Abstract
Background
We quantified and characterized the outcomes of ablation in persistent atrial fibrillation (PersAF) subjects, and the utility of electroanatomical mapping with a market-released high-density (HD) mapping catheter.
Methods
PersAF subjects received electroanatomical mapping with the Advisor™ HD Grid mapping catheter, Sensor Enabled™ (HD Grid) and radiofrequency (RF) ablation to gather data regarding ablation strategies, mapping efficiency, quality, and outcomes. Subjects were enrolled from January 2019 to April 2020 across 25 international sites and followed for 12 months after the procedure.
Results
Three hundred thirty-four PersAF subjects (average age 64.2 years; 76% male; 25.4% previous AF ablation) were enrolled. Multiple map types were generated in a variety of rhythms using HD Grid. Significant differences in low voltage areas were identified in maps generated with the HD Wave Solution™ electrode configuration when compared to the standard configuration, which in some cases, influenced physicians’ ablation strategies. PV-only ablation strategy was used in 59.0% of subjects and 34.1% of subjects received PV ablation and additional lesions. Of the subjects, 82.0% were free from recurrent atrial arrhythmias at 12 months and new or increased dose of class I/III antiarrhythmic drugs. About 6.0% of subjects experienced a serious adverse event or serious adverse device effect through 12 months including 1 event deemed related to HD Grid and the index procedure by the investigator and 1 death unrelated to study devices.
Conclusions
The results of this study (NCT03733392) support the safety and utility of electroanatomical mapping with HD Grid in subjects with complex arrhythmias, such as PersAF in the real-world setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Atrial fibrillation (AF) is the most common arrhythmia and is associated with adverse prognosis including increased mortality [1]. Early rhythm control therapy including antiarrhythmic therapy and catheter ablation compared to standard care showed a reduced risk of a composite endpoint of death from cardiovascular causes, stroke, or hospitalization with worsening of heart failure or acute coronary syndrome in patients with early AF [2]. Catheter ablation reduces morbidity and mortality compared to antiarrhythmic drugs alone [3,4,5]. Pulmonary vein isolation (PVI) is the cornerstone in patients with paroxysmal AF (PAF) to electrically disconnect pulmonary veins from the left atrium and return patients to sinus rhythm (SR) [6, 7]. In persistent AF (PersAF), catheter ablation success rates are lower and standardized ablation technique is less evident.
While PVI is the cornerstone of catheter ablation for PAF, in PersAF, PVI alone has resulted in higher recurrence rates than those with PAF, indicating the potential for additional ablation targets beyond PVI [8, 9]. However, studies such as the STAR AF II clinical trial have found no significant reduction in the rate of recurrent AF when additional ablations were performed in addition to PVI and indicate that perhaps more selective targets may be needed to better characterize an individual patient’s specific arrhythmic substrate or ablation strategy [7]. Despite the fact that there is currently no consensus on the most successful ablation strategy for patients with PersAF, there is undoubtedly a broad agreement that detailed electroanatomical mapping of atrial substrates holds significant information to plan ablation strategy beyond PVI in PersAF. High-density (HD) mapping has been used to distinguish potential triggers and drivers of PersAF including areas of low voltage, fibrosis, local reentry, dyssynchrony and rotational drivers [10, 11]. Additionally, following AF ablation, complex arrhythmias are not uncommon. The majority of which occur in PersAF subjects and can be related to multiple different mechanisms [12]. This highlights the potential benefit of HD mapping in the identification of substrate, mechanisms, and ablation strategy of PersAF and accompanying atrial flutter (AFL) during redo ablation procedures.
