Abstract
Purpose
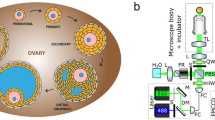
Mammalian oogenesis and folliculogenesis share a dynamic connection that is critical for gamete development. For maintenance of quiescence or follicular activation, follicles must respond to soluble signals (growth factors and hormones) and physical stresses, including mechanical forces and osmotic shifts. Likewise, mechanical processes are involved in cortical tension and cell polarity in oocytes. Our objective was to examine the contribution and influence of biomechanical signaling in female mammalian gametogenesis.
Methods
We performed a systematic review to assess and summarize the effects of mechanical signaling and mechanotransduction in oocyte maturation and folliculogenesis and to explore possible clinical applications. The review identified 2568 publications of which 122 met the inclusion criteria.
Results
The integration of mechanical and cell signaling pathways in gametogenesis is complex. Follicular activation or quiescence are influenced by mechanical signaling through the Hippo and Akt pathways involving the yes-associated protein (YAP), transcriptional coactivator with PDZ-binding motif (TAZ), phosphatase and tensin homolog deleted from chromosome 10 (PTEN) gene, the mammalian target of rapamycin (mTOR), and forkhead box O3 (FOXO3) gene.
Conclusions
There is overwhelming evidence that mechanical signaling plays a crucial role in development of the ovary, follicle, and oocyte throughout gametogenesis. Emerging data suggest the complexities of mechanotransduction and the biomechanics of oocytes and follicles are integral to understanding of primary ovarian insufficiency, ovarian aging, polycystic ovary syndrome, and applications of fertility preservation.





Similar content being viewed by others
References
John GB, Gallardo TD, Shirley LJ, Castrillon DH. Foxo3 is a PI3K-dependent molecular switch controlling the initiation of oocyte growth. Dev Biol. 2008;321:197–204.
Anderson RA, McLaughlin M, Wallace WHB, Albertini DF, Telfer EE. The immature human ovary shows loss of abnormal follicles and increasing follicle developmental competence through childhood and adolescence. Hum Reprod. 2014;29:97–106.
Ingber DE. Cellular mechanotransduction: putting all the pieces together again. FASEB J. 2006;20:1230–2.
Heisenberg CP, Bellaïche Y. Forces in tissue morphogenesis and patterning. Cell. 2013;153:948–62.
Albertini DF, Barrett SL. The developmental origins of mammalian oocyte polarity. Semin Cell Dev Biol. 2004;15:599–606.
Thorne JT, Segal TR, Chang S, Jorge S, Segars JH, Leppert PC. Dynamic reciprocity between cells and their microenvironment in reproduction. Biol Reprod. 2015;92:1–10.
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Jorge S, Chang S, Barzilai JJ, Leppert P, Segars JH. Mechanical signaling in reproductive tissues: mechanisms and importance. Reprod Sci. 2014;21:1093–107.
Hornick JE, Duncan FE, Shea LD, Woodruff TK. Isolated primate primordial follicles require a rigid physical environment to survive and grow in vitro. Hum Reprod. 2012;27:1801–10.
Shea LD, Woodruff TK, Shikanov A. Bioengineering the ovarian follicle microenvironment. Annu Rev Biomed Eng. 2014;16:29–52.
Xu M, West E, Shea LD, Woodruff TK. Identification of a stage-specific permissive in vitro culture environment for follicle growth and oocyte development. Biol Reprod. 2006;75:916–23.
West ER, Xu M, Woodruff TK, Shea LD. Physical properties of alginate hydrogels and their effects on in vitro follicle development. Biomaterials. 2007;28:4439–48.
West ER, Shea LD, Woodruff TK. Engineering the follicle microenvironment. Semin Reprod Med. 2007;25:287–99.
Shikanov A, Xu M, Woodruff TK, Shea LD. Interpenetrating fibrin–alginate matrices for in vitro ovarian follicle development. Biomaterials Elsevier Ltd. 2009;30:5476–85.
Smith RM, Woodruff TK, Shea LD. Designing follicle–environment interactions with biomaterials. Cancer Treat Res. 2010;156:11–24.
Woodruff TK, Shea LD. A new hypothesis regarding ovarian follicle development: ovarian rigidity as a regulator of selection and health. J Assist Reprod Genet. 2011;28:3–6.
