Abstract
Purpose
Platelet-rich plasma (PRP) has become a novel treatment in various aspects of medicine including orthopedics, cardiothoracic surgery, plastic surgery, dermatology, dentistry, and diabetic wound healing. PRP is now starting to become an area of interest in reproductive medicine more specifically focusing on infertility. Poor ovarian reserve, menopause, premature ovarian failure, and thin endometrium have been the main areas of research. The aim of this article is to review the existing literature on the effects of autologous PRP in reproductive medicine providing a summation of the current studies and assessing the need for additional research.
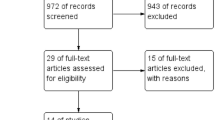
Methods
A literature search is performed using PubMed, MEDLINE, and CINAHL Plus to identify studies focusing on the use of PRP therapy in reproductive medicine. Articles were divided into 3 categories: PRP in thin lining, PRP in poor ovarian reserve, and PRP in recurrent implantation failure.
Results
In women with thin endometrium, the literature shows an increase in endometrial thickness and increase in chemical and clinical pregnancy rates following autologous PRP therapy. In women with poor ovarian reserve, autologous intraovarian PRP therapy increased anti-Mullerian hormone (AMH) levels and decreased follicle-stimulating hormone (FSH), with a trend toward increasing clinical and live birth rates. This trend was also noted in women with recurrent implantation failure.
Conclusions
Limited literature shows promise in increasing endometrial thickness, increasing AMH, and decreasing FSH levels, as well as increasing chemical and clinical pregnancy rates. The lack of standardization of PRP preparation along with the lack of large randomized controlled trials needs to be addressed in future studies. Until definitive large RCTs are available, PRP use should be considered experimental.
Similar content being viewed by others
Data availability
Not applicable
Code availability
Not applicable
References
Aghajanova L, Houshdaran S, Balayan S, Manvelyan E, Irwin J, Huddleston H, et al. In vitro evidence that platelet-rich plasma stimulates cellular processes involved in endometrial regeneration. J Assist Reprod Genet. 2018;35:757–70.
Kim H, Shin J, Koo H, Kwon H, Choi D, Kim J. Effect of autologous platelet-rich plasma treatment on refractory thin endometrium during the frozen embryo transfer cycle: a pilot study. Front Endocrinol. 2019;10:1–9.
Mouhayar Y, Sharara FI. G-CSF and stem cell therapy for the treatment of refractory thin lining in assisted reproductive technology. J Assist Reprod Genet. 2017;34:831–7.
Du J, Lu H, Yu X, Lu Z, Mi L, Zhang X. Efficacy and safety of platelet-rich plasma for the treatment of thin endometrium: a protocol for systematic review and meta-analysis. Medicine. 2020;99:1–4.
Coksuer H, Akdemir Y, Barut M. Improved in vitro fertilization success and pregnancy outcome with autologous platelet-rich plasma treatment in unexplained infertility patients that had repeated implantation failure history. Gynecol Endocrinol. 2019:1–6.
Eftekhar M, Neghab N, Naghshineh E, Khani P. Can autologous platelet rich plasma expand endometrial thickness and improve pregnancy rate during frozen-thawed embryo transfer cycle? A randomized clinical trial. Taiwan J Obstet Gynecol. 2018;57:810–3.
Chang Y, Li J, Chen Y, Wei L, Yang X, Shi Y, et al. Autologous platelet-rich plasma promotes endometrial growth and improves pregnancy outcome during in vitro fertilization. Int J Clin Exp Med. 2015;8:1286–90.
Farimani M, Poorolajal J, Rabiee S, Bahmanzadeh M. Successful pregnancy and live birth after intrauterine administration of autologous platelet-rich plasma in a woman with recurrent implantation failure: a case report. Int J Reprod BioMed. 2017;15:803–6.
Nazari L, Salehpour S, Hoseini S, Zadehmodarres S, Azargashb E. Effects of autologous platelet-rich plasma on endometrial expansion in patients undergoing frozen-thawed embryo transfer: a double-blind RCT. Int J Reprod BioMed. 2019;17:443–8.
Jirge P. Poor ovarian reserve. J Hum Reprod Sci. 2016;9:63–9.
Pantos K, Simopoulou M, Pantou A, Rapani A, Tsioulou P, Nitsos N, et al. A case series on natural conceptions resulting in ongoing pregnancies in menopausal and prematurely menopausal women following platelet-rich plasma treatment. Cell Transplant. 2019;28:1333–40.
Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42(3):610–8.
Jo CH, Shin JS, Lee YG, Shin WH, Kim H, Lee SY, et al. Platelet-rich plasma for arthroscopic repair of large to massive rotator cuff tears: a randomized, single-blind, parallel-group trial. Am J Sports Med. 2013;41(10):2240–8.
Cervelli V, Gentile P, Scioli MG, Grimaldi M, Casciani CU, Spagnoli LG, et al. Application of platelet-rich plasma in plastic surgery: clinical and in vitro evaluation. Tissue Eng Part C Methods. 2009;15(4):625–34.
Picard F, Hersant B, Bosc R, Meningaud JP. The growing evidence for the use of platelet-rich plasma on diabetic chronic wounds: a review and a proposal for a new standard care. Wound Repair Regen. 2015;23(5):638–43.
Dawood A, Salem H. Current clinical applications of platelet-rich plasma in various gynecological disorders: an appraisal of theory and practice. Clin Exp Reprod Med. 2018;45:67–74.
Dhurat R, Sukesh MS. Principles and methods of preparation of platelet-rich plasma: a review and author’s perspective. J Cutan Aesthet Surg. 2014;7:189–97.