Yeo et al. first identified the concept of “bipolar blindness” as the inability to detect an electrogram (EGM) when propagation of the wavefront is traveling perpendicular to the electrode dipole [12]. To overcome this obstacle, the Advisor™ HD Grid mapping catheter, Sensor Enabled™ (HD Grid) consists of four splines with four 1 mm equidistant electrodes mounted on each spline and attached at the tip to maintain a fixed distance between splines, which allows the HD Wave Solution™ (HDWS) electrode configuration to simultaneous analyze adjacent orthogonal bipolar signals. Therefore, the HDWS configuration preferentially selects EGMs with the greatest amplitude detected by the HD Grid mapping catheter, thus identifying local EGMs and correcting for the directional influence of wavefront propagation on bipolar signal amplitude, which may assist in substrate characterization and ablation strategy decisions.
The aim of this study is to quantify and characterize the outcomes of radiofrequency (RF) ablation in subjects with PersAF in real-world settings, and the utility of electroanatomical mapping with the HD Grid and EnSite Precision™ Cardiac Mapping System (SV 2.2 or higher, hereafter called “EnSite Precision”) with orthogonal bipole (HDWS) configuration.
2 Methods
2.1 Study design
The Advisor™ HD Grid Observational Study (NCT03733392) was a prospective, non-randomized, multicenter observational study designed to quantify and characterize the utility of electroanatomical mapping, and subsequent procedural outcomes of RF ablation after mapping with the Advisor™ HD Grid Mapping Catheter, Sensor Enabled (Abbott, St. Paul, MN) and the EnSite Precision™ Cardiac Mapping System with the HDWS configuration in subjects with PersAF in the real-world environment. Twenty-five international sites within Europe, Canada, Australia, and South Africa participated in this study. The conduct of the clinical study was in accordance with the Declaration of Helsinki and approved by the appropriate Ethics Committee of the respective clinical sites and as specified by local regulation. All patients enrolled in the study provided written informed consent.
2.2 Patient selection
This clinical study enrolled subjects over the age of 18 years who were indicated for cardiac RF ablation with electroanatomical mapping for the treatment of PersAF defined as documented continuous AF sustained beyond 7 days but less than 12 months. Patients with a PersAF diagnosis considered secondary to electrolyte imbalance, uncontrollable thyroid disease, or reversible or non-cardiac cause were excluded from the study. Other key exclusion criteria included left atrial diameter > 55 mm, left ventricular ejection fraction < 40%, uncontrolled heart failure or NYHA function class III or IV, or implanted ICD/CRT-D.
2.3 Mapping and procedure
Patient demographics, clinical history, and baseline clinical assessments were collected prior to the procedure. PersAF subjects underwent mapping and ablation according to the Instructions for Use (IFU) of the HD Grid, Ensite Precision™ Cardiac Mapping System, and any other medical devices used during the procedure. HD Grid was required to be used with EnSite Precision to generate a baseline electroanatomical map prior to ablation procedure. Complete contact with the cardiac wall was to be achieved before collecting data. Additional maps could be created or retrospectively generated using the Ensite™ TurboMap module (TurboMap). When reported, initial Automap/Turbomap settings used are detailed in Supplement Table S1. Ablation catheters were to be used per IFU to perform ablation per standard of care. Collection of additional maps and performance of additional ablations were allowed if clinically necessary. Ablation to treat other arrhythmias, such as AFL, that occurred during the procedure was allowed per physician discretion and standard of care. Data were collected during procedure regarding mapping activities and characteristics, procedural characteristics, ablation strategies and targets, and physician experience.
2.4 HDWS and standard configuration voltage comparisons
Any map generated with the HDWS electrode configuration could also be generated using the standard along-the-spline (hereafter called “standard “) electrode configuration with the same geometry as baseline map. If not performed during the procedure, this was performed after completion of the ablation procedure. A retrospective map was defined as the generation of a map that did not require collection of any new or additional electroanatomical data points. Instead, already collected mapping data was reused with new point collection or acquisition settings or electrode configurations selected (via TurboMap) or manual alteration of a copied open map. To compare overall mean voltage and low voltage surface area, only cases in which pre-ablation SR maps were generated with the HDWS configuration and the standard configuration were analyzed using the Ensite Precision platform.