Abel MH, Wootton AN, Wilkins V, Huhtaniemi I, Knight PG, Charlton HM. The effect of a null mutation in the follicle-stimulating hormone receptor gene on mouse reproduction. Endocrinology. 2000;141:1795–803.
McGee E, Hsueh AJ. Initial and cyclic recruitment of ovarian follicles. Endocr Rev. 2000;21:200–14.
Kawamura K, Cheng Y, Suzuki N, Deguchi M, Sato Y, Takae S, et al. Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proc Natl Acad Sci. 2013;110:17474–9.
Cordeiro CN, Christianson MS, Selter JH, Segars JH. In vitro activation: a possible new frontier for treatment of primary ovarian insufficiency. Reprod Sci. 2016;23:429–38.
Xiang C, Li J, Hu L, Huang J, Luo T, Zhong Z, et al. Hippo signaling pathway reveals a spatio-temporal correlation with the size of primordial follicle pool in mice. Cell Physiol Biochem. 2015;35:957–68.
Dupont S. Role of YAP/TAZ in cell–matrix adhesion-mediated signalling and mechanotransduction. Exp Cell Res Elsevier. 2016;343:42–53.
Dupont S, Morsut L, Aragona M, Enzo E, Giulitti S, Cordenonsi M, et al. Role of YAP/TAZ in mechanotransduction. Nature. 2011;474:179–83.
Provenzano PP, Keely PJ. Mechanical signaling through the cytoskeleton regulates cell proliferation by coordinated focal adhesion and rho GTPase signaling. J Cell Sci. 2011;124:1195–205.
Kawashima I, Kawamura K. Regulation of follicle growth through hormonal factors and mechanical cues mediated by hippo signaling pathway. Syst Biol Reprod Med. 2017:1–9.
Abbassi L, Malki S, Cockburn K, Macaulay A, Robert C, Rossant J, et al. Multiple mechanisms cooperate to constitutively exclude the transcriptional co-activator YAP from the nucleus during murine oogenesis. Biol Reprod. 2016;94:102.
Cheng Y, Feng Y, Jansson L, Sato Y, Deguchi M, Kawamura K, et al. Actin polymerization-enhancing drugs promote ovarian follicle growth mediated by the hippo signaling effector YAP. FASEB J. 2015;29:2423–30.
Brigstock DR. The connective tissue growth factor/cysteine-rich 61/nephroblastoma overexpressed (CCN) family. Endocr Rev. 1999;20:189–206.
Wada K, Itoga K, Okano T, Yonemura S, Sasaki H. Hippo pathway regulation by cell morphology and stress fibers. Development. 2011;138:3907–14.
Aragona M, Panciera T, Manfrin A, Giulitti S, Michielin F, Elvassore N, et al. A mechanical checkpoint controls multicellular growth through YAP/TAZ regulation by actin-processing factors. Cell. 2013;154:1047–59.
Cantley LC, Fruman DA, Meyers RE, Cantley LC, Lawlor MA, Alessi DR, et al. The phosphoinositide 3-kinase pathway. Science. 2002;296:1655–7.
Cecconi S, Mauro A, Cellini V, Patacchiola F. The role of Akt signalling in the mammalian ovary. Int J Dev Biol. 2012;56:809–17.
Li J, Kawamura K, Cheng Y, Liu S, Klein C, Liu S, et al. Activation of dormant ovarian follicles to generate mature eggs. Proc Natl Acad Sci. 2010;107:10280–4.
Ernst EH, Grøndahl ML, Grund S, Hardy K, Heuck A, Sunde L, et al. Dormancy and activation of human oocytes from primordial and primary follicles: molecular clues to oocyte regulation. Hum Reprod. 2017;32:1684–700.
Ezzati MM, Baker MD, Saatcioglu HD, Aloisio GM, Pena CG, Nakada Y, et al. Regulation of FOXO3 subcellular localization by kit ligand in the neonatal mouse ovary. J Assist Reprod Genet. 2015;32:1741–7.
Sobinoff AP, Sutherland JM, McLaughlin EA. Intracellular signalling during female gametogenesis. Mol Hum Reprod. 2013;19:265–78.