Bos-Mikich A, de Oliveira R, Frantz N. Platelet-rich plasma therapy and reproductive medicine. J Assist Reprod Genet. 2018;35:753–6.
Kamath M, Mascarenhas M, Franik S, Liu E, Sunkara K. Clinical adjuncts in in vitro fertilization: a growing list. Fertil Steril. 2019:1–9.
Cavallo C, Roffi A, Grigolo B, Mariani E, Pratelli L, Merli G, et al. Platelet-rich plasma: the choice of activation method affects the release of bioactive molecules. BioMed Research International. 2016;2016:1–7.
Chang Y, Li J, Wei L, Pang J, Chen J, Liang X. Autologous platelet-rich plasma infusion improves clinical pregnancy rate in frozen embryo transfer cycles for women with thin endometrium. Medicine. 2019;98:1–5.
Frantz N, Ferreira M, Kulmann M, Frantz G, Bos-Mikich A, Oliveira R. Platelet-rich plasma as an effective alternative approach for improving endometrial receptivity-a clinical retrospective study. JBRA Assist Reprod. 2020:1–5.
Zadehmodarres S, Salehpour S, Saharkhiz N, Nazari L. Treatment of thin endometrium with autologous platelet-rich plasma: a pilot study. JBRA Assit Reprod. 2017;21:54–6.
Tandulwadkar S, Naralkar M, Surana D, Selvakarthick M, Kharat A. Autologous intrauterine platelet-rich plasma instillation for suboptimal endometrium in frozen embryo transfer cycles: a pilot study. J Hum Reprod Sci. 2017;10:208–12.
Chang Y, Li J, Wei LN, Pang J, Chen J, Liang X. Autologous platelet-rich plasma infusion improves clinical pregnancy rate in frozen embryo transfer cycles for women with thin endometrium. Medicine (Baltimore). 2019;98(3):e14062. https://doi.org/10.1097/MD.0000000000014062.
Nazari L, Salehpour S, Hosseini M, Moghanjoughi M. The effects of autologous platelet-rich plasma in repeated implantation failure: a randomized controlled trial. Hum Fertil. 2018:1–6.
Sills E, Rickers N, Li X, Palermo G. First data on in vitro fertilization and blastocyst formation after intraovarian injection of calcium gluconate-activated autologous platelet rich plasma. Gynecol Endocrinol. 2018;34:756–60.
Sfakianoudis K, Simopoulou M, Nitsos N, Rapani A, Pantou A, Vaxevanoglou T, et al. A case series on platelet-rich plasma revolutionary management of poor responder patients. Gynecol Obstet Invest. 2018;84:99–106.
Cakiroglu Y, Saltik A, Yuceturk A, Karaosmanoglu O, Kopuk S, Scott R, et al. Effects of intraovarian injection of autologous platelet rich plasma on ovarian reserve and IVF outcome parameters in women with primary ovarian insufficiency. Aging. 2020;12:10211–22.
Hsu C, Hsu L, Hsu I, Chiu Y, Dorjee S. Live birth in woman with premature ovarian insufficiency receiving ovarian administration of platelet-rich plasma (PRP) in combination with gonadotropin: a case report. Front Endocrinol. 2020;11:1–5.
Melo P, Navarro C, Jones C, Coward K, Coleman L. The use of autologous platelet-rich plasma (PRP) versus no intervention in women with low ovarian reserve undergoing fertility treatment: a non-randomized interventional study. J Assist Reprod Genet. 2020;37:855–63.
Sills SE, Rickers NS, Petersen JL, Li X, Wood SH. Regenerative effect of intraovarian injection of activated autologous platelet rich plasma: serum anti-mullerian hormone levels measured among poor-prognosis in vitro fertilization patients. Int J Regen Med. 2020;1(2):2–5.
Sills E, Wood S. Autologous activated platelet-rich plasma injection into adult human ovary tissue: molecular mechanism, analysis, and discussion of reproductive response. Biosci Rep. 2019;39:1–15.
Stojkovska S, Dimitrov G, Stamenkovska N, Hadzi-Lega M, Petanovski Z. Live birth rates in poor responders’ group after previous treatment with autologous platelet-rich plasma and low dose ovarian stimulation compared with poor responders used only low dose ovarian stimulation before in vitro fertilization. J Med Sci. 2019;7:3184–8.
Mehrafza M, Kabodmehri R, Nikpouri Z, Pourseify G, Raoufi A, Eftekhari A, et al. Comparing the impact of autologous platelet-rich plasma and granulocyte colony stimulating factor on pregnancy outcome in patients with repeated implantation failure. J Reprod Infertil. 2019;20:35–41.
Sfakianoudis K, Simopoulou M, Nitsos N, Lazaros L, Rapani A, Pantou A, et al. Successful implantation and live birth following autologous platelet-rich plasma treatment for a patient with recurrent implantation failure and chronic endometritis. In Vivo. 2019;33:515–21.
Aghajanzadeh F, Esmaeilzadeh S, Basirat Z, Mahouti T, Heidari F, Golsorkhtabaramiri M. Using autologous intrauterine platelet-rich plasma to improve the reproductive outcomes of women with recurrent implantation failure. JBRA Assist. Reprod. 2020;24:30–3.
Zargar M, Pazhouhanfar R, Najafian M, Moradi CP. Effects of intrauterine autologous platelet-rich plasma infusions on outcomes in women with repetitive in vitro fertilization failures: a prospective randomized study. Clinical Experimental Obstet Gynecol. 2021;48(1):179–84.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sharara, F.I., Lelea, LL., Rahman, S. et al. A narrative review of platelet-rich plasma (PRP) in reproductive medicine. J Assist Reprod Genet 38, 1003–1012 (2021). https://doi.org/10.1007/s10815-021-02146-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02146-9