Abstract
Purpose
Catheter ablation of premature ventricular contractions (PVCs) is highly successful and has become the hallmark treatment for symptomatic or highly prevalent cases. However, few studies exist that evaluate the outcomes of ablation and likely mechanisms of PVC recurrence beyond 1 year of follow-up.
Methods
This study is a retrospective analysis of patients who underwent catheter ablation for symptomatic PVCs with acute procedural success and had clinical follow-up ≥ 12 months.
Results
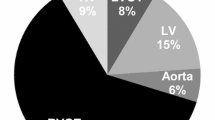
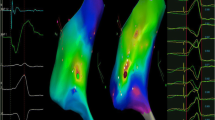
Forty-four patients (24 women; age 53.5 ± 4.8 years) following acutely successful PVC ablation with long-term follow-up were studied. At a mean of 36 ± 6 months, overall long-term ablation success was 75% (33/44 patients). Notably, recurrence of the targeted PVC focus was low (6.8%, 3/44 patients); the majority of recurrences were from a new source location (18.2%, 8/44 patients). The time course for targeted versus de novo PVC recurrences was significantly different: recurrence of a PVC similar to the targeted PVC morphology occurred at a mean of 5.0 ± 2.0 months, while recurrence of a PVC different from the index case occurred at a mean of 35.8 ± 17.1 months (p = 0.01). Non-ischemic cardiomyopathy was associated with increased risk of PVC recurrence (odds ratio [OR] 14.50 (95% confidence interval [CI] 1.92–109.33, p = 0.01)) and was a significant negative prognostic factor in multivariate analysis for PVC recurrence survival (hazard ratio [HR] 4.63, 95% CI 1.03–20.74, p = 0.04).
Conclusions
The majority of long-term PVC recurrences occur late in follow-up, at locations remote from the targeted PVC source or sources. Such sites may represent ongoing substrate evolution; additional work is required to determine the precise substrate alterations which promote such arrhythmogenic changes.
Similar content being viewed by others
Abbreviations
- ECG:
-
Electrocardiogram
- PVC:
-
Premature ventricular contraction
- RVOT:
-
Right ventricular outflow tract
- LVOT:
-
Left ventricular outflow tract
References
Latchamsetty R, Bogun F. Premature ventricular complexes and premature ventricular complex induced cardiomyopathy. Curr Probl Cardiol. 2015;40:379–422.
Badhwar N, Scheinman MM. Idiopathic ventricular tachycardia: diagnosis and management. Curr Probl Cardiol. 2007;32:7–43.
Chugh SS, Shen WK, Luria DM, Smith HC. First evidence of premature ventricular complex-induced cardiomyopathy: a potentially reversible cause of heart failure. J Cardiovasc Electrophysiol. 2000;11:328–9.
Hoffmayer KS, Gerstenfeld EP. Diagnosis and management of idiopathic ventricular tachycardia. Curr Probl Cardiol. 2013;38:131–58.
Yarlagadda RK, Iwai S, Stein KM, Markowitz SM, Shah BK, Cheung JW, et al. Reversal of cardiomyopathy in patients with repetitive monomorphic ventricular ectopy originating from the right ventricular outflow tract. Circulation. 2005;112:1092–7.
Bala R, Garcia FC, Hutchinson MD, Gerstenfeld EP, Dhruvakumar S, Dixit S, et al. Electrocardiographic and electrophysiologic features of ventricular arrhythmias originating from the right/left coronary cusp commissure. Heart Rhythm : Off J Heart Rhythm Soc. 2010;7:312–22.
Bogun F, Crawford T, Reich S, Koelling TM, Armstrong W, Good E, et al. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: comparison with a control group without intervention. Heart Rhythm : Off J Heart Rhythm Soc. 2007;4:863–7.
Chinushi M, Aizawa Y, Ohhira K, Fujita S, Shiba M, Niwano S, et al. Repetitive ventricular responses induced by radiofrequency ablation for idiopathic ventricular tachycardia originating from the outflow tract of the right ventricle. Pacing Clin Electrophysiol : PACE. 1998;21:669–78.
Good E, Desjardins B, Jongnarangsin K, Oral H, Chugh A, Ebinger M, et al. Ventricular arrhythmias originating from a papillary muscle in patients without prior infarction: a comparison with fascicular arrhythmias. Heart Rhythm : Off J Heart Rhythm Soc. 2008;5:1530–7.
Jauregui Abularach ME, Campos B, Park KM, Tschabrunn CM, Frankel DS, Park RE, et al. Ablation of ventricular arrhythmias arising near the anterior epicardial veins from the left sinus of Valsalva region: ECG features, anatomic distance, and outcome. Heart Rhythm : Off J Heart Rhythm Soc. 2012;9:865–73.