John GB, Shidler MJ, Besmer P, Castrillon DH. Kit signaling via PI3K promotes ovarian follicle maturation but is dispensable for primordial follicle activation. Dev Biol. 2010;331:292–9.
Jones RL, Pepling ME. KIT signaling regulates primordial follicle formation in the neonatal mouse ovary. Dev Biol Elsevier. 2013;382:186–97.
Saatcioglu HD, Cuevas I, Castrillon DH. Control of oocyte reawakening by kit. PLoS Genet. 2016;12:e1006215.
Reddy P, Shen L, Ren C, Boman K, Lundin E, Ottander U, et al. Activation of Akt (PKB) and suppression of FKHRL1 in mouse and rat oocytes by stem cell factor during follicular activation and development. Dev Biol. 2005;281:160–70.
Castrillon DH, Miao L, Kollipara R, Horner JW, DePinho RA. Suppression of ovarian follicle activation in mice by the transcription factor Foxo3a. Science (80-. ). 2003;301:215–8.
Sun HW, Tong SL, He J, Wang Q, Zou L, Ma SJ, et al. RhoA and RhoC-siRNA inhibit the proliferation and invasiveness activity of human gastric carcinoma by rho/PI3K/Akt pathway. World J Gastroenterol. 2007;13:3517–22.
Goto M, Iwase A, Ando H, Kurotsuchi S, Harata T, Kikkawa F. PTEN and Akt expression during growth of human ovarian follicles. J Assist Reprod Genet. 2007;24:541–6.
Kim SY, Ebbert K, Cordeiro MH, Romero M, Zhu J, Serna VA, et al. Cell autonomous phosphoinositide 3-kinase activation in oocytes disrupts normal ovarian function through promoting survival and overgrowth of ovarian follicles. Endocrinology. 2015;156:1464–76.
Reddy P, Liu L, Adhikari D, Jagarlamudi K, Rajareddy S, Shen Y, et al. Oocyte-specific deletion of Pten causes premature activation of the primordial follicle pool. Science (80-. ) 2008;319:611–3.
Reddy P, Adhikari D, Zheng W, Liang S, Hamalainen T, Tohonen V, et al. PDK1 signaling in oocytes controls reproductive aging and lifespan by manipulating the survival of primordial follicles. Hum Mol Genet. 2009;18:2813–24.
Jagarlamudi K, Liu L, Adhikari D, Reddy P, Idahl A, Ottander U, et al. Oocyte-specific deletion of Pten in mice reveals a stage-specific function of PTEN/PI3K signaling in oocytes in controlling follicular activation. PLoS One. 2009;4:3–9.
Cheng Y, Kim J, Li XX, Hsueh AJ. Promotion of ovarian follicle growth following mTOR activation: synergistic effects of AKT stimulators. PLoS One. 2015;10:1–9.
Tong Y, Li F, Lu Y, Cao Y, Gao J, Liu J. Rapamycin-sensitive mTORC1 signaling is involved in physiological primordial follicle activation in mouse ovary. Mol Reprod Dev. 2013;80:1018–34.
Adhikari D, Zheng W, Shen Y, Gorre N, Hämäläinen T, Cooney AJ, et al. Tsc/mTORC1 signaling in oocytes governs the quiescence and activation of primordial follicles. Hum Mol Genet. 2009;19:397–410.
Lu X, Guo S, Cheng Y, Kim JH, Feng Y, Feng Y. Stimulation of ovarian follicle growth after AMPK inhibition. Reproduction. 2017;153:683–94.
Zhao Y, Zhang Y, Li J, Zheng N, Xu X, Yang J, et al. MAPK3/1 participates in the activation of primordial follicles through mTORC1-KITL signaling. J Cell Physiol. 2018;233:226–37.
Adhikari D, Risal S, Liu K, Shen Y. Pharmacological inhibition of mTORC1 prevents over-activation of the primordial follicle pool in response to elevated PI3K signaling. PLoS One. 2013;8:e53810.
Zhang XM, Li L, Xu JJ, Wang N, Liu WJ, Lin XH, et al. Rapamycin preserves the follicle pool reserve and prolongs the ovarian lifespan of female rats via modulating mTOR activation and sirtuin expression. Gene. 2013;523:82–7.
