Abstract
Purpose
Left atrial catheter ablation for patients with atrial fibrillation (AF) requires periprocedural anticoagulation to minimize thromboembolic complications. High rates of major bleeding complications using dabigatran etexilate for periprocedural anticoagulation have been reported, raising concerns regarding its safety during left atrial catheter ablation. We sought to evaluate the safety and efficacy of a dabigatran use strategy versus warfarin, at a single high-volume AF ablation center.
Methods
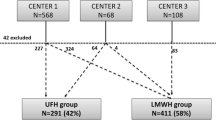
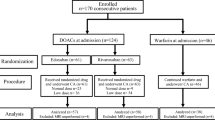
We performed a retrospective analysis on consecutive patients undergoing left atrial ablation at Vanderbilt Medical Center from January 2011 through August 2012 with a minimum follow-up of 3 months. Patient cohorts were divided into two groups, those utilizing dabigatran etexilate pre- and post-ablation and those undergoing ablation on dose-adjusted warfarin, with or without low-molecular-weight heparin bridging. Dabigatran was held 24–30 h pre-procedure and restarted 4–6 h after hemostasis was achieved. We evaluated all thromboembolic and bleeding complications at 3 months post-ablation.
Results
A total of 254 patients underwent left atrial catheter ablation for atrial fibrillation or left atrial flutter. Periprocedural anticoagulation utilized dabigatran in 122 patients and warfarin in 135 patients. Three late thromboembolic complications occurred in the dabigatran group (2.5 %), compared with one (0.7 %) in the warfarin group (p = 0.28). The dabigatran group had similar minor bleeding (2.5 vs. 7.4 %, p = 0.07), major bleeding (1.6 vs. 0.7 %, p = 0.51), and composite of bleeding and thromboembolic complications (6.6 vs. 8.9 %, p = 0.49) when compared to warfarin. There were no acute thromboembolic complications in either group (<24 h post-ablation).
Conclusions
In patients undergoing left atrial catheter ablation for AF or left atrial flutter, use of periprocedural dabigatran etexilate provides a safe and effective anticoagulation strategy compared to warfarin. A prospective randomized study is warranted.
Similar content being viewed by others
References
Fisher, J. D., Spinelli, M. A., Mookherjee, D., Krumerman, A. K., & Palma, E. C. (2006). Atrial fibrillation ablation: reaching the mainstream. [Meta-analysis research support, Non-US Gov’t Review]. Pacing and Clinical Electrophysiology: PACE, 29(5), 523–537.
Cappato, R., Calkins, H., Chen, S. A., Davies, W., Iesaka, Y., Kalman, J., et al. (2010). Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. Arrhythmia and Electrophysiology, 3(1), 32–38.
Scherr, D., Sharma, K., Dalal, D., Spragg, D., Chilukuri, K., Cheng, A., et al. (2009). Incidence and predictors of periprocedural cerebrovascular accident in patients undergoing catheter ablation of atrial fibrillation. [Research support, Non-US Gov’t]. Journal of Cardiovascular Electrophysiology, 20(12), 1357–1363.
Vazquez, S. R., Johnson, S. A., & Rondina, M. T. (2010). Peri-procedural anticoagulation in patients undergoing ablation for atrial fibrillation. [Review]. Thrombosis Research, 126(2), e69–e77.
Viles-Gonzalez, J. F., & Mehta, D. (2011). Thromboembolic risk and anticoagulation strategies in patients undergoing catheter ablation for atrial fibrillation. [Review]. Current Cardiology Reports, 13(1), 38–42.
Di Biase, L., Burkhardt, J. D., Mohanty, P., Sanchez, J., Horton, R., Gallinghouse, G. J., et al. (2010). Periprocedural stroke and management of major bleeding complications in patients undergoing catheter ablation of atrial fibrillation: the impact of periprocedural therapeutic international normalized ratio. [Comparative study multicenter study research support, Non-US Gov’t]. Circulation, 121(23), 2550–2556.
Hakalahti, A., Uusimaa, P., Ylitalo, K., & Raatikainen, M. J. (2011). Catheter ablation of atrial fibrillation in patients with therapeutic oral anticoagulation treatment. [Clinical trial research support, Non-US Gov’t]. Europace, 13(5), 640–645.
Hussein, A. A., Martin, D. O., Saliba, W., Patel, D., Karim, S., Batal, O., et al. (2009). Radiofrequency ablation of atrial fibrillation under therapeutic international normalized ratio: a safe and efficacious periprocedural anticoagulation strategy. Heart Rhythm, 6(10), 1425–1429.
Santangeli, P., Di Biase, L., Sanchez, J. E., Horton, R., & Natale, A. (2011). Atrial fibrillation ablation without interruption of anticoagulation. Cardiology Research and Practice, 2011, 837841.
Wazni, O. M., Beheiry, S., Fahmy, T., Barrett, C., Hao, S., Patel, D., et al. (2007). Atrial fibrillation ablation in patients with therapeutic international normalized ratio: comparison of strategies of anticoagulation management in the periprocedural period. [Clinical trial comparative study controlled clinical trial]. Circulation, 116(22), 2531–2534.