2.5 Follow-up
A pre-discharge visit was performed post-procedure and included a 12-lead ECG, review of medication, and evaluation of any reportable adverse events. A serious adverse event (SAE) was any event that led to death, serious deterioration in health of the subject, or fetal distress, death, congenital abnormality or defect. A serious adverse device effect (SADE) is defined as any SAE that was determined to be a result of a medical device used in the study. A 90-day blanking period was utilized, and follow-up visits were scheduled at 6 months (180 ± 90 days) and 12 months (360 ± 90 days) from the index procedure. Information collected at scheduled follow-up visits included assessment of atrial arrhythmia recurrence (AF, AFL, or atrial tachycardia “AT “ lasting 30 s or longer), antiarrhythmic medication use (including class I/III AAD and dose), completed EQ-5D-5L and AFEQT (Atrial Fibrillation Effect on Quality-of-life) quality of life (QOL) surveys, occurrence of adverse events or protocol deviations. Holter monitors were issued at the 12-month visit and subjects were instructed to obtain a 48-h recording from which a core laboratory reviewed and reported findings to Abbott. Results from the Holter monitors were used for determining the rate of long-term success in PersAF subjects. The proportion of subjects free from repeat ablation procedures to treat PersAF outside the blanking period out of all subjects from which data were available were also documented.
2.6 Statistical methods
The objectives of this study were addressed through multiple descriptive endpoints. Categorical variables were reported as proportion and number of subjects. Continuous variables were reported as mean ± standard deviation and number of subjects and, where specified, median (Q1, Q3) (min, max). Comparisons of overall mean voltage and low-voltage surface area were performed using the paired t-test as each initial map served as a patient’s own control. Comparisons of quality-of-life scores at 6 and 12 months relative to baseline were performed using paired t-test. All p values are reported descriptively. Results with p < 0.05 were considered statistically significant. All statistical analyses were performed using SAS 9.4.
3 Results
3.1 Study population
Between January 2019 and April 2020, a total of 334 subjects with PersAF across 25 international sites were enrolled and received an ablation procedure in this study (Supplement Table S2). Seventy-six percent of the population were male with an average age of 64.2 ± 10.4 years, and all underwent electroanatomical mapping with the HD Grid mapping catheter and received RF energy delivery. Baseline characteristics are summarized in Table 1. History of arrhythmia and previous ablation treatment in PersAF subjects is summarized in Table 2. All subjects had a prior history of AF and 25.4% (85/334) were previously ablated to treat AF. Prior AF ablation strategy included PVI only (36.5%) and ablation beyond PVI (40.0%). Subjects also had a history of AFL and AT, some of which had a history of ablation targeting these arrhythmias prior to their enrollment in this study (Table 2).
3.2 HD Grid mapping characteristics and ablation strategies
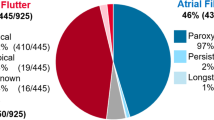
After providing consent for study participation, electroanatomical mapping during the ablation procedure was performed with the HD Grid mapping catheter. A total of 496 maps were generated in a variety of cardiac structures (Fig. 1) and rhythms (Table 3) intended for the treatment of PersAF and other arrhythmias (i.e., AFL). These high-density maps were efficiently created with an average of 9799.0 ± 8665.9 and 2064.7 ± 1431.1 total collected and used mapping points, respectively, in an average of 12.5 ± 9.1 min per map (Table 3). Physicians in this study primarily referenced peak-to-peak maps (69.2%; 343/493) to treat PersAF subjects (Table 3). The configuration that compares simultaneous orthogonal bipoles, HDWS configuration, was the primary configuration used to map and identify ablation strategies in the majority of subjects (76.3%; 255/334). Substrates frequently searched for and identified included areas of low voltage, scar/fibrosis, and CFE (Supplement Table S3). PV-only targets were ablated in 59.0% (197/334) of all procedures. 34.1% (114/334) of subjects received PV plus additional lesions and 6.9% (23/334) of subjects’ ablation strategy did not include any PV targets. Non-PV ablation targets included the roof of the left atrium, posterior wall isolation, cavotricuspid isthmus, and mitral isthmus, among others. Ablation targets utilized in this study to treat PersAF subjects are summarized in Fig. 1.