Jiang Z-Z, Hu M-W, Ma X-S, Schatten H, Fan H-Y, Wang Z-B, et al. LKB1 acts as a critical gatekeeper of ovarian primordial follicle pool. Oncotarget. 2016;7:5738–53.
Ren Y, Suzuki H, Jagarlamudi K, Golnoski K, McGuire M, Lopes R, et al. Lhx8 regulates primordial follicle activation and postnatal folliculogenesis. BMC Biol. 2015;13:1–12.
Albertini DF, Combelles CMH, Benecchi E, Carabatsos MJ. Cellular basis for paracrine regulation of ovarian follicle development. Reproduction. 2001;121:647–53.
Da Silva-Buttkus P, Jayasooriya GS, Mora JM, Mobberley M, Ryder TA, Baithun M, et al. Effect of cell shape and packing density on granulosa cell proliferation and formation of multiple layers during early follicle development in the ovary. J Cell Sci. 2008;121:3890–900.
McLaughlin M, Bromfield JJ, Albertini DF, Telfer EE. Activin promotes follicular integrity and oogenesis in cultured pre-antral bovine follicles. Mol Hum Reprod. 2010;16:644–53.
Pangas SA, Rademaker AW, Fishman DA, Woodruff TK. Localization of the activin signal transduction components in normal human ovarian follicles: implications for autocrine and paracrine signaling in the ovary. J Clin Endocrinol Metab. 2002;87:2644–57.
Chang HM, Cheng JC, Liu Y, Klausen C, Xu C, Leung PCK. Activin A-induced increase in LOX activity in human granulosa-lutein cells is mediated by CTGF. Reproduction. 2016;152:293–301.
Chang HM, Fang Y, Liu PP, Cheng JC, Yang X, Leung PC. Connective tissue growth factor mediates growth differentiation factor 8-induced increase of lysyl oxidase activity in human granulosa-lutein cells. MolCell Endocrinol. 2016;434:186–98.
Fang Y, Chang HM, Cheng JC, Klausen C, Leung PCK, Yang X. Transforming growth factor-β1 increases lysyl oxidase expression by downregulating MIR29A in human granulose lutein cells. Reproduction. 2016;152:205–13.
Yang S, Wang S, Luo A, Ding T, Lai Z, Shen W, et al. Expression patterns and regulatory functions of microRNAs during the initiation of primordial follicle development in the neonatal mouse ovary. Biol Reprod. 2013;89:1–11.
He X, Toth TL. In vitro culture of ovarian follicles from Peromyscus. Semin Cell Dev Biol. 2017;61:140–9.
Zielak-Steciwko AE, Browne JA, McGettigan PA, Gajewska M, Dzieciol M, Szulc T, et al. Expression of microRNAs and their target genes and pathways associated with ovarian follicle development in cattle. Physiol Genomics. 2014;46:735–45.
Plancha CE, Sanfins A, Rodrigues P, Albertini D. Cell polarity during folliculogenesis and oogenesis. Reprod BioMed Online. 2005;10:478–84.
Rodgers RJ, Irving-Rodgers HF, Russell DL. Extracellular matrix of the developing ovarian follicle. Reproduction. 2003;126:415–24.
Bernal AL, Mardon H. Focal adhesion proteins in human granulosa cells. Reprod Technol. 2000;10:29–38.
Rodgers RJ, Irving-Rodgers HF. Formation of the ovarian follicular antrum and follicular fluid. Biol Reprod. 2010;82:1021–9.
Hsueh AJW, Kawamura K, Cheng Y, Fauser BCJM. Intraovarian control of early folliculogenesis. Endocr Rev. 2015;36:1–24.
Kino T, Segars JH, Chrousos GP. The guanine nucleotide exchange factor Brx: a link between osmotic stress, inflammation and organ physiology and pathophysiology. Expert Rev Endocrinol Metab. 2010;5:603–14.
Grive KJ, Freiman RN. The developmental origins of the mammalian ovarian reserve. Development. 2015;142:2554–63.
Bristol SK, Woodruff TK. Follicle-restricted compartmentalization of transforming growth factor beta superfamily ligands in the feline ovary. Biol Reprod. 2004;70:846–59.
