Abstract
Objective
To evaluate the relationship between different hCG priming-to-oocyte retrieval intervals and assisted reproductive technology (ART) outcome.
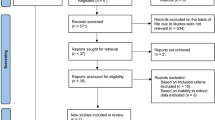
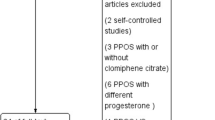
Methods
We systematically searched PubMed, EMBASE, the Cochrane Library, Science Citation Index, Chinese biomedicine (CBM) literature database, and Chinese Journal Full-text Database for randomized controlled trials (RCTs) published up to November 2010. Data was extracted from the studies by two independent reviewers. Statistical analysis was performed with Cochrane Collaboration’s Review Manager (RevMan) 5.0.2. From extracted data, Risk Ratio (RR) with 95% confidence interval (CI) was calculated.
Results
5 RCTs totaling 895 participants were included. Oocyte maturation rate was higher in the long interval group compared with short interval group (RR, 0.67; 95% CI, 0.62–0.73). There were no significant difference between the two groups with regard to fertilization rate (RR, 0.99; 95% CI, 0.94–1.04), implantation rate (RR, 0.91; 95% CI, 0.40–2.04), and pregnancy rate (RR, 0.79; 95% CI, 0.58–1.08).
Conclusion
The percentage of mature (MII) oocytes can be increased by prolonging the interval between hCG priming and oocyte retrieval. The prolonged interval could not increase the fertilization rate, implantation rate, and pregnancy rate. Although there was evidence to confirm the results, they still need to be confirmed by large-sample, multicenter, randomized controlled trials. The time interval dependent mechanisms responsible for ART performance need to be elucidated.






Similar content being viewed by others
Abbreviations
- ART:
-
Assisted reproductive technology
- ATP:
-
Adenosine triphosphate
- CC:
-
Clomiphene citrate
- COH:
-
Controlled ovarian hyperstimulation
- ET:
-
Embryo transfer
- FSH:
-
Follicle-stimulating hormone
- GnRH-a:
-
Gonadotropic hormone releasing hormone analogue
- hCG:
-
Human chorionic gonadotropin
- hMG:
-
Human menopausal gonadotropin
- ICSI:
-
Intracytoplasmic sperm injection
- IGF:
-
Insulin-like growth factor
- IL:
-
Interleukin
- IM:
-
Intramuscular injection
- IUI:
-
Intrauterine insemination
- IVF:
-
In vitro fertilization
- IVM:
-
In vitro maturation
- LH:
-
Luteinizing hormone
- LI:
-
Long interval
- MII:
-
Metaphase II
- NA:
-
Not available
- RCT:
-
Randomized controlled trial
- RevMan:
-
Review Manager
- RR:
-
Risk ratio
- SI:
-
Short interval
- TUS:
-
Transvaginal ultrasound
- VEGF:
-
Vascular endothelial growth factor
- 2PN:
-
Two-pronuclear
- 95% CI:
-
95% confidence interval
References
Griesinger G, Kolibianakis EM, Papanikolaou EG, Diedrich K, Van Steirteghem A, Devroey P, et al. Triggering of final oocyte maturation with gonadotropin-releasing hormone agonist or human chorionic gonadotropin. Live birth after frozen-thawed embryo replacement cycles. Fertil Steril. 2007;88:616–21.
Gudmundsson J, Fleming R, Jamieson ME, McQueen D, Coutts JRT. Luteinization to oocyte retrieval delay in women in whom multiple follicular growth was induced as part of an in vitro fertilization/gamete intrafallopian transfer program. Fertil Steril. 1990;53:735–7.
Kuo TC, Endo K, Dharmarajan AM, Miyazaki T, Atlas SJ, Wallach EE. Direct effect of angiotensin II on in-vitro perfused rabbit ovary. J Reprod Fertil. 1991;92:469–74.
Artini PG, Fasciani A, Monti M, Luisi S, D’Ambrogio G, Genazzani AR. Changes in vascular endothelial growth factor levels and the risk of ovarian hyperstimulation syndrome in women enrolled in an in vitro fertilization program. Fertil Steril. 1998;70:560–4.
Bokal EV, Vrtovec HM, Virant Klun I, Verdenik I. Prolonged HCG action affects angiogenic substances and improves follicular maturation, oocyte quality and fertilization competence in patients with polycystic ovarian syndrome. Hum Reprod. 2005;20:1562–8.
Artini PG, Monti M, Fasciani A, Battaglia C, D’Ambrogio G, Genazzani AR. Vascular endothelial growth factor, interleukin-6 and interleukin-2 in serum and follicular fluid of patients with ovarian hyperstimulation syndrome. Eur J Obstet Gynecol Reprod Biol. 2002;101:169–74.
World Health Organization. Temporal relationships between ovulation and defined changes in the concentration of plasma oE2–17β, luteinizing hormone, follicle stimulating hormone and progesterone. Am J Obstet Gynecol. 1980;138:383–90.