Abhishek, F., Heist, E. K., Barrett, C., Danik, S., Blendea, D., Correnti, C., et al. (2011). Effectiveness of a strategy to reduce major vascular complications from catheter ablation of atrial fibrillation. [Research Support, Non-US Gov’t]. Journal of Interventional Cardiac Electrophysiology: An International Journal of Arrhythmias and Pacing, 30(3), 211–215.
Wann, L. S., Curtis, A. B., Ellenbogen, K. A., Estes, N. A., 3rd, Ezekowitz, M. D., Jackman, W. M., et al. (2011). 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on dabigatran): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. [Practice guideline]. Journal of the American College of Cardiology, 57(11), 1330–1337.
Connolly, S. J., Ezekowitz, M. D., Yusuf, S., Eikelboom, J., Oldgren, J., Parekh, A., et al. (2009). Dabigatran versus warfarin in patients with atrial fibrillation. [Comparative study multicenter study randomized controlled trial research support, Non-US Gov’t]. The New England Journal of Medicine, 361(12), 1139–1151.
Calkins, H., Kuck, K. H., Cappato, R., Brugada, J., Camm, A. J., Chen, S. A., et al. (2012). 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace, 14(4), 528–606.
Lakkireddy, D., Reddy, Y. M., Di Biase, L., Vanga, S. R., Santangeli, P., Swarup, V., et al. (2012). Feasibility and safety of dabigatran versus warfarin for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation: results from a multicenter prospective registry. Journal of the American College of Cardiology, 59(13), 1168–1174.
van Ryn, J., Stangier, J., Haertter, S., Liesenfeld, K. H., Wienen, W., Feuring, M., et al. (2010). Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. [Review]. Thrombosis and Haemostasis, 103(6), 1116–1127.
Stangier, J., Rathgen, K., Stahle, H., Gansser, D., & Roth, W. (2007). The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. [Randomized controlled trial]. British Journal of Clinical Pharmacology, 64(3), 292–303.
Stangier, J., Eriksson, B. I., Dahl, O. E., Ahnfelt, L., Nehmiz, G., Stahle, H., et al. (2005). Pharmacokinetic profile of the oral direct thrombin inhibitor dabigatran etexilate in healthy volunteers and patients undergoing total hip replacement. [Clinical trial clinical trial, phase i clinical trial, phase ii multicenter study randomized controlled trial research support, Non-US Gov’t]. The Journal of Clinical Pharmacology, 45(5), 555–563.
Stangier, J., Stahle, H., Rathgen, K., & Fuhr, R. (2008). Pharmacokinetics and pharmacodynamics of the direct oral thrombin inhibitor dabigatran in healthy elderly subjects. [Randomized controlled trial research support, Non-US Gov’t]. Clinical Pharmacokinetics, 47(1), 47–59.
Garnock-Jones, K. P. (2011). Dabigatran etexilate: a review of its use in the prevention of stroke and systemic embolism in patients with atrial fibrillation. American Journal of Cardiovascular Drugs: Drugs, Devices, and Other Interventions, 11(1), 57–72.
Sanford, M., & Plosker, G. L. (2008). Dabigatran etexilate. Drugs, 68(12), 1699–1709.
Takahashi, A., Kuwahara, T., & Takahashi, Y. (2009). Complications in the catheter ablation of atrial fibrillation: incidence and management. [Review]. Circulation Journal, 73(2), 221–226.
Gaita, F., Caponi, D., Pianelli, M., Scaglione, M., Toso, E., Cesarani, F., et al. (2010). Radiofrequency catheter ablation of atrial fibrillation: a cause of silent thromboembolism? Magnetic resonance imaging assessment of cerebral thromboembolism in patients undergoing ablation of atrial fibrillation. [comparative study multicenter study]. Circulation, 122(17), 1667–1673.
Knight, B. P. (2012). Anticoagulation for atrial fibrillation ablation: what is the optimal strategy? [Comment editorial]. Journal of the American College of Cardiology, 59(13), 1175–1177.
Stangier, J., Rathgen, K., Stahle, H., & Mazur, D. (2010). Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. [Clinical trial research support, Non-US Gov’t]. Clinical Pharmacokinetics, 49(4), 259–268.
Winkle, R. A., Mead, R. H., Engel, G., Kong, M. H., & Patrawala, R. A. (2012). The use of dabigatran immediately after atrial fibrillation ablation. Journal of Cardiovascular Electrophysiology, 23(3), 264–268.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kaiser, D.W., Streur, M.M., Nagarakanti, R. et al. Continuous warfarin versus periprocedural dabigatran to reduce stroke and systemic embolism in patients undergoing catheter ablation for atrial fibrillation or left atrial flutter. J Interv Card Electrophysiol 37, 241–247 (2013). https://doi.org/10.1007/s10840-013-9793-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-013-9793-7