Makker A, Goel MM, Mahdi AA. PI3K/PTEN/Akt and TSC/mTOR signaling pathways, ovarian dysfunction, and infertility: an update. J Mol Endocrinol. 2014;53:R103–18.
Ryan KE, Casey SM, Canthy MJ, Crowe MA, Martin F, Evans ACO. Akt and Erk signal transduction pathways are early markers of differentiation in dominant and subordinate ovarian follicles in cattle. Reproduction. 2007;133:617–26.
Evans AC, Martin F. Kinase pathways in dominant and subordinate ovarian follicles during the first wave of follicular development in sheep. Anim Reprod Sci. 2000;64:221–31.
Matousek M, Carati C, Gannon B, Brännström M. Novel method for intrafollicular pressure measurements in the rat ovary: increased intrafollicular pressure after hCG stimulation. Reproduction. 2001;121:307–14.
Richard S, Tartia AP, Boison D, Baltz JM. Mouse oocytes acquire mechanisms that permit independent cell volume regulation at the end of oogenesis. J Cell Physiol. 2016;232:2436–46.
Curry TE, Smith MF. Impact of extracellular matrix remodeling on ovulation and the folliculo-luteal transition. Semin Reprod Med. 2006;24:228–41.
Gubbay O, Guo W, Rae MT, Niven D, Langdon SP, Hillier SG. Inflammation-associated gene expression is altered between normal human ovarian surface epithelial cells and cell lines derived from ovarian adenocarcinomas. Br J Cancer. 2005;92:1927–33.
Puttabyatappa M, Al-Alem LF, Zakerkish F, Rosewell KL, Brännström M, Curry TE. Induction of tissue factor pathway inhibitor 2 by hCG regulates periovulatory gene expression and plasmin activity. Endocrinology. 2017;158:109–20.
Murdoch WJ, Gottsch ML. Proteolytic mechanisms in the ovulatory folliculo-luteal transformation. Connect Tissue Res. 2003;44:50–7.
Murdoch WJ. Regulation of collagenolysis and cell death by plasmin within the formative stigma of preovulatory ovine follicles. J Reprod Fertil. 1998;113:331–6.
Murdoch WJ, Colgin DC, Ellis JA. Role of tumor necrosis factor-a in the ovulatory mechanism of ewes. J Anim Sci. 1997;75:1601–5.
Ko C, Gieske MC, Al-Alem L, Hahn Y, Su W, Gong MC, et al. Endothelin-2 in ovarian follicle rupture. Endocrinology. 2006;147:1770–9.
Bridges PJ, Jo M, Al Alem L, Na G, Su W, Gong MC, et al. Production and binding of endothelin-2 (EDN2) in the rat ovary: endothelin receptor subtype a (EDNRA)-mediated contraction. Reprod Fertil Dev. 2010;22:780–7.
Al-Alem L, Bridges PJ, Su W, Gong MC, Iglarz M, Ko C. Endothelin-2 induces oviductal contraction via endothelin receptor subtype a in rats. J Endocrinol. 2007;193:383–91.
Rolaki A, Drakakis P, Millingos S, Loutradis D, Makrigiannakis A. Novel trends in follicular development, atresia and corpus luteum regression: a role for apoptosis. Reprod BioMed Online. 2005;11:93–103.
Evans JP, Robinson DN. The spatial and mechanical challenges of female meiosis. Mol Reprod Dev. 2011;78:769–77.
Larson SM, Lee HJ, Hung PH, Matthews LM, Robinson DN, Evans JP. Cortical mechanics and meiosis II completion in mammalian oocytes are mediated by myosin-II and ezrin–radixin–moesin (ERM) proteins. Mol Biol Cell. 2010;21:3182–92.
Hosseini SM, Moulavi F, Tanhaie-Vash N, Asgari V, Ghanaei HR, Abedi-Dorche M, et al. The principal forces of oocyte polarity are evolutionary conserved but may not affect the contribution of the first two blastomeres to the blastocyst development in mammals. PLoS One. 2016;11:e0148382.
Duan X, Liu J, Zhu CC, Wang QC, Cui XS, Kim NH, et al. RhoA-mediated MLC2 regulates actin dynamics for cytokinesis in meiosis. Cell Cycle. 2016;15:471–7.