Nader S, Berkowitz AS. Study of the pharmacokinetics of human chorionic gonadotropin and its relation to ovulation. In Vitro Fert Embryo Transfer. 1990;7:114–8.
Edwards RG, Steptoe PC. Induction of follicular growth, ovulation and luteinization in the human ovary. J Reprod Fertil. 1975;22(Suppl):121–63.
Testart J, Frydman R. Minimum time lapse between luteinizing hormone surge or human chorionic gonadotropin administration and follicular rupture. Fertil Steril. 1982;37:50–3.
Trounson AO, Leeton JF, Wood C. In vitro fertilization and embryo transfer in the human. In: Rolland R, van Hall EV, Hillier SG, Mcnatty KP, Schoemaker J, editors. Follicular maturation and ovulation. Amsterdam, Exerpta Medica 1982:313
De Vits A, Gerris J, Joostens M, Aytos A. Comparison between two hCG-to-oocyte aspiration intervals (36 versus 38) on the outcome of in-vitro fertilization. Hum Reprod. 1994;9(Suppl):12–5.
Mansour RT, Aboulghar MA, Serour GI. Study of the optimum time for human chorionic gonadotropin-ovum pickup interval in in vitro fertilization. J Assist Reprod Genet. 1994;11:478–81.
Fleming R, Coutts JRT. Induction of multiple follicular development for IVF. Brit Med Bull. 1990;46:596–615.
Al-Mizyen ES, Balet R, Lower AM, Wilson C, McClure AF, Al Shawaf T, et al. Unexpected successful fertilization in vitro of oocytes retrieved 60 hours after human chorionic gonadotrophin injection. Hum Reprod. 1998;13:1020–1.
Nargund G, Reid F, Parsons J. Human chorionic gonadotropin-to-oocyte collection interval in a superovulation IVF program. A prospective study. J Assist Reprod Genet. 2001;18:87–90.
Bjercke S, Tanbo T, Dale PO, Abyholm T. Comparison between two hCG-to-oocyte aspiration intervals on the outcome of in vitro fertilization. J Assist Reprod Genet. 2000;17:319–22.
Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions 5.0.0 [updated February 2008]. In: The Cochrane collaboration. Wiley 2008.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Claman P, Wilkie V, Collins D. A short (335 h) compared with a long (395 h) interval between HCG injection and intrauterine insemination after superovulation therapy. Hum Reprod. 2000;15:6–7.
Claman P, Wilkie V, Collins D. Timing intrauterine insemination either 33 or 39 hours after administration of human chorionic gonadotropin yields the same pregnancy rates as after superovulation therapy. Fertil Steril. 2004;82:13–6.
Fischer RA, Nakajima ST, Gibson M, Brumsted JR. Ovulation after intravenous and intramuscular human chorionic gonadotropin. Fertil Steril. 1993;60:418–22.
Howles CM, Macnamee MC, Edwards RG. Progesterone supplementation in the late follicular phase of an in-vitro fertilization cycle: a ‘natural’ way to time oocyte recovery? Hum Reprod. 1988;3:409–12.
Laufer N, DeCherney AH, Tarlatzis BC, Zuckerman AL, Polan ML, Dlugi AM, et al. Delaying human chorionic gonadotropin administration in human menopausal gonadotropin-induced cycles decreases successful in vitro fertilization of human oocytes. Fertil Steril. 1984;42:198–203.
Templeton AA, Van Look P, Angell RE, et al. Oocyte recovery and fertilization rates in women at various times after the administration of hCG. J Reprod Fertil. 1986;76:771–8.
Schachter M, Friedler S, Ron-El R, Zimmerman AL, Strassburger D, Bern O, et al. Can pregnancy rate be improved in gonadotropin-releasing hormone (GnRH) antagonist cycles by administering GnRH agonist before oocyte retrieval? A prospective, randomized study. Fertil Steril. 2008;90:1087–93.
Raziel A, Schachter M, Strassburger D, Kasterstein E, Ron-El R, Friedler S. In vivo maturation of oocytes by extending the interval between human chorionic gonadotropin administration and oocyte retrieval. Fertil Steril. 2006;86:583–7.
Jamieson ME, Fleming R, Kader S, Ross KS, Yates RW, Coutts JR. In vivo and in vitro maturation of human oocytes: effects on embryo development and polyspermic fertilization. Fertil Steril. 1991;56:93–7.
Schmidt DW, Maier DB, Nulsen JC, Benadiva CA. Reducing the dose of human chorionic gonadotropin in high responders does not affect the outcomes of in vitro fertilization. Fertil Steril. 2004;82:841–6.
Isik AZ, Vicdan K. Combined approach as an effective method in the prevention of severe ovarian hyperstimulation syndrome. Eur J Obstet Gynecol Reprod Biol. 2001;97:208–12.