John RM, Stevenson WG. Catheter-based ablation for ventricular arrhythmias. Curr Cardiol Rep. 2011;13:399–406.
Joshi S, Wilber DJ. Ablation of idiopathic right ventricular outflow tract tachycardia: current perspectives. J Cardiovasc Electrophysiol. 2005;16(Suppl 1):S52–8.
Kottkamp H, Chen X, Hindricks G, Willems S, Haverkamp W, Wichter T, et al. Idiopathic left ventricular tachycardia: new insights into electrophysiological characteristics and radiofrequency catheter ablation. Pacing Clin Electrophysiol : PACE. 1995;18:1285–97.
Kumagai K, Yamauchi Y, Takahashi A, Yokoyama Y, Sekiguchi Y, Watanabe J, et al. Idiopathic left ventricular tachycardia originating from the mitral annulus. J Cardiovasc Electrophysiol. 2005;16:1029–36.
Latif S, Dixit S, Callans DJ. Ventricular arrhythmias in normal hearts. Cardiol Clin. 2008;26:367–80 vi.
Movsowitz C, Schwartzman D, Callans DJ, Preminger M, Zado E, Gottlieb CD, et al. Idiopathic right ventricular outflow tract tachycardia: narrowing the anatomic location for successful ablation. Am Heart J. 1996;131:930–6.
Tada H, Ito S, Naito S, Kurosaki K, Kubota S, Sugiyasu A, et al. Idiopathic ventricular arrhythmia arising from the mitral annulus: a distinct subgroup of idiopathic ventricular arrhythmias. J Am Coll Cardiol. 2005;45:877–86.
Tada H, Tadokoro K, Ito S, Naito S, Hashimoto T, Kaseno K, et al. Idiopathic ventricular arrhythmias originating from the tricuspid annulus: prevalence, electrocardiographic characteristics, and results of radiofrequency catheter ablation. Heart Rhythm :Off J Heart Rhythm Soc. 2007;4:7–16.
Yamada T, McElderry HT, Doppalapudi H, Murakami Y, Yoshida Y, Yoshida N, et al. Idiopathic ventricular arrhythmias originating from the aortic root prevalence, electrocardiographic and electrophysiologic characteristics, and results of radiofrequency catheter ablation. J Am Coll Cardiol. 2008;52:139–47.
Yamada T, McElderry HT, Okada T, Murakami Y, Doppalapudi H, Yoshida N, et al. Idiopathic focal ventricular arrhythmias originating from the anterior papillary muscle in the left ventricle. J Cardiovasc Electrophysiol. 2009;20:866–72.
Betensky BP, Park RE, Marchlinski FE, Hutchinson MD, Garcia FC, Dixit S, et al. The V(2) transition ratio: a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin. J Am Coll Cardiol. 2011;57:2255–62.
Buxton AE, Waxman HL, Marchlinski FE, Simson MB, Cassidy D, Josephson ME. Right ventricular tachycardia: clinical and electrophysiologic characteristics. Circulation. 1983;68:917–27.
Dixit S, Gerstenfeld EP, Callans DJ, Marchlinski FE. Electrocardiographic patterns of superior right ventricular outflow tract tachycardias: distinguishing septal and free-wall sites of origin. J Cardiovasc Electrophysiol. 2003;14:1–7.
Hachiya H, Aonuma K, Yamauchi Y, Igawa M, Nogami A, Iesaka Y. How to diagnose, locate, and ablate coronary cusp ventricular tachycardia. J Cardiovasc Electrophysiol. 2002;13:551–6.
Ito S, Tada H, Naito S, Kurosaki K, Ueda M, Hoshizaki H, et al. Development and validation of an ECG algorithm for identifying the optimal ablation site for idiopathic ventricular outflow tract tachycardia. J Cardiovasc Electrophysiol. 2003;14:1280–6.
Lin D, Ilkhanoff L, Gerstenfeld E, Dixit S, Beldner S, Bala R, et al. Twelve-lead electrocardiographic characteristics of the aortic cusp region guided by intracardiac echocardiography and electroanatomic mapping. Heart Rhythm :Off J Heart Rhythm Soc. 2008;5:663–9.
Sekiguchi Y, Aonuma K, Takahashi A, Yamauchi Y, Hachiya H, Yokoyama Y, et al. Electrocardiographic and electrophysiologic characteristics of ventricular tachycardia originating within the pulmonary artery. J Am Coll Cardiol. 2005;45:887–95.
Yamada T, Doppalapudi H, McElderry HT, Okada T, Murakami Y, Inden Y, et al. Idiopathic ventricular arrhythmias originating from the papillary muscles in the left ventricle: prevalence, electrocardiographic and electrophysiological characteristics, and results of the radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 2010;21:62–9.