Brunet S, Verlhac MH. Positioning to get out of meiosis: the asymmetry of division. Hum Reprod Update. 2011;17:68–75.
Sanfins A, Lee GY, Plancha CE, Overstrom EW, Albertini DF. Distinctions in meiotic spindle structure and assembly during in vitro and in vivo maturation of mouse oocytes. Biol Reprod. 2003;69:2059–67.
Barrett SL, Albertini DF. Allocation of gamma-tubulin between oocyte cortex and meiotic spindle influences asymmetric cytokinesis in the mouse oocyte. Biol Reprod. 2007;76:949–57.
Combelles CMH, Albertini DF. Microtubule patterning during meiotic maturation in mouse oocytes is determined by cell cycle-specific sorting and redistribution of gamma-tubulin. Dev Biol. 2001;239:281–94.
Li R, Albertini DF. The road to maturation: somatic cell interaction and self-organization of the mammalian oocyte. Nat. Rev. Mol. Cell biol. Nat Publ Group. 2013;14:141–52.
Robinson DN. Cell division: biochemically controlled mechanics. Curr Biol. 2001;11:737–40.
Kloc M, Ghobrial RM, Borsuk E, Kubiak JZ. Polarity and asymmetry during mouse oogenesis and oocyte maturation. Mouse Dev. 2012:23–44.
Jo Y-J, Jang W-I, Namgoong S, Kim N-H. Actin-capping proteins play essential roles in the asymmetric division of maturing mouse oocytes. J Cell Sci. 2015;128:160–70.
Duan X, Zhang H, Pan M, Zhang Y, Sun S. Vesicular transport protein Arf6 modulates cytoskeleton dynamics for polar body extrusion in mouse oocyte meiosis. BBA Mol Cell Res. 2018;1865:455–62.
Duan X, Liu J, Dai X-X, Liu H-L, Cui X-S, Kim N-H, et al. Rho-GTPase effector ROCK phosphorylates cofilin in actin-meditated cytokinesis during mouse oocyte meiosis. Biol Reprod. 2014;90:1–9.
Lee SR, Xu YN, Jo YJ, Namgoong S, Kim NH. The rho-GTPase effector ROCK regulates meiotic maturation of the bovine oocyte via myosin light chain phosphorylation and cofilin phosphorylation. Mol Reprod Dev. 2015;82:849–58.
Wang F, Zhang L, Duan X, Zhang GL, Wang ZB, Wang Q, et al. RhoA-mediated FMNL1 regulates GM130 for actin assembly and phosphorylates MAPK for spindle formation in mouse oocyte meiosis. Cell Cycle. 2015;14:2835–43.
Wang QC, Liu J, Wang ZB, Zhang Y, Duan X, Cui XS, et al. Dynamin 2 regulates actin-mediated spindle migration in mouse oocytes. Biol Cell. 2014;106:193–202.
Jang WI, Jo YJ, Kim HC, Jia JL, Namgoong S, Kim NH. Non-muscle tropomyosin (Tpm3) is crucial for asymmetric cell division and maintenance of cortical integrity in mouse oocytes. Cell Cycle. 2014;13:2359–69.
Pan MH, Wang F, Lu Y, Tang F, Duan X, Zhang Y, et al. FHOD1 regulates cytoplasmic actin-based spindle migration for mouse oocyte asymmetric cell division. J Cell Physiol. 2018;233:2270–8.
Halet G, Carroll J. Rac activity is polarized and regulates meiotic spindle stability and anchoring in mammalian oocytes. Dev Cell. 2007;12:309–17.
De S, Marcinkiewicz JL, Vijayaraghavan S, Kline D. Expression of 14-3-3 protein isoforms in mouse oocytes, eggs and ovarian follicular development. BMC Res Notes. 2012;5:57.
Kolano A, Brunet S, Silk AD, Cleveland DW, Verlhac M-H. Error-prone mammalian female meiosis from silencing the spindle assembly checkpoint without normal interkinetochore tension. Proc Natl Acad Sci. 2012;109:E1858–67.
Lee Y, Kim KH, Yoon H, Lee OH, Kim E, Park M, et al. RASD1 knockdown results in failure of oocyte maturation. Cell Physiol Biochem. 2016;40:1289–302.