Regions mapped and ablated. The percentage of patients in which a particular region of the left atrium (anterior–posterior view, top left; posterior-anterior view, bottom left) or right atrium (anterior–posterior view, top right; posterior-anterior view, bottom right) was mapped with HD Grid (blue text) or ablated with RF study catheter (green text). LAA = left atrial appendage, RAA = right atrial appendage, LOM = ligament of Marshall, LSPV = left superior pulmonary vein, LIPV = left inferior pulmonary vein, RSPV = right superior pulmonary vein, RIPV = right inferior pulmonary vein, SVC = superior vena cava, IVC = inferior vena cava
3.3 Identification of substrates with simultaneous orthogonal configuration has an impact on ablation strategy
In order to better understand the role of simultaneous orthogonal bipole configurations with HD Grid in identifying ablation targets beyond traditional mapping methods, maps generated using HDWS configuration were compared to those created with the standard configuration (Supplement Fig. S1). The number of maps reported here was dependent on the data availability of comparative maps, the timing of the map comparisons, and the differences identified in compared maps, therefore resulting in a number of different analysis groups. In cases where comparable maps were generated, physicians reported that mapping with the HDWS configuration showed differences in substrate characteristics in 56.3% (153/272) of maps, including 29 instances where the comparison was performed in real time during the procedure and 124 maps where the comparison was performed after the procedure using retrospective maps generated with the standard configuration. It is important to note that comparisons made in real-time during the procedure actively informed the physicians’ ablation strategy whereas comparisons made after the procedure only indicate potential changes to the ablation strategy. The differences in substrate characteristics identified with the HDWS configuration versus the standard configuration, such as location and/or surface area of low voltage, fractionation, and activation time/activation sequence, have the potential to influence ablation strategy. In comparisons during the procedure, physicians reported the HDWS configuration assisted in identifying the ablation strategy in 69.0% (20/29) of these cases and changed the ablation strategy in 41.4% (12/29). In retrospective comparisons, 32.3% (40/124) of maps generated with the HDWS configuration identified an ablation strategy different than what would have been identified with the standard maps (Fig. 2).
Substrate differences identified and role in ablation strategy of HDWS versus standard configurations. Flow diagram describing the number of maps generated with the HDWS configuration that were compared to maps generated with the standard configuration using the HD Grid mapping catheter, including comparisons made during (boxes outlined in pink) and after (boxes outlined in orange) the procedure in cases which HDWS configuration identified differences in overall substrate characteristics versus standard configuration (boxes outlined and shaded in blue) as well as a further breakdown of the same comparisons in cases which HDWS configuration maps identified differences specifically in surface area and/or location of low voltage substrate versus standard configuration (boxes outlined and shaded in green)
3.4 Mapping with HD Grid in the simultaneous orthogonal configuration provides voltage measurements significantly different than standard electrode configuration
Overall, the greatest differences identified in maps generated using the HDWS configuration versus standard were in surface area and/or location of low voltage (79.7%; 122/153). Of the 122 maps in which surface area and/or location of low voltage were reported to differ between HDWS and standard electrode configurations, 15 maps were compared in real-time during the procedure and 107 maps were compared retrospectively after the procedure. Of the real-time comparisons, the HDWS configuration was reported to have assisted in identifying the ablation strategy in 53.3% (8/15) of maps and changed the ablation strategy in 26.7% (4/15) of maps (Fig. 2). Of the retrospective comparisons, the ablation strategy identified by the HDWS configuration was different than what would have been identified with the standard configuration in 30.8% (33/107) of maps. One example of this retrospective comparison in which HDWS configuration identified differences in low voltage that informed the ablation strategy is shown in Fig. 3A. The HDWS configuration map in Fig. 3A clearly shows reduced low voltage areas compared to standard configuration. In this example, the information provided by the HDWS configuration led to less substrate modification especially at the bottom of the left atrium and at the left atrial isthmus.