Jagiello G, Karniki J, Ryan R. Superovulaton with pituitary gonadotropin methods for obtaining meiotic metaphase figures in human ova. Lancet. 1968;1:178–80.
Van Steirteghem AC, Liu J, Joris H, Nagy Z, Janssenswillen C, Tournaye H, et al. Higher success rate by intracytoplasmic sperm injection than by subzonal insemination. Report of a second series of 300 consecutive treatment cycles. Hum Reprod. 1993;8:1055–60.
Steptoe PC, Edwards RG. Laparoscopic recovery of preovulatory human oocytes after priming of ovaries with gonadotrophins. Lancet. 1970;1:683–9.
Edwards RG, Steptoe PC. Control of human ovulation, fertilization and implantation. Proc R Soc Med. 1974;67:932–6.
Andersen AG, Als-Nielsen B, Hornnes PJ, Franch Andersen L. Time interval from human chorionic gonadotrophin (HCG) injection to follicular rupture. Hum Reprod. 1995;10:3202–5.
Trounson A, Wood C, Kausche A. In vitro maturation and the fertilization and developmental competence of oocytes recovered from untreated polycystic ovarian patients. Fertil Steril. 1994;62:353–62.
Son WY, Chung JT, Chian RC, Herrero B, Demirtas E, Elizur S, et al. A 38 h interval between hCG priming and oocyte retrieval increases in vivo and in vitro oocyte maturation rate in programmed IVM cycles. Hum Reprod. 2008;23:2010–6.
Hull MG, Fleming CF, Hughes AO, McDermott A. The age-related decline in female fecundity: a quantitative controlled study of implanting capacity and survival of individual embryos after in vitro fertilization. Fertil Steril. 1996;65:783–90.
Schnorr JA, Doviak MJ, Muasher SJ, Jones Jr HW. Impact of a cryopreservation program on the multiple pregnancy rate associated with assisted reproductive technologies. Fertil Steril. 2001;75:147–51.
Thurin A, Hausken J, Hillensjo T, Jablonowska B, Pinborg A, Strandell A, et al. Elective single-embryo transfer versus double-embryo transfer in in vitro fertilization. N Engl J Med. 2004;351:2392–402.
Lukassen HGM, Braat DD, Wetzels AMM, Zielhuis GA, Adang EMM, Scheenjes E, et al. Two cycles with single embryo transfer versus one cycle with double embryo transfer: a randomized controlled trial. Hum Reprod. 2005;20:702–8.
Veleva Z, Vilska S, Hyden-Granskog C, Tiitinen A, Tapanainen JS, Martikainen H. Elective single embryo transfer in women aged 36–39 years. Hum Reprod. 2006;21:2098–102.
Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G, et al. Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod. 1999;14:2345–9.
Roux C, Joanne C, Agnani G, Fromm M, Clavequin MC, Bresson JL. Morphometric parameters of living human in-vitro fertilization embryos; importance of the asynchronous division process. Hum Reprod. 1995;10:1201–7.
Hiiragi T, Solter D. Mechanism of first cleavage specification in the mouse egg: is our body plan set at day 0? Cell Cycle. 2005;4:661–4.
Gardner RL, Davies TJ. An investigation of the origin and significance of bilateral symmetry of the pronuclear zygote in the mouse. Hum Reprod. 2006;21:492–502.
Racowsky C, Jackson KV, Cekleniak NA, Fox JH, Hornstein MD, Ginsburg ES. The number of eight-cell embryos is a key determinant for selecting day 3 or day 5 transfer. Fertil Steril. 2000;73:558–64.
Scott L, Finn A, O’Leary T, McLellan S, Hill J. Morphologic parameters of early cleavage-stage embryos that correlate with fetal development and delivery: prospective and applied data for increased pregnancy rates. Hum Reprod. 2007;22:230–40.
Acknowledgments
The authors would like to thank Jin-Hui Tian, Bin Ma, Lei Jiang, Wen-Qin Jia, Kang Yi, and Lun Li (Evidence-Based Medicine Center of Lanzhou University, Lanzhou, China) for advice on conducting the meta-analysis and writing the article.
Conflicts of interest statement
The authors declared no conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Capsule In ART treatment cycles, the chances to achieve a pregnancy are critically dependent on the retrieval of a suitable number of high quality oocytes and embryos. Angiotensin II, vascular endothelial growth factor (VEGF), interleukin I (IL-1), IL-6, IL-8, angiopoietin, insulin-like growth factor (IGF), basic fibroblast growth factor (bFGF), and endothelin levels appear able to identify women candidate for an ART treatment from whom a suitable number of high quality oocytes may be retrieved.
Rights and permissions
About this article
Cite this article
Wang, W., Zhang, XH., Wang, WH. et al. The time interval between hCG priming and oocyte retrieval in ART program: a meta-analysis. J Assist Reprod Genet 28, 901–910 (2011). https://doi.org/10.1007/s10815-011-9613-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-011-9613-x