Hughesdon PE. Morphology and morphogenesis of the Stein–Leventhal ovary and of so-called “hyperthecosis.” Obstet Gynecol Surv 1982;37:59–77.
Hatzirodos N, Bayne RA, Irving-Rodgers HF, Hummitzsch K, Sabatier L, Lee S, et al. Linkage of regulators of TGF-activity in the fetal ovary to polycystic ovary syndrome. FASEB J. 2011;25:2256–65.
Mukherjee A, Sidis Y, Mahan A, Raher MJ, Xia Y, Rosen ED, et al. FSTL3 deletion reveals roles for TGF-beta family ligands in glucose and fat homeostasis in adults. Proc Natl Acad Sci U S A. 2007;104:1348–53.
Urbanek M, Sam S, Legro RS, Dunaif A. Identification of a polycystic ovary syndrome susceptibility variant in fibrillin-3 and association with a metabolic phenotype. J Clin Endocrinol Metab. 2007;92:4191–8.
D’Ascenzo S, Giusti I, Millimaggi D, Marci R, Tatone C, Colonna RC, et al. Intrafollicular expression of matrix metalloproteinases and their inhibitors in normally ovulating women compared with patients undergoing in vitro fertilization treatment. Eur J Endocrinol. 2004;151:87–91.
Tarkun I, Cantürk Z, Arslan BC, Türemen E, Tarkun P. The plasminogen activator system in young and lean women with polycystic ovary syndrome. Endocr J. 2004;51:467–72.
Kort J, Behr B. Biomechanics and developmental potential of oocytes and embryos. Fertil Steril. 2017;108:738–41.
Lai D, Takayama S, Smith GD. Recent microfluidic devices for studying gamete and embryo biomechanics. J Biomech Elsevier. 2015;48:1671–8.
Yanez LZ, Camarillo DB. Microfluidic analysis of oocyte and embryo biomechanical properties to improve outcomes in assisted reproductive technologies. Mol Hum Reprod. 2017;23:235–47.
He X. Microfluidic encapsulation of ovarian follicles for 3D culture. Ann Biomed Eng. 2017;45:1676–84.
Andolfi L, Masiero E, Giolo E, Martinelli M, Luppi S, dal Zilio S, et al. Investigating the mechanical properties of zona pellucida of whole human oocytes by atomic force spectroscopy. Integr Biol. 2016;8:886–93.
Kawashima I, Kawamura K. Disorganization of the germ cell pool leads to primary ovarian insufficiency. Reproduction. 2017;153:R205–13.
Yin O, Cayton K, Segars JH. In vitro activation: a dip into the primordial follicle pool? J Clin Endocrinol Metab. 2016;101:3568–70.
Novella-Maestre E, Herraiz S, Rodriguez-Iglesias B, Diaz-Garcia C, Pellicer A. Short-term PTEN inhibition improves in vitro activation of primordial follicles, preserves follicular viability, and restores AMH levels in cryopreserved ovarian tissue from Cancer patients. PLoS One. 2015;10:e0127786.
Suzuki N, Yoshioka N, Takae S, Sugishita Y, Tamura M, Hashimoto S, et al. Successful fertility preservation following ovarian tissue vitrification in patients with primary ovarian insufficiency. Hum Reprod. 2015;30:608–15.
Zhai J, Yao G, Dong F, Bu Z, Cheng Y, Sato Y, et al. In vitro activation of follicles and fresh tissue auto-transplantation in primary ovarian insufficiency patients. J Clin Endocrinol Metab. 2016;101:4405–12.
Acknowledgements
We would like to thank Janice P. Evans, PhD for her suggestions and edits of the manuscript and Jamie Blanck, MLIS, MPA, AHIP for her assistance with the systematic review query.
Funding
In part, by the Howard W. and Georgeanna Seegar Jones Endowment. C.O. was supported by the intramural research program of NICHD, ZIE HD-008737-14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Electronic supplementary material
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Shah, J.S., Sabouni, R., Cayton Vaught, K.C. et al. Biomechanics and mechanical signaling in the ovary: a systematic review. J Assist Reprod Genet 35, 1135–1148 (2018). https://doi.org/10.1007/s10815-018-1180-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1180-y