Yamada T, Yoshida N, Murakami Y, Okada T, Muto M, Murohara T, et al. Electrocardiographic characteristics of ventricular arrhythmias originating from the junction of the left and right coronary sinuses of Valsalva in the aorta: the activation pattern as a rationale for the electrocardiographic characteristics. Heart Rhythm :Off J Heart Rhythm Soc. 2008;5:184–92.
Yoshida N, Yamada T, McElderry HT, Inden Y, Shimano M, Murohara T, et al. A novel electrocardiographic criterion for differentiating a left from right ventricular outflow tract tachycardia origin: the V2S/V3R index. J Cardiovasc Electrophysiol. 2014;25:747–53.
Baser K, Bas HD, Belardi D, Yokokawa M, Good E, Latchamsetty R, et al. Predictors of outcome after catheter ablation of premature ventricular complexes. J Cardiovasc Electrophysiol. 2014;25:597–601.
Zhang F, Yang B, Chen H, Ju W, Kojodjojo P, Cao K, et al. Noncontact mapping to guide ablation of right ventricular outflow tract arrhythmias. Heart Rhythm : Off J Heart Rhythm Soc. 2013;10:1895–902.
Lalani GG, Coysh T, Baykaner T, Zaman J, Hopper K, Schricker AA, et al. Organized sources are spatially conserved in recurrent compared to pre-ablation atrial fibrillation: further evidence for non-random electrical substrates. J Cardiovasc Electrophysiol. 2016;27:661–9.
Dimitri H, Ng M, Brooks AG, Kuklik P, Stiles MK, Lau DH, et al. Atrial remodeling in obstructive sleep apnea: implications for atrial fibrillation. Heart Rhythm : Off J Heart Rhythm Soc. 2012;9:321–7.
Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol. 2014;64:2222–31.
El Kadri M, Yokokawa M, Labounty T, Mueller G, Crawford T, Good E, et al. Effect of ablation of frequent premature ventricular complexes on left ventricular function in patients with nonischemic cardiomyopathy. Heart Rhythm : Off J Heart Rhythm Soc. 2015;12:706–13.
Nazarian S, Bluemke DA, Lardo AC, Zviman MM, Watkins SP, Dickfeld TL, et al. Magnetic resonance assessment of the substrate for inducible ventricular tachycardia in nonischemic cardiomyopathy. Circulation. 2005;112:2821–5.
Wijeysundera HC, Hansen MS, Stanton E, Cropp AS, Hall C, Dhalla NS, et al. Neurohormones and oxidative stress in nonischemic cardiomyopathy: relationship to survival and the effect of treatment with amlodipine. Am Heart J. 2003;146:291–7.
Financial support
This study was financially supported by the UCSD Clinical Translational Research Institute (GEM Grant), the University of California Center for Accelerated Innovation, the UCSD Rady MEET Grant to DEK, and National Institutes of Health (Grant 5T35HL007491) to DL.
Author information
Authors and Affiliations
Contributions
Derek Lee: Data analysis/interpretation, drafting article, statistics.
Kurt S. Hoffmayer: Critical revision of article, statistics, approval of article.
Jonathan C. Hsu: IRB approval secured by, data collection, approval of article.
Amir Schricker: Data generation, approval of article.
Ulrika Birgersdotter-Green: Critical revision of article, approval of article.
Farshad Raissi: Data generation, approval of article.
Gregory K. Feld: Data generation, approval of article.
David E. Krummen: Funding secured by, concept/design, data generation, drafting article, critical revision of article, approval of article.
Corresponding author
Ethics declarations
This study was conducted under an institution review board-approved protocol for the retrospective analysis of patients following catheter ablation at the University of California San Diego Medical Center.
Conflict of interest
Lee: This author declares that he has no conflict of interest.
Hsu: Honoraria from Medtronic, St. Jude Medical, Boston Scientific, and Biotronik. Consulting for 3DT Holdings. Research grants from Biotronik, Biosense Webster.
Feld: Equity and Board of Directors for Perminova, Inc.
Krummen: Consulting for Abbott Laboratories. Equity in Vektor Medical.
Hoffmayer, Schricker, Hsu, Birgersdotter-Green, Raissi, Feld, and Krummen: EP Fellowship support from Abbott Laboratories, Biosense Webster, Biotronik, Boston Scientific, and Medtronic.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Lee, D., Hoffmayer, K.S., Hsu, J.C. et al. Long-term mode and timing of premature ventricular complex recurrence following successful catheter ablation. J Interv Card Electrophysiol 55, 153–160 (2019). https://doi.org/10.1007/s10840-019-00520-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00520-3