels leads to three-dimensional cellularization of hybrid constructs. Biomacromolecules. 2008;9(8):2097–103.
Ekaputra AK, Prestwich GD, Cool SM, Hutmacher DW. The three-dimensional vascularization of growth factor-releasing hybrid scaffold of poly (epsilon-caprolactone)/collagen fibers and hyaluronic acid hydrogel. Biomaterials. 2011;32(32):8108–17.
Acknowledgments
The authors would like to thank the staff of the Center of Biotechnologies of the A.O.R.N. “A. Cardarelli” for the kind support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
All animal experiments were performed in accordance with the Directive 2010/63/EU.
Additional information
L. Rossi and C. Attanasio have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Rossi, L., Attanasio, C., Vilardi, E. et al. Vasculogenic potential evaluation of bottom-up, PCL scaffolds guiding early angiogenesis in tissue regeneration. J Mater Sci: Mater Med 27, 107 (2016). https://doi.org/10.1007/s10856-016-5720-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5720-7