Low voltage differences between HDWS and standard configurations. A A left atrial high-density voltage map from posterior anterior view (PA) during sinus rhythm (SR) in HD Wave Solution (HDWS; left) and in standard configuration (right). Depicting scar area < 0.2 mV in gray and healthy myocardium > 0.5 mV in purple in both maps. Red circles highlight observable differences in low voltage areas between the two configurations. Six thousand eighty-nine yellow dots depict recorded local atrial signal. LSPV left superior pulmonary vein, LIPV left inferior pulmonary vein, RSPV left posterior pulmonary vein, RIPV left posterior pulmonary vein. B Analysis of pre-ablation maps generated during SR depicting a significant difference in overall mean voltage detected by HDWS configuration versus standard configuration. Paired t-test was used for statistical analysis. C Analysis of pre-ablation maps generated during SR depicting a significant difference in low voltage area (0.2–0.5 mV) detected by HDWS configuration versus standard configuration. Paired t-test was used for statistical analysis
To objectively quantify the change in low voltage identified between electrode configurations, pre-ablation maps of the left atrium generated when subjects were in SR were analyzed (N = 26). As the comparable retrospective maps were generated with the same mapping points and electroanatomical data as the original, each map served as its own control. The mean voltage detected with the HDWS configuration was 1.62 ± 0.80 mV while there was a significant reduction of mean voltage with the standard configuration of 1.38 ± 0.68 mV (average difference in mean voltage of 0.24 (p < 0.0001)) (Fig. 3B). The total surface area of low voltage (LVA) detected in the entire left atrium with the HDWS configuration versus standard configuration was also compared using peak-to-peak bipolar voltage of 0.2–0.5 mV to define LVA. LVA was significantly different with 27.94 ± 12.45 cm2 detected by the HDWS configuration and 31.56 ± 13.34 detected by the standard configuration (p < 0.0001) (Fig. 3C). Therefore, mapping in standard configuration detected a significantly larger total surface area of low voltage in the left atrium.
3.5 The Advisor HD Grid Observational Study resulted in safe and effective short- and long-term outcomes for PersAF patients
The procedural characteristics of this study are summarized in Table 4. Acute success defined as the proportion of subjects who received HD Grid mapping and RF energy delivery resulting in termination of clinical arrhythmia or non-inducibility of clinical arrhythmia after ablation with cardioversion allowed prior to inducibility attempt was achieved in 85.9% (287/334) of subjects (Table 4). Utilizing a 90-day blanking period following the index ablation procedure, 82.0% (168/205) of subjects were free from all atrial arrhythmias (AF/AFL/AT) greater than 30 s as documented by 48-h Holter monitor at their 12-month follow-up visit and new or increased dose of class I/III AADs. Additionally, at 12-months follow-up, 97.0% (291/300) of subjects were free from an additional procedure to specifically treat PersAF after the 90-day blanking period. (Table 4).
Changes in QOL at 6 and 12 months after receiving HD Grid mapping and RF ablation relative to baseline were assessed in validated QOL surveys. Overall AFEQT scores significantly increased from an average of 59.8 ± 22.4 at baseline to 85.0 ± 15.6 at the 12-month visit (p < 0.0001) (Fig. 3). EQ-5D-5L visual analog scales (VAS) scores also significantly increased relative to baseline (p < 0.0001) (Fig. 4).
Of the PersAF subjects, 6.0% (20/334) experienced an SAE or SADE following the procedure throughout the entire duration of the study. Two SAEs and 12 SADEs occurred periprocedurally and 2 SAEs and 6 SADEs within 30 days postprocedure with 1 event overall deemed related to the HD Grid mapping catheter and index procedure. There was one death in the study from a massive intracranial hemorrhage 226 days postprocedure, the cause of which was unknown and deemed unrelated to the HD Grid mapping catheter or index procedure. Adverse event types are further detailed in Supplement Tables S4 and S5.
4 Discussion
4.1 Main findings of the study
This is the first real world prospective, non-randomized, multicenter observational study investigating the use of the Advisor™ HD Grid mapping catheter and the HDWS configuration in patients undergoing RF ablation for PersAF. HD Grid was efficient and useful for creating detailed electroanatomical maps. In these maps, the use of a the HDWS mapping configuration identified quantifiable differences that changed the ablation strategy of the operator. This study resulted in favorable procedural characteristics and outcomes and demonstrated the utility of mapping with HD Grid.
The age, sex, and concomitant disease in this study population were typical of the PersAF population and comparable to other PersAF trials [7, 13]. Approximately one third of patients had a history of heart failure (28.1%) predominantly with NYHA Class II and the majority of patients were symptomatic from AF. A quarter of patients received at least one previous ablation for AF. Of these patients, 36.5% were treated with PVI only in the previous ablation procedure.
Efficiency of the HD Grid catheter and the HDWS configuration was reflected in 496 maps using a mapping time of 12.5 ± 9.1 min, collecting a mean of 9799 ± 8665.9 points per patient in different rhythms. This is comparable in quantity and time to other mapping systems [14]. The underlying rhythm during mapping was mainly SR or another regular atrial rhythm to allow interpretation of atrial substrate. 31.7% of patients were mapped while in AF.
Comparing the HDWS configuration to the standard configuration revealed clear differences in substrate characteristics. The most prominent differences between the two electrode configurations were seen in location and/or surface area of low voltage (79.7%). Representation of fractionated electrograms or activation time and sequence was less eminent. In SR, total surface area of low voltage areas was significantly smaller (mean difference of 3.63 cm2) and true voltage at these locations was significantly higher (mean difference 0.24 mV) with the HDWS configuration. Furthermore, physicians reported their ablation strategy identified with the HDWS configuration was different than what would have been identified with the standard configuration in 30.8% (33/107) comparisons after the procedure. This particularly important finding demonstrates the potential of the HD Grid catheter to provide a more complete picture and accurate basis for additional ablation strategies beyond PVI.
Primary ablation strategy was PVI (59.0%) followed by 34.1% of patients who received PVI and additional lines. These numbers reflect adhesion to recent international guidelines [6]. Targets of additional ablation were represented by the roof area and posterior wall. Cavo tricuspid isthmus (CTI) and mitral isthmus ablation were performed in approximately 10% of cases each to treat right and left macro-reentry tachycardias.
In a meta-analysis including 956 patients with PersAF, single procedure arrhythmia-free survival for PVI alone showed 66.7% at 12-month follow-up [15]. These data position therapy towards palliation rather than a cure as a realistic future goal. Acute success in this cohort, defined as acute termination or non-inducibility of clinical arrhythmia, was 85.9%, taking into account that cardioversion was allowed prior to final induction. 82.0% of patients were free from atrial recurrence as documented by 48-h Holter monitoring at the 12-month follow-up visit and new or increased dose of class I/III AADs. This finding includes patients with PVI only and patients with PVI and additional lines mainly at the roof and posterior wall. This rather high percentage of patients free of recurrence compared to other studies should be cautiously interpreted [7, 16,17,18]. It is also important to recall this study enrolled patients with previous ablation procedures rather than only performing de novo ablation. This also applies to the high percentage of patients (97%) who did not receive repeat ablation procedures after the 90-day blanking period to specifically treat AF. Another very promising finding is that catheter ablation significantly improves quality of life measured by AFEQT and EQ-5D-5L VAS Score which goes along with other recent studies [19, 20]. These data emphasize the utility of the Advisor™ HD grid mapping catheter to identify ablation strategies resulting in effective ablation procedures and improved QOL.
A total of 6.0% of PersAF patients experienced a SAE or SADE. However, only one out of 54 total adverse events, a procedure related stroke, was linked to the use of the Advisor™ HD Grid catheter. One patient death occurred due to a severe intracranial hemorrhage 226 days after the index procedure and was considered not related to the procedure. These data underline the safety of the Advisor HD Grid catheter.
4.2 Study limitations
Due to the COVID-19 pandemic, early enrollment closures were implemented, thus impacting the study sample size. Additionally, the pandemic prevented many patients from completing required Holter monitoring at their 12-month follow-up visit. This significantly impeded data collection for long-term effectiveness as the analysis of arrhythmia recurrence only considered failures if it was documented by the 48-h Holter monitor. Other forms of arrhythmia documentation were collected at unscheduled visits or 6-month follow-up but were not included in this analysis. As this study was designed to collect data on how the HD Grid catheter was used in the real-world setting, there were no rigid mapping protocols but rather strong recommendations for generating maps with the HDWS configuration versus the standard configuration. Data on mapping comparisons, such as “change in ablation strategy,” were reported by physicians in categorical form. This limits the ability to report details of ablation targets or how ablation strategy differed between HDWS and standard configuration comparisons. Additionally, comparisons of the pre-ablation HDWS configuration maps to the standard electrode configuration maps were largely performed after the procedure was completed and the study was not designed to prospectively compare outcomes related to HDWS guided ablation strategies. Further research is needed to better understand how ablation strategy is impacted by the difference in electroanatomical maps identified in the current study, and how the impacted ablation strategy affects long-term outcomes.
5 Conclusion
The use of the Advisor™ HD Grid Mapping Catheter, Sensor Enabled™ catheter with the ability to analyze and compare orthogonal signals is feasible and has the potential to influence the ablation strategy in PersAF with high acute and long-term success rates. Overall, this study provides evidence supporting the use of the HD Grid catheter and the HDWS electrode configuration to create detailed, high-quality maps to perceptively search for and identify substrates such as low voltage to treat PersAF subjects. The results of this study support the safety and utility of electroanatomical mapping with HD Grid in subjects with complex arrythmias in the real-world setting.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death. Circulation. 1998;98(10):946–52. https://doi.org/10.1161/01.cir.98.10.946 ([published Online First: Epub Date]|).
Kirchhof P, Camm AJ, Goette A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 2020;383(14):1305–16. https://doi.org/10.1056/nejmoa2019422 ([published Online First: Epub Date]|).
Saglietto A, De Ponti R, Di Biase L, et al. Impact of atrial fibrillation catheter ablation on mortality, stroke, and heart failure hospitalizations: a meta-analysis. J Cardiovasc Electrophysiol. 2020;31(5):1040–7. https://doi.org/10.1111/jce.14429 ([published Online First: Epub Date]|).
Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Ep Europace. 2018;20(1):e1–160.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–76.
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS) The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498.
Verma A, Jiang C-Y, Betts TR, et al. Approaches to Catheter Ablation for Persistent Atrial Fibrillation. N Engl J Med. 2015;372(19):1812–22. https://doi.org/10.1056/nejmoa1408288 ([published Online First: Epub Date]|).
Ackerman MJ, Priori SG, Willems S, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies: This document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). EP Europace. 2011;13(8):1077–109. https://doi.org/10.1093/europace/eur245 ([published Online First: Epub Date]|).
Schade A, Costello-Boerrigter L, Steinborn F, et al. Voltage-guided ablation in persistent atrial fibrillation—favorable 1-year outcome and predictors. J Interv Card Electrophysiol. 2021;62(2):249–57.
Rolf S, Hindricks G, Sommer P, et al. Electroanatomical mapping of atrial fibrillation: Review of the current techniques and advances. Rolf S, Hindricks G, Sommer P, Richter S, Arya A, Bollmann A, Kosiuk J, Koutalas E.J. Atr Fibrillation. 2014;7(4):1140. https://doi.org/10.4022/jafib.1140
Saini A, Huizar JF, Tan A, Koneru JN, Ellenbogen KA, Kaszala K. Scar homogenization in atrial fibrillation ablation: evolution and practice. Journal of Atrial Fibrillation 2017;10(3), https://doi.org/10.4022/jafib.1645 [published Online First: Epub Date]|.
Castrejón-Castrejón S, Ortega M, Pérez-Silva A, et al. Organized atrial tachycardias after atrial fibrillation ablation. Cardiol Res Pract. 2011;2011:1–16. https://doi.org/10.4061/2011/957538 ([published Online First: Epub Date]|).
Packer DL, Mark DB, Robb RA, et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation. JAMA. 2019;321(13):1261. https://doi.org/10.1001/jama.2019.0693 ([published Online First: Epub Date]|).
Kosiuk J, Hilbert S, John S, Bertagnolli L, Hindricks G, Bollmann A. Preliminary experience with high-density electroanatomical mapping for ablation of atrial fibrillation–Comparison of mini-basket and novel open irrigated magnetic ablation catheter in consecutive patients. Int J Cardiol. 2017;228:401–5.
Voskoboinik A, Moskovitch JT, Harel N, Sanders P, Kistler PM, Kalman JM. Revisiting pulmonary vein isolation alone for persistent atrial fibrillation: a systematic review and meta-analysis. Heart Rhythm. 2017;14(5):661–7. https://doi.org/10.1016/j.hrthm.2017.01.003 ([published Online First: Epub Date]|).
Vogler J, Willems S, Sultan A, et al. Pulmonary vein isolation versus defragmentation: the CHASE-AF clinical trial. J Am Coll Cardiol. 2015;66(24):2743–52.
Wynn GJ, Panikker S, Morgan M, et al. Biatrial linear ablation in sustained nonpermanent AF: results of the substrate modification with ablation and antiarrhythmic drugs in nonpermanent atrial fibrillation (SMAN-PAF) trial. Heart Rhythm. 2016;13(2):399–406.
Khurram IM, Habibi M, GucukIpek E, et al. Left atrial LGE and arrhythmia recurrence following pulmonary vein isolation for paroxysmal and persistent AF. JACC: Cardiovascular Imaging. 2016;9(2):142–8.
Mark DB, Anstrom KJ, Sheng S, et al. Effect of Catheter Ablation vs Medical Therapy on Quality of Life Among Patients With Atrial Fibrillation. JAMA. 2019;321(13):1275. https://doi.org/10.1001/jama.2019.0692 ([published Online First: Epub Date]|).
Evans JM, Withers KL, Lencioni M, et al. Quality of life benefits from arrhythmia ablation: A longitudinal study using the C-CAP questionnaire and EQ5D. Pacing Clin Electrophysiol. 2019;42(6):705–11. https://doi.org/10.1111/pace.13675 ([published Online First: Epub Date]|).
Funding
The Advisor™ HD Grid Observational Study was supported by the manufacturer of the Advisor™ HD Grid Mapping Catheter, Sensor Enabled, Abbott Laboratories.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The conduct of the clinical study was in accordance with the Declaration of Helsinki and approved by the appropriate Ethics Committee of the respective clinical sites and as specified by local regulation.
Consent to participate
All patients enrolled in the study provided written informed consent.
Conflict of interest
D.S. has received personal fees from Abbott, grants from Abbott and Boston Scientific, and other support from Biotronik. H.H. has received honoraria for lectures and proctoring from Abbott and Boston Scientific. J.L. has received consulting fees and grants or contracts from Abbott and Biosense Webster. All remaining authors have declared no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fiedler, L., Roca, I., Lorgat, F. et al. Characterization of high-density mapping in catheter ablation for persistent atrial fibrillation: results from the Advisor™ HD Grid Mapping Catheter Observational study. J Interv Card Electrophysiol 66, 1411–1421 (2023). https://doi.org/10.1007/s10840-022-01442-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